Psychology is rooted in science that seeks to understand our thoughts, feelings and actions. It is also a broad field – some psychology professionals develop and test theories through basic research; while others work to help individuals, organizations, and communities better function; still others are both researchers and practitioners.
Profiles

Dr David Nussbaum

Dr Yusef Karimi
Dr David Nussbaum et Dr Yusef Karimi, Extrémisme et terrorisme
L’extrémisme et le terrorisme ne se limitent pas à une région géographique ou à une période donnée. Nous en voyons les résultats partout dans le monde, ici en Amérique du Nord, au Moyen-Orient, et plus récemment, en Europe. Le Dr David Nussbaum et le Dr Yusef Karimi discutent du rôle de la psychologie dans la compréhension, et éventuellement, dans la prévention de la violence extrémiste.
« J’avais un camarade de classe à l’école secondaire qui était extrêmement intelligent. Il n’était pas religieux à cette époque; la plupart des Kurdes sont séculiers et ils ne croient pas beaucoup en une religion fondamentaliste ou extrémiste. Alors que j’étais étudiant à la maîtrise à l’université, j’ai appris qu’il s’était associé à Al Qaeda en Afghanistan. À ce moment-là, je me demandais pourquoi les gens souhaitaient rallier Daech, Al Qaeda et d’autres groupes extrémistes. Surtout que la plupart de mes amis et moi-même avions toujours été contre ces groupes dans ma province. Environ un an après, j’ai entendu dire qu’il avait été tué en Afghanistan avec Abdullah Massoud. J’étais en état de choc. Pourquoi? Pourquoi les avait-il rejoints? Où étaient les racines psychologiques de tout ce processus? »
Le Dr Yusef Karimi est Kurde. Il est venu au Canada de l’Iran, quand sa femme a obtenu un bon emploi ici il y a un peu plus d’un an. Il a terminé son doctorat en psychologie du counseling en Iran, où il s’est particulièrement consacré à comprendre ce qui motive les gens à s’associer à des groupes comme Al Qaeda. Pendant quatre ou cinq ans, il s’est rendu dans les villages de long de la frontière de l’Iran et de l’Irak lors de la prière du vendredi, et passant le reste de la fin de semaine à interviewer les membres de groupes extrémistes.
« J’ai communiqué avec eux, recueilli beaucoup d’information à leur sujet, en plus d’interviewer 16 djihadistes salafistes. Malheureusement, après ces entrevues, trois d’entre eux se sont joints à Daech en Syrie et se sont fait tuer là-bas. En tant qu’être humain et psychologue, j’avais appris à connaître ces gens pendant un moment. Leur mort m’a beaucoup déprimé. À cette époque, ma première idée était de trouver le moyen de convaincre les gens de ne pas s’associer à ces groupes extrémistes au départ. À ce jour, j’essaie toujours de trouver la réponse à cette question. »
La réponse, selon le Dr Karimi, ne se trouve certainement pas dans ce que l’Occident a fait sur le plan du contre-terrorisme, en envahissant l’Afghanistan et l’Irak avec pour objectif l’édification de la nation, menant des frappes de drones en Syrie et en Somalie, sans compter les autres interventions qui commencent par des agressions et aboutissent à des occupations militaires. Il évoque les événements récents survenus en Afghanistan, la résurgence des talibans après le retrait des États-Unis, comme exemple patent des lacunes de cette stratégie.
« Je crois que ce qui a été fait au Moyen-Orient sur le plan de la lutte contre le terrorisme et l’extrémisme est voué à l’échec en raison des répercussions de l’emploi de méthodes inappropriées. L’éradication de l’extrémisme actuel requiert une approche phénoménologique qui s’attaque aux racines du problème. Les politiciens et les responsables des politiques préfèrent habituellement définir et évaluer les groupes extrémistes présentement actifs au Moyen-Orient en fonction de leur capacité organisationnelle existante, plutôt que des menaces réelles qu’ils posent.
