Infectious diseases, like any life stressor, challenge the way we cope. Whether we learn about them on television or experience them personally, we can feel upset, fearful and anxious as a result, both for our own personal safety and that of our family, friends, colleagues, and community. Stressful events can also bring up feelings and memories of previous traumatic events thereby compounding the distress that we feel.
The Novel Coronavirus (COVID-19) is one such infectious illness that currently poses significant risk to public health and we are all challenged by it. It is important to remember that it is normal to be emotionally affected by events like wide-spread illnesses, and that there are steps we can take to help us cope.
The information that follows is intended to help people cope psychologically in the face of health risks like COVID-19. It does not convey important information that you should know about how the virus is contracted, its signs and symptoms, how to decrease your risk of contracting the virus and how the virus is treated. For important and up to date information about COVID-19 visit the Public Health Agency of Canada (PHAC) website at https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html
While people vary in their response to a crisis, for one like COVID-19, it is likely that more people will see impacts on their mental health and well being than will suffer serious physical effects of the illness. People who may respond more strongly to the stress of a crisis include:
- Older people and people with chronic diseases who are at higher risk for COVID-19
- Children and teens
- People who are helping with the response to COVID-19, like doctors, nurses, and other health care providers, or first responders
- People who have mental health conditions including problems with substance use
- People who tend to worry – particularly about their health, or who have experienced a previous or recent traumatic event
- People who live alone or have few social supports
Assessing and Coping with Risk
Stress during an infectious disease outbreak can include:
- Fear and worry about your own health and the health of your loved ones
- Changes in sleep or eating patterns
- Difficulty sleeping or concentrating
- Worsening of chronic health problems
- Increased use of alcohol, tobacco, or other drugs
Taking care of yourself, your friends, and your family can help you cope with stress and helps to make your community stronger. Coping strategies can include:
- Staying informed and taking guidance from experts to help you most accurately assess your personal risk of getting physically sick. Consulting expert sources such as infectious disease practitioners, family physicians or nurse practitioners, public health hotlines, or government websites (such as Health Canada, Public Health Agency of Canada, Centre for Disease Control, and the World Health Organization) for information.[1]
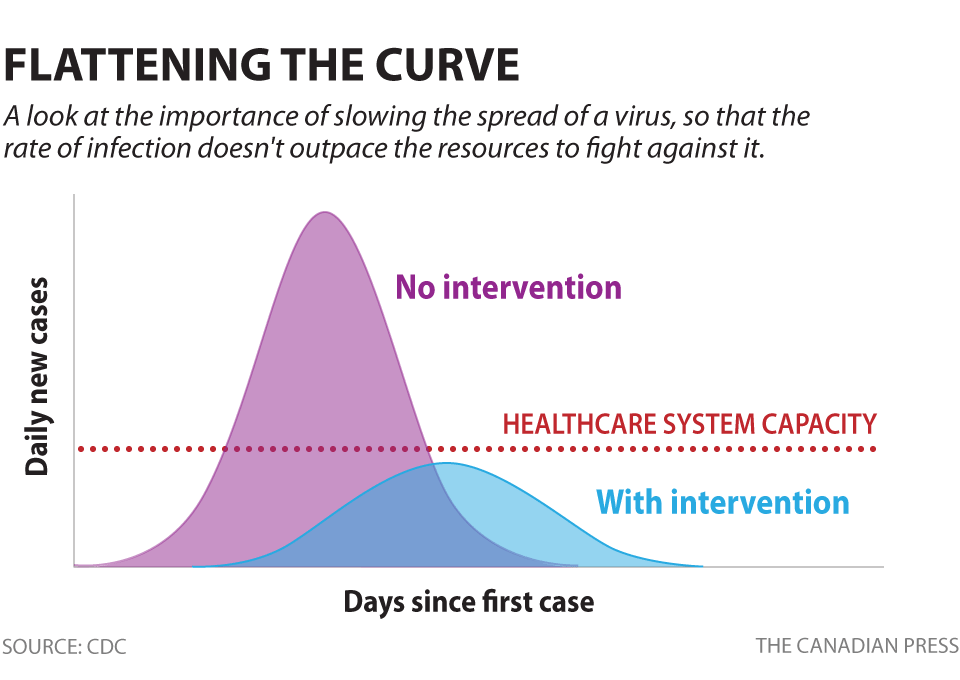
- Following the health and safety guidelines of such agencies as the Public Health Agency of Canada and Health Canada to minimize your risk of contracting the virus. Remembering that the media reports things that go wrong, or exceptional events, more often than things that go right, or common events. We hear about and pay more attention to the few people who might have been made very sick or who have died from an illness than we do about the many more people who have successfully recovered from an illness.
