What is COVID-19?
COVID-19 is a new coronavirus that is rapidly spreading throughout the world. According to the WHO, it is classified as a pandemic. Most people (80%) experience mild symptoms, although the virus is most harmful to seniors (over 65 years of age) and people with compromised immune systems (e.g., with cancer, chronic inflammatory conditions like rheumatoid arthritis) and pre-existing medical conditions (e.g., cardiovascular disease, uncontrolled hypertension or diabetes, and chronic lung diseases).
How is COVID-19 transmitted?
Similar to seasonal flu, people can get infected with COVID-19 if they inhale water droplets containing the virus, such as when someone sneezes on them, or by touching a surface contaminated by the virus (e.g., a hand-railing) and then touching their nose or mouth or rubbing their eyes.
What should you do if you think you have COVID-19?
The following symptoms may appear 2-14 days after exposure.
If you think you have been exposed to COVID-19 or if you develop symptoms (e.g., a fever or respiratory symptoms like such as cough or difficulty breathing), isolate yourself, stay home and call your healthcare provider and/or local health authority immediately (see: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/2019-novel-coronavirus-information-sheet.html#pha). You will be asked to describe your symptoms and travel history. They will advise you on how to get tested and/or treatment.
If you are sick with COVID-19 or suspect you are infected with the virus that causes COVID-19, follow the steps below, as outlined by the Public Health Agency of Canada (PHAC) and the Centers for Disease Control (CDC), to help prevent the disease from spreading to people in your home and community.
- Stay home (except to get medical care in case of symptom deterioration)
- Avoid using any form of public transportation
- Separate yourself from other people and animals in your home
- Wear a facemask if you are sick (wearing masks does not protect you from others who may be sick)
- Cough and sneeze into your arm or elbow
- Immediately dispose of used tissues
- Clean your hands often
- Avoid sharing personal household items (particularly towels)
- Clean all “high-touch” surfaces every day
- Monitor your symptoms and seek prompt medical attention if your illness is worsening (e.g., difficulty breathing)
- Call ahead before visiting your doctor
What is the best way to keep safe?
Currently, there is no vaccine for COVID-19. Human behaviour is key to the spread of COVID-19, and behavioural strategies may help to reduce transmission. The best way of protecting yourself is to wash your hands regularly with soap and water before and after meals and after touching ‘public’ surfaces (like doorknobs or handles). Keep your hands away from your face and cover your coughs and sneezes (e.g., coughing into your arm). The recommended way of doing these things may be different than how you are used to doing them. Using evidence-based behavioral strategies may help you adapt your daily routines to keep you safer:
- Up-skill how you wash your hands: Washing our hands is often part of our daily routines already, but to be effective in preventing transmission of the virus, most of us probably need to wash our hands better and for longer:
- Make sure you have soap or alcohol-based* hand sanitizer available; if you’re worried about dry hands, bring moisturiser with you (*alcohol content should be 60% or higher)
- Wash your hands for at least 20 seconds. Humming a song (e.g. happy birthday) that lasts that long may help with timing. (“If I’m washing my hands, I will hum happy birthday!”)
- Put soap on the back and front of your hands, under your nails and between your fingers
- Make it more salient: consider making it more memorable by telling yourself “when washing my hands, I will wash them as if I just cut up a jalapeno and need to take out my contact lenses!”
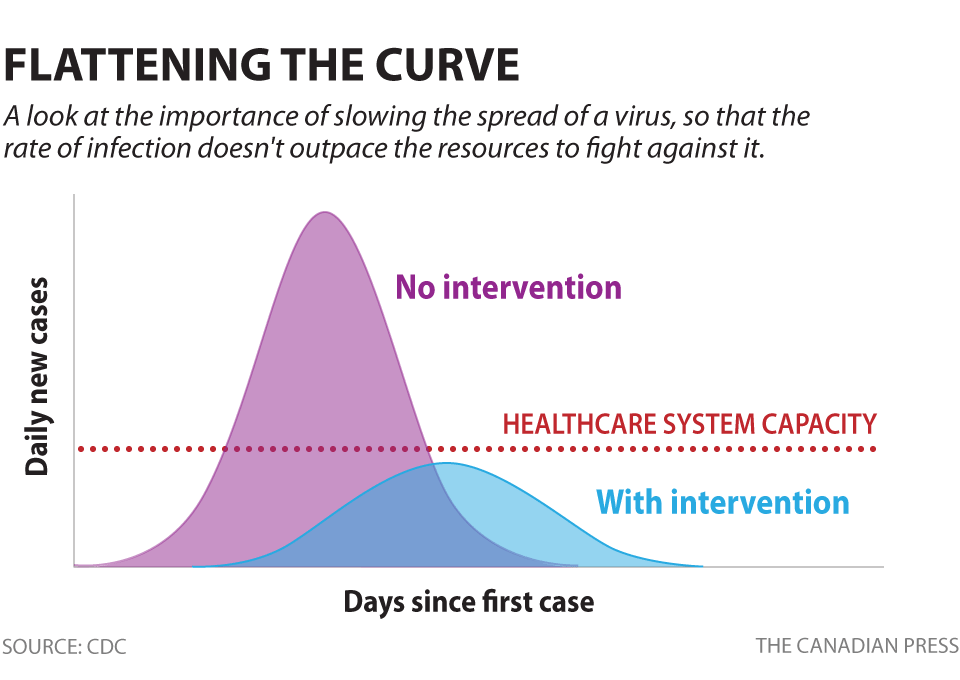
- Social Distancing: Social distancing is a term applied to certain actions that are taken by Public Health officials to stop or slow down the spread of a highly contagious disease, and ensure our public health system can continue to meet the demands placed on it. The figure below depicts the critical role that social distancing can play to reduce the spread in a short period of time. Social distancing is one of the most effective measures for reducing the overall speed of transmission, to protect and preserve the capacity of the healthcare system to care for severe cases. Social distancing is specific to limiting physical/in-person connections. It is important to stay connected to each other through other means to maintain our connections and support one another (email, phone, social media)