En tant que psychologue, en tant que personne ayant visité ces pays du Moyen-Orient et qui fait partie de cette culture, ce que nous avons observé au cours des derniers mois en Afghanistan est l’échec des efforts des 20 dernières années visant l’édification de la nation. Nous pouvons considérer de multiples facteurs ayant mené à ce revers, mais à mon avis, il en est un que nous devrions examiner de très près. C’est-à-dire l’absence de connaissances des caractéristiques individuelles du peuple afghan. Dans cette situation, la psychologie peut nous fournir une très grande quantité de connaissances sur les caractéristiques d’une communauté donnée. Et cela peut nous mener loin sur la voie de la pacification et de la résolution des conflits. »
Les talibans, de retour aux commandes de l’Afghanistan, ont fait les gros titres ces dernières semaines lorsqu’ils se sont joints au reste du monde pour appeler à une résolution pacifique de l’invasion russe en Ukraine. En soi, cet appel a suscité beaucoup de réactions partout dans le monde : « quand les talibans réclament la paix, on sait qu’il se passe quelque chose de terrible… », ce qui traduit une sérieuse absence de nuance et de compréhension à l’égard de la région.
En 1989, les moudjahidines afghans ont défait l’Union soviétique, la repoussant hors de l’Afghanistan après une guerre longue et coûteuse. Puis, ils sont arrivés à renverser le gouvernement afghan soutenu par les communistes en place à ce moment, mais se sont rapidement fractionnés, et après une seconde guerre civile en Afghanistan, ont cédé le pouvoir aux talibans. Les moudjahidines se sont dispersés dans toutes les directions, dont l’une était menée par Oussama ben Laden, un des supporteurs les plus connus des moudjahidines.
L’agression soviétique, maintenant russe, n’a rien de nouveau. Avant l’invasion odieuse de l’Ukraine, ces derniers jours, les forces militaires de Poutine et les fermes de bots s’adonnaient au cyberterrorisme partout sur la planète, ce qui aurait pu être un signal pour le reste du monde qu’ils préparaient quelque chose de plus conventionnellement violent.
Le Dr David Nussbaum est le président de la Section de l’extrémisme et du terrorisme de la SCP. Le Dr Nussbaum a un doctorat en psychologie biologique, mais il souligne qu’il a vraiment appris la psychologie clinique au volant d’un taxi qu’il conduisait deux nuits par semaine pendant quatre ans, alors qu’il terminait son doctorat. Il a fait des études postdoctorales en neuropsychologie, au cours desquelles il s’est intéressé à la psychologie médicolégale. Il est devenu membre de la Section de la justice pénale de la SCP, et en a été le président pendant sept ans. Il y a fait la rencontre du Dr Wagdy Loza, alors psychologue en chef au pénitencier de Kingston. Le Dr Loza a lancé la Section de l’extrémisme et du terrorisme et le Dr Nussbaum fut l’un des premiers signataires ayant contribué à obtenir le statut initial de la section. Cela l’a orienté vers le terrorisme au Moyen-Orient, mais il parle du lien entre le communisme, l’extrémisme et le terrorisme depuis de nombreuses années.
« Les gens sont séduits par la promesse d’une utopie communiste, le paradis du travailleur. Sauf qu’après cinq ans dans une économie marxiste, ils sont chanceux de pouvoir manger. Ils pourraient invoquer qu’ils ressentent le remords de l’acheteur et qu’ils veulent se débarrasser du gouvernement. C’est à ce moment que la nature totalitaire, draconienne de l’étatisme émerge. Pensez aux goulags russes, et ainsi de suite. »
La nature totalitaire et draconienne de Poutine l’étatiste est actuellement manifeste, tandis que le monde réagit à l’invasion de l’Ukraine par une condamnation quasi universelle. Cependant, il est intéressant de noter la différence entre la réaction du monde à cette invasion, lorsqu’on la compare avec l’invasion américaine de l’Afghanistan ou l’offensive de l’Arabie saoudite au Yémen. La guerre est la guerre, qu’elle ait lieu au Moyen-Orient ou en Europe, et le Dr Nussbaum affirme sans ambages qu’il n’existe pas de lieu unique où le terrorisme, ou les idéologies qui le produisent prospèrent.