- Balancing gathering information and heeding safety guidelines to reduce risk with not letting the gathering of information or the attention to safety guidelines unduly preoccupy you.
Things to Keep in Mind about Stress
It is important to remember that:
- People are strong and resilient, and generally have the skills they need to cope with the stressors they will face in a lifetime.
- Not everyone reacts to the same event in the same way and not everyone shows their distress in the same way.
- The ways in which children and communities cope and react to a stressor are influenced by how they see parents, caregivers and community leaders cope and react.
Taking Care under Times of Stress
Taking care of yourself:
- Hearing about the pandemic repeatedly can be upsetting, so take breaks from watching, reading, or listening to news stories, including social media.
- Take care of your body. Take deep breaths, stretch, or meditate. Try to eat healthy, well-balanced meals, exercise regularly, get plenty of sleep, and avoid alcohol and drugs.
- Connect with others. Talk with people you trust about your concerns and how you are feeling – even when engaging in social distancing.
- Maintain as normal a routine as possible, including engaging in activities you enjoy.
- Call a health or mental health care provider if stress gets in the way of your daily activities for several days in a row.
Taking care of your family:
The threat of illness can be particularly upsetting to children and teens. Children and teens react, in part, to what they see from the adults around them. When parents and caregivers deal with the COVID-19 calmly and confidently, they can provide the best support for their children.
There are many things you can do to support your child or teen
- Given them the opportunity to talk about their concerns about the outbreak, tell them the truth, reassure them, and let them know they can count on you.
- Let them know it is ok if they feel upset or scared and talk to them about ways to cope with their feelings.
- Limit your family’s exposure to news coverage of the event, including social media.
- Try to keep up with regular routines to the extent possible. If schools are closed, create a schedule for learning activities and relaxing or fun activities; if organized activities are cancelled, try to engage in the activity (or an adaptation of the activity) at home.
If you notice that your child or teen’s behaviour has changed significantly, discuss the situation with them. Behavioural changes such as the ones below might also suggest a need to contact a regulated health care professional for additional help.
- Excessive crying or irritation in younger children
- Returning to behaviors they have outgrown (for example, toileting accidents or bedwetting)
- Changes in sleeping patterns (too much or too little) or appetite (eating too much or too little)
- Excessive worry or sadness
- Unhealthy eating or sleeping habits
- Irritability and “acting out” behaviors in teens
- Poor school performance or avoiding school
- Difficulty with attention and concentration
- Avoidance of activities enjoyed in the past
- Unexplained headaches or body pain
- Use of alcohol, tobacco, or other drugs
Taking care of people impacted by quarantine
Quarantine – or isolation from others for a period of time – is an important public health tool used to prevent those who are infected or who may be infected from infecting others. It involves being confined to your residence, with little or no direct contact with other people. Not surprisingly, almost everyone finds this to be upsetting, albeit to varying degrees.
During quarantine, it is important to maintain a connection with the outside world. This can be done by using the telephone, the Internet and social media. Although it may not be as good as seeing people face to face, it allows you to maintain meaningful contact with people.
When coming out of quarantine, people may experience different feelings, including:
- Mixed emotions, particularly relief
- Fear and worry about your own health and the health of your loved ones
- Stress from the experience of monitoring yourself or being monitored by others for signs and symptoms of COVID-19
- Sadness, anger, or frustration because friends or loved ones may have unfounded fears of contracting the disease from contact with you, even though you have been determined not to be contagious
- Guilt about not being able to perform normal work or parenting duties during quarantine
- Other emotional or mental health changes
For friends and loved ones of people in quarantine, although your contact with someone in quarantine may be significantly reduced, it is important to be reassuring and listen in a compassionate way. Contact him/her as often as is appropriate, thereby limiting their feelings of isolation. Talk to other people you trust about how you feel in response to the situation.