Social distancing measures include limiting large groups of people coming together, closing buildings, and canceling events. Examples of social distancing measures can include: suspending classes in or closing schools, modifying hours of operations for services, changing workplace practices to allow flexible shift plans and tele-work, closing theatres, cancelling large scale indoor and outdoor events (e.g. sporting events, concerts, parades, festivals), and suspending or limiting transportation means. - Am I really touching my face that much? Yes! To be transmitted, COVID-19 needs access, and that is usually through your nose, mouth or eyes. Over the course of the day, most people touch their face a few dozen times, often without realizing it. Potentially effective behavioural strategies to stop touching your face are:
- Use ‘if-then’ plans to ‘program’ that automatic part of your brain to be more aware of when you touch your face to curb this behaviour. For example, “If I find myself resting my hand on my chin, I will remind myself that I want to stop the spread of COVID-19”.
- Ask your family/friends/coworkers to monitor and give you feedback on how often you touch your face without realizing it; make a game out of it to track each other, aiming to touch your face less. You might be amazed at how often you touch your face without realizing it.
- Replace handshakes and kissing cheeks: Shaking hands and kissing cheeks are common ways of greeting in Canadian society. Developing alternative ways of friendly connection during the COVID-19 outbreak. Bumping feet, elbows, or bowing could avoid transmission while maintaining our important social connections. While initially a bit awkward, explaining why may help to normalize it.
- Restrict all non-essential travel until further notice:
- Canada’s chief public health officer, Dr. Theresa Tam, is advising all Canadians to postpone or cancel all non-essential travel outside of Canada until further notice.
- If you plan to travel, stay informed of Canadian travel advisories as well as those for your travel destination.
- If you are flying, confirm travel policies and restrictions with your airline (this includes ensuring return or alternate flights can be secured should flight restrictions change).
- Ensure you have appropriate health and travel insurance – including cancellation insurance ‘for any reason’.
- When considering whether or not to travel, keep in mind that local and foreign travel restrictions and border controls are changing everyday. If you do decide to travel, be aware that borders could close at any time and you may be forced to extend your stay.
- Get the vaccine once it becomes available: Current estimates by the World Health Organization (WHO) are that developing a vaccine is at least 18 months away. When a vaccine is made available, it is important to make the time to get vaccinated for yourself, as well as for those who can’t be vaccinated due to medical and other reasons. We can help everyone stay safe if all of us get vaccinated, because we won’t spread infection. This is called “herd immunity.” When it comes to vaccination, ensuring the greatest amount of community coverage is key for optimal prevention and protection of vulnerable populations (seniors, those with health conditions).
Psychological reactions to COVID-19: Why are they important?
Psychological factors play an important role in how people and communities respond to illness and manage its spread.
Some people under-respond to the threat of COVID-19. These people think the danger is exaggerated. Under-responders may not practice good hygiene, they don’t get vaccinated, and they don’t stay home if they’re sick; these behaviours help infection to spread. To accurately assess the risks of COVID-19, check out the websites of the PHAC, WHO or CDC (see below for links to updated resources). Under-responding could spread infection to family and friends.
Some people over-respond to the threat of COVID-19. These people become highly anxious about the infection and may go to great lengths to keep themselves safe. They may become xenophobic (i.e., needlessly frightened of foreign people), may needlessly wear protective masks (while wearing a mask may prevent you from spreading your infection to others, masks are not effective in preventing you from catching an infection from someone else), and may hoard supplies of food and other necessities. Over-responding by one person seeds fear in others because fear is contagious, so the more you see people buying toilet paper makes you believe that toilet paper may run out, leading you to rush out and stock up (needlessly). Moreover, if you hoard food, toilet paper, or hand sanitizer that you are not likely to need for example, then other people in your community have less access to them.
