What is acute pain?
Acute pain is typically described as a mild to intense sharp pain. It comes on quickly and lasts for a short period of time, usually providing a signal to the body that something is wrong. Experiencing acute pain is important because it is a part of our body’s built-in warning system. The experience of pain varies across individuals, which means that the same painful event can be felt very differently among children.
Pain is like a puzzle that is made up of different pieces. There is a biological piece (e.g., previous injuries can make a person more sensitive to pain), a psychological piece (e.g., memories of past pain experiences can impact future pain experiences) and a social experience piece (e.g., the people who are in the room with you can impact how much pain you feel and how much pain you actually express). Even within the same person, the impact each piece has can change from situation to situation or as someone matures over their life. So even the same painful event can be experienced by the same person differently at different points in time!
Common causes of acute pain in children include everyday bumps and bruises (e.g., when a child falls off a bike), routine medical procedures (e.g., getting a needle at the doctor’s office), and post-surgical pain (e.g., the pain following tonsil removal that often lasts days). A person’s report of pain must be respected and paid attention to, no matter how old the person is. Sometimes a child cannot tell us they are in pain because they are too young or have intellectual or developmental disabilities. However, a good rule of thumb is that anything that causes pain in adults will also cause pain in children. There are well-validated ways to help assess and understand the pain of infants, children, and teens.
Assessment of acute pain in children
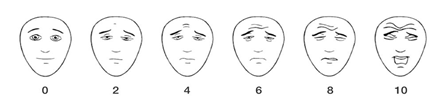
Scientists and clinicians know that pain is tricky to assess even in adults, so a lot of work has gone into trying to understand the best ways to measure pain in children. With infants, toddlers, and preschoolers, watching body language is often the best way. For example, the FLACC (Face, Legs, Activity, Cry, Consolability) scale instructs caregivers to focus on the infant/child’s grimacing face, flailing legs, arched body or squirming, if they are crying, and how easily they are consoled. If children are hospitalized, it’s possible to use physiological measures like heart rate or how much oxygen is circulating in the blood. The higher the heart rate or the lower the oxygen saturation in the blood, the more stress the child is in and the more pain we assume the child is experiencing. Some pain assessment tools used in the hospital, such as the PIPP-R (Premature Infant Pain Profile-Revised), incorporate both behaviours and physiology measures. Sometime around the age of 6 or 7 years, children are able to self-report their pain more reliably, so parents and health professionals should try to ask them about their pain. For example, the Faces Pain Scale – Revised[1] (see below) is a great way to ask early school-aged children about how much something hurts. For older children and teens, who may have a good understanding of how rating scales work, you can just use a numeric rating scale without any aids. For example, you could ask an older child or teen, “On a scale of 0 to 10, where 0 is no pain and 10 is the worst pain you can imagine, how much pain are you experiencing right now?”.
Why is acute pain a priority in children?
Acute pain occurs frequently in both healthy children and those with chronic illnesses. Although pain serves an adaptive role, it may have adverse effects on the body, mind and social wellbeing of children if left unmanaged. Through experience, children learn the concept of pain, and previous experiences of pain influence how they experience pain in the future. Without appropriate assessment and treatment, acute pain can change how a child processes pain. A fear of needle-related procedures and avoidance of medical appointments may also develop if pain is not properly managed. Sometimes, acute pain can even lead to longer-term pain (i.e., pain that lasts more than 3 months). For example, research has suggested that anaesthesia and analgesia during surgery is important as it may protect a child from longer term pain.
Psychological strategies for managing acute pain in infants, children, and teens
Whether you are the parent (or caregiver) of an infant, child, or teenager, research shows that you play a major role in helping your child prepare for and cope with acute pain experiences. The way your child depends on you for support might look different depending on how old your child is.
Managing pain in infants and toddlers
Since infants (< 2 years old) haven’t yet developed the abilities needed to understand why they are in pain or what they can do to feel better, they rely on their caregivers more than ever to help them make sense of and cope with the experience. Parents can help reduce acute pain in infants and toddlers. One strategy parents can use with their infants that does not require any preparation is as easy as ABCD! The ABCD approach requires parents to calm themselves to help them calm their child. The ABCD’s are:
- Assess your own anxiety. Your infant looks for hints from you to help them make sense of what’s happening. When you are calm, your infant is more likely to feel calm, too. If you have your child in your arms, your slow heartbeat will help you keep your child calm.
- Belly breathe if you are stressed. Take some slow deep breaths in through your nose and into your belly. Slowing your breathing will slow your heart rate which can help slow your infant’s breathing and heart rate.
- Use a calm, close cuddle with your infant. Your cuddle is extremely comforting to your infant, especially when used before, during, and after painful experiences. Depending on how old and active your infant is, this might involve skin-to-skin contact (holding your infant, dressed only in a diaper, against your bare chest, breastfeeding your child) or hugging your child while they sit in your lap or stand between your legs or while in your arms.
- Distract your infant at the right moment. Distracting your infant using a toy, book, bubbles, or song, or by talking to them about something unrelated to the pain can help him or her calm down, but you should wait 30-45 seconds for their crying to slow down and their eyes to open before you start the distraction. Infants might show you that they are not ready for distraction yet (by becoming more upset, pushing the toy away, or looking away in response to the distraction). If this happens, go back to cuddling.