« Le terrorisme ne se limite pas à une région géographique, à une idéologie particulière; il y a des terroristes partout au monde, et ce, depuis des millénaires. Aujourd’hui, dans les 25 ou 30 dernières années, c’est devenu un enjeu majeur parce que diverses idéologies cherchent à prendre le contrôle de la planète (ou d’immenses parties de la planète). L’une des choses qu’ils font pour influencer les gouvernements et les citoyens est l’utilisation du terrorisme pour instiller la peur afin que les gens se soumettent à leurs diktats. C’est toujours fait dans un but politique. »
Le Dr Karimi mentionne qu’au cours de l’histoire, nous avons souvent dû revoir ce que nous pensions savoir, en raison d’une violence extrémiste que nous n’avions pas envisagée auparavant.
« Nous avons fait l’expérience du fascisme et du racisme en Allemagne avant la Seconde Guerre mondiale. Au XXe siècle, Hannah Arendt affirmait qu’avec la montée du totalitarisme nous étions confrontés à un nouveau phénomène et à une nouvelle réalité. La classe politique n’avait jamais fait face à cette situation auparavant, alors elle disait que nous devions établir une nouvelle science de la politique pour expliquer et interpréter le terrorisme. Tout comme ce qu’affirmait Alexis de Tocqueville au XVIIIe siècle après la Révolution française. Aujourd’hui, la psychologie, et la psychologie politique en particulier, fait face à un autre phénomène inédit et à une nouvelle réalité. Cela soulève plusieurs questions. Par exemple, comment pouvons-nous comprendre l’individu dans une société comme l’Afghanistan, ou la Syrie ou l’Irak, dans laquelle l’ordre social repose largement sur une structure tribale? Le fait de tenter d’édifier une nouvelle nation en Afghanistan n’était absolument pas aligné avec cette culture. »
Après le 11-Septembre, l’extrémisme a commencé à devenir un problème grave en Amérique du Nord, les groupes d’extrême droite à idéologie anti-islamiste essaimant partout. Les efforts déployés par l’Occident pour supprimer ces groupes et éviter de leur donner une tribune n’ont eu qu’un effet limité et, ces dernières années, l’extrémisme a atteint de nouveaux sommets en gagnant en puissance.
Selon le Dr Karimi, la solution à ce problème est semblable à la solution au terrorisme moyen-oriental : rejoindre les gens avant qu’ils ne deviennent extrémistes. Ce sera un processus de longue haleine, et ça ne peut se produire du jour au lendemain, mais le fait de comprendre la culture et de l’accueillir sèmera les graines d’une désescalade de l’extrémisme à l’avenir. Il dit du Canada, où il habite depuis un an,
« De nombreux immigrants viennent au Canada et c’est bien ainsi puisqu’ils apportent avec eux une grande quantité de connaissances de l’extérieur. Mais nous devrions avoir un plan pour intégrer ces gens et leur culture. C’est bien beau d’accueillir beaucoup d’immigrants et de réfugiés. Mais on doit compter sur un plan pour les intégrer à la société canadienne. Les voir vivre avec d’autres Canadiens de manière intégrée, pour qu’ils ne soient pas perçus comme “l’autre”, ce qui est actuellement le cas pour nombre d’entre eux. C’est bien que nous ayons un pays multiculturel, mais nous pourrions faire beaucoup plus pour tirer profit de ce multiculturalisme afin de rendre le Canada meilleur. »

Dre Wendy Darr

Dr Allister MacIntyre

Dr Damian O’Keefe
Dre Wendy Darr, Dr Allister MacIntyre, Dre Susan Dowler et Dr Damian O’Keefe, Psychologie du milieu militaire
Les psychologues dans l’armée jouent de nombreux rôles, de la sélection du personnel à la conception de la formation en passant par un certain nombre de rôles thérapeutiques. Nous avons échangé avec la Dre Wendy Darr, le Dr Allister MacIntyre, la Dre Susan Dowler et le Dr Damian O’Keefe pour en apprendre davantage sur le sujet.