What can people do to stay calm but remain appropriately vigilant?
- Listen to the advice of health authorities such as PHAC, the WHO and CDC for more local information about if/how COVID-19 is spreading in your area. See resources below.
- Change your habits around washing hands, touching your face, socializing and coughing – see behavioural strategies above.
- Some degree of concern is reasonable if it leads you to be proactive and take appropriate precautions, like staying home or social distancing, hand washing and sanitizing, and refraining from unnecessary travel. Otherwise, you should feel confident about carrying on with your everyday life as usual, with some minor adaptations. For example, if you typically go to the gym for your workout, consider going for a walk or a run in your neighborhood. If you go to a restaurant, skip the buffet and order a la carte. As long as there is no evidence of ‘community transmission’ (which is transmission of the virus from person to person through community contact rather than contracting it through travel), you should feel confident about maintaining several aspects of your routine, including going out.
- Keep things in perspective by consulting sources of information that are balanced and evidence-based, such as the PHAC, the WHO, and other credible sources (see links below). Remind yourself that the graphic images on the Internet, or the rumors on social media, may exaggerate the actual threat. The images of empty shelves in supermarkets are compelling visuals but are not necessarily common and may be confined to certain areas. No one is posting images of full shelves and calm shoppers because those images aren’t newsworthy. If you feel anxious when following news media or social media, limit your exposure.
- Fear is contagious. If you act frightened or engage in panic buying, then others will react with fear as well. You have a responsibility to your loved ones, friends, and the rest of the community to deal with the COVID-19 outbreak in a sensible, reasoned manner. Try to “lead by example”.
- Remind yourself that the current crisis will pass, and life will return to normal.
Where can I get more information?
- Further advice for behavioural strategies to reduce transmission: https://blogs.bmj.com/bmj/2020/03/03/behavioural-strategies-for-reducing-covid-19-transmission-in-the-general-population/
- Up to date case tracking worldwide and in Canada using Johns Hopkins interactive tracker: https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
- Guidance that is regularly updated from trusted sources:
- Public Health Agency of Canada: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html
- World Health Organization: https://www.who.int/health-topics/coronavirus
- US Centres for Disease Control and Prevention: https://www.cdc.gov/coronavirus/2019-ncov/
- The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. By S. Taylor (2019). Newcastle upon Tyne: Cambridge Scholars Publishing.
- It’s Not All in Your Head: How Worrying About Your Health Could be Making You Sick – and What You Can Do About It. By G.J.G. Asmundson & S. Taylor (2004). New York: Guilford Press.
How can I tell whether I should seek professional help for COVID-19-related stress or anxiety?
Look for warning signs such as the following:
- Persistent anxiety, worry, insomnia, or irritability.
- Needlessly avoiding social contacts to the point that you become unnecessarily isolated.
- Persistently checking your body (e.g., taking your temperature many times each day) or persistently seeking reassurance about your health from doctors, friends, family, or the Internet.
- Performing excessive or unnecessary hygiene precautions, such as wearing a facemask at home or repeatedly washing your hands when there is no need to do so.
- Abusing alcohol or drugs, or overeating, as a way of coping with stress.
- Feedback from friends or family that you seem unusually worried or stressed out.
How can I get help with stress or anxiety? Psychological treatments can be very effective, sometimes more effective than medication, in helping people recover from anxiety. To find a psychologist, you can consult the psychological association in your province or city. A list of them can be found at https://cpa.ca/public/whatisapsychologist/PTassociations. Your local hospital, community health clinic, local public health department, or primary care provider (e.g., family doctor or nurse practitioner) may also be of assistance.
This fact sheet has been prepared for the Canadian Psychological Association by Steven Taylor, Ph.D., R.Psych., Department of Psychiatry, University of British Columbia, Kim Lavoie, Ph.D., FCPA, FABMR, Montreal Behavioral Medicine Center (MBMC) and Department of Psychology, University of Quebec at Montreal (UQAM), and Justin Presseau, Ph.D., Clinical Epidemiology Program (Ottawa Hospital Research Institute), and School of Psychology and School of Epidemiology and Public Health (University of Ottawa).
Prepared: March 12, 2020
Updated: March 13, 2020
Your opinion matters! Please contact us with any questions or comments about any of the Psychology Works Fact Sheets: factsheets@cpa.ca
Canadian Psychological Association
141 Laurier Avenue West, Suite 702
Ottawa, Ontario K1P 5J3
Tel: 613-237-2144
Toll free (in Canada): 1-888-472-0657
[i] https://www.cdc.gov/coronavirus/2019-ncov/about/index.html
[ii] https://www.cdc.gov/coronavirus/2019-ncov/about/steps-when-sick.html