Managing pain in younger children (3-10 years)
Between the ages of about 3 and 10, children are gradually learning what they can do to get themselves through painful experiences, but still rely heavily on their parent or caregiver taking charge of the situation. During this broad age stage, successful coping with pain will usually involves a combination of child-led and parent-led strategies, with a greater emphasis on the parent the younger the child is.
While there are strategies that will work at any age from about 3 to adolescence (described later on), children in this stage have some unique psychological considerations. Children in this stage might experience some anticipatory worries when they know a painful procedure is coming. To help prepare their child for a painful experience, parents can take some extra steps in advance of a planned painful procedure:
- Decide when and how to share information with your child about an upcoming painful procedure. Younger children can be told the day of the procedure. Older children and teens should be told at least the day before, so that they can prepare coping strategies ahead of time and might benefit from learning about and practicing the steps involved in the procedure.
- Answer your child’s questions honestly. For example, if your child asks if a needle will hurt, you might say “It might hurt a small or medium amount, but it will be over soon”.
- Consider offering your child some choice in how their pain is managed, such as how they want to be distracted during the procedure, whether they want to hold your hand, and what they would like to do after the procedure. Offering choices to a young child is usually not helpful and might overwhelm the child. For older children, offering choices in advance (such as before you leave the house) helps them know what to expect and can help them feel more in control of the situation. They can also be motivated to get through the unpleasantness for a reward immediately after the painful procedure (e.g., lollipop) or in the near future (e.g., ice cream stop on the way home). In the below section are strategies that will work with children across childhood.
Managing pain in older children and teens (10+ years)
As children progress through the tween and teen years, they often take on an increasingly independent role in managing their pain. Although the preparatory strategies described above can help reduce the stress your child experiences before a procedure, they should always be used in combination with strategies for managing the pain while and/or after it occurs.
The following strategies can help reduce pain in children and teens during and after a painful experience:
- Effective strategies for distracting your child will vary depending on their age, abilities, and interests, and might include blowing bubbles or pinwheels, playing with a toy or video game, watching a movie, listening to music, or using virtual reality technology. Generally speaking, the more actively the child is involved in the distraction activity, the more powerful the distraction will be.
- Guided imagery. Through guided imagery, you can help your child use their imagination and senses to picture themselves in a different, more calming place. Guided imagery scripts for children of all ages are available online.
- Belly breathing. Breathing exercises that involve diaphragmatic (or “belly”) breathing can be used with children to help them feel calmer during and after painful experiences. Children can be instructed to breathe in through their nose and into their belly (keeping a hand on their belly to check that it rises with each breath) and breathe out through their mouth.
- Coping statements. Teaching children to use coping statements can help them think more positively and feel less negatively about the painful event. Having children repeat statements such as “I can get through this” or “I know the pain will go away”, aloud or in their head, can help them feel better. Reminding them after the painful experience about how well they did, how short the pain was, or how “worth it” the reward was will also help them build better pain memories for the future.
Parent behaviours to avoid
Sometimes despite the best intentions, parents overuse behaviours that have been linked to higher pain-related distress. Parents and caregivers should try to notice and limit their use of these behaviours:
- Reassuring your child by saying things like “it’s ok” or “you’re fine” when your child is visibly distressed or before they are distressed. It can cause them to feel confused, increasing their distress, or it can signal to them that something scary is coming, because parents don’t usually reassure their child when things are fine.
- Criticizing your child’s response to pain. Saying things like “your brother didn’t cry after his needle” or “big girls don’t cry” may teach a child that it is not okay to express pain when they are feeling it, increasing future distress and pain.
- Apologizing for your child’s pain. Apologizing for your child’s pain when you are not the one who caused it can confuse your child. It can also suggest to him or her that their pain has caused distress for you, which can further increase their distress.
Where can I get more information?
Learn more about assessing and treating acute pain at the AboutKidsHealth Pain Hub, a health education resource for children, youth, and caregivers approved by The Hospital for Sick Children (https://www.aboutkidshealth.ca/pain). In addition to describing psychological strategies we mention in this sheet, this resource provides parent- and patient-friendly information sheets that describe important physical (such as using smells and sounds or massage) and pharmacological strategies (such as acetaminophen, sugar water, or numbing cream) that often add to the success of psychological strategies.
You can also consult with a registered psychologist to find out if psychological interventions might be of help to you. Provincial, territorial, and some municipal associations of psychology often maintain referral services. For the names and websites of provincial and territorial associations of psychology, please visit: https://cpa.ca/public/whatisapsychologist/PTassociations
This fact sheet has been prepared for the Canadian Psychological Association by Miranda Di Lorenzo, Shaylea Badovinac, and Dr. Rebecca Pillai Riddell, York University.
Date: November 24, 2020
Your opinion matters! Please contact us with any questions or comments about any of the Psychology Works Fact Sheets: factsheets@cpa.ca.
Canadian Psychological Association
Tel: 613-237-2144
Toll free (in Canada): 1-888-472-0657
[1] Faces Pain Scale – Revised. Copyright ©2001, International Association for the Study of Pain.