Most people will be able to handle quarantine without serious difficulty; however, some may have some significant mental health problems coping while in quarantine or when released. If this is the case, consult a regulated) health professional with mental health expertise who can assess the situation and provide the necessary care.
When Psychological Distress Becomes Too Much
Stressors such as the risk of illness associated with a pandemic will affect people differently. We can be affected psychologically (e.g., feeling worried), as well as physically (e.g., sleeping poorly). Stressors that are beyond our personal control are especially difficult to cope with well. Signs and symptoms that might signal a psychological problem or disorder for which professional help might be beneficial include:
- Sleeping poorly, too much or too little
- Avoiding others, even within the confines of social distancing
- Experiencing headaches, stomach problems, neck or back pain
- Crying
- Talking less
- Feeling anxious, depressed or having panic attacks
- Feeling angry, guilty, helpless, numb, or confused
- Thinking about or watching too much television on COVID-19 or pandemics
- Not wanting to get out of bed
- Having difficulties concentrating
- Excessive eating
- Drinking more alcohol or taking more prescription drugs
- Having little patience
- Feeling overprotective of loved ones
It is important to remember that most of us have had some of the signs and symptoms listed above at one time or another, and that COVID-19 has led to increased stress for most people. If you have a number of these signs and symptoms and they
- persist beyond a couple of weeks
- persist to the point where you are not able to carry out the home or work-related activities permitted by social distancing advisories
- are accompanied by intense feelings of despair or helplessness or suicidal thoughts
you are well advised to consult a regulated health care professional such as a psychologist, your family physician, a nurse practitioner, psychiatrist, or other mental health provider.
Where do I go for more information?
You can consult with a registered psychologist to find out if psychological interventions might be of help to you. Provincial, territorial, and some municipal associations of psychology often maintain referral services. For the names and coordinates of provincial and territorial associations of psychology, please visit: https://cpa.ca/public/whatisapsychologist/PTassociations
This fact sheet has been prepared for the Canadian Psychological Association by Dr. Lisa Votta-Bleeker, Deputy CEO, Canadian Psychological Association.
Date: March 20, 2020
Your opinion matters! Please contact us with any questions or comments about any of the Psychology Works Fact Sheets: factsheets@cpa.ca
Canadian Psychological Association
Tel: 613-237-2144
Toll free (in Canada): 1-888-472-0657
[1] https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html; https://www.cdc.gov/coronavirus/2019-ncov/index.html; https://www.who.int/

 Meghan Norris: The Canadian Handbook for Careers in Psychological Science
Meghan Norris: The Canadian Handbook for Careers in Psychological Science
 Leanna Verrucci
Leanna Verrucci Leigh Greiner
Leigh Greiner Marais Bester
Marais Bester Natalie Jones
Natalie Jones Jen Welter
Jen Welter Eva Best
Eva Best Lauren Florko
Lauren Florko Heather Orpana
Heather Orpana Gregory Craig
Gregory Craig Alexandra Thompson
Alexandra Thompson Robin Langerak
Robin Langerak Suzanne Simpson
Suzanne Simpson Chrissy Chubala
Chrissy Chubala Amy Bucher
Amy Bucher Liane Davey
Liane Davey
 Angela Febbraro
Angela Febbraro Amanda Parriag
Amanda Parriag Anne-Marie Côté
Anne-Marie Côté Susan Underhill
Susan Underhill Sophie Kenny
Sophie Kenny Troy Forcier
Troy Forcier Natalie Therrien Normand
Natalie Therrien Normand Sandra Meeres
Sandra Meeres Jenn Richler
Jenn Richler Christina Bilczuk
Christina Bilczuk Marc-André Lafrenière
Marc-André Lafrenière Evangeline Danseco
Evangeline Danseco Jennifer Veitch
Jennifer Veitch