Psychologie du milieu militaire
Au milieu des années 1980, « un véritable exercice militaire était mené en Europe, impliquant des pays de partout dans le monde. Les Allemands de l’Ouest ont été chargés de la “guerre psychologique”. Il s’agissait d’un exercice d’entraînement et tous les individus qui y étaient engagés savaient que ce n’était pas une vraie guerre. Les Allemands de l’Ouest ont rédigé un seul tract qui a mis un terme à tout l’exercice. Ils ont attendu la fin de la deuxième semaine de l’exercice. Les soldats de première ligne avaient dormi dans la boue, ils étaient crasseux et ils étaient fatigués. S’ils dormaient un peu, ils étaient privés de sommeil – en fait, ils se sentaient absolument malheureux. Le tract que les Allemands de l’Ouest ont distribué ressemblait en tout point à une publicité de la pizzeria du coin, offrant de livrer des pizzas gratuitement à leurs camarades de l’échelon arrière : les infirmiers, les personnes chargées de l’approvisionnement et celles qui n’étaient pas au combat. Quand les soldats sur le terrain ont réalisé que pendant qu’ils vivaient dans la boue et mangeaient des boîtes de rations, leurs collègues soldats étaient derrière eux, à manger de la pizza gratuite, ils se sont dit merde, et ils ont démissionné. On ne ferait pas ça dans un vrai scénario de guerre, mais dans ce scénario en temps de paix, l’énorme écart entre leurs conditions de vie et ce qu’ils percevaient des conditions de vie des autres a suffi pour qu’ils décident de ne plus jouer le jeu ».
Le Dr Allister MacIntyre a passé 31 ans dans les Forces armées canadiennes en tant qu’officier de sélection du personnel. Il est titulaire d’un doctorat en psychologie sociale, mais sa thèse portait davantage sur les comportements au travail : la culture, le climat et le leadership au sein de l’Aviation royale canadienne. Quand il était encore un militaire en uniforme, il s’est rendu en Allemagne de l’Ouest. Il y a suivi un cours offert par l’armée sur la guerre psychologique, destiné aux officiers de l’OTAN. Il intègre aujourd’hui certains des principes qu’il a retenus au cours sur l’influence et la persuasion qu’il donne au Collège militaire.
En général, quand nous pensons à la guerre psychologique, nous pensons aux militaires américains faisant jouer du Van Halen à tue-tête pendant des jours pour faire sortir Manuel Noriega de sa forteresse au Panama. (Le fait de lancer Panama de Van Halen dans ce scénario était, selon l’humble avis de l’auteur de ces lignes, un moyen plutôt ringard et beaucoup trop direct.) Récemment, le soi-disant convoi de la liberté qui a bloqué Ottawa pendant trois semaines a été accusé de mener une guerre psychologique par les politiciens, les juges et les forces de l’ordre, parce qu’ils ont usé de leurs klaxons incessants et de sirènes stridentes pour perturber le sommeil et le quotidien des résidents du quartier. Le Dr MacIntyre affirme que le concept général est beaucoup plus vaste que cela.
« La “guerre psychologique” n’est pas vue comme une discipline de la psychologie, elle est beaucoup plus associée à une discipline militaire qui se sert de principes psychologiques. Elle implique des choses comme la propagande, pour influencer vos ennemis et aussi pour obtenir le soutien sur le front intérieur. Les gens croient que la guerre psychologique vise à faire quelque chose à l’ennemi, mais il s’agit surtout d’obtenir le soutien de sa propre nation pour dire “nous faisons vraiment un travail légitime ici”. Certaines des choses que j’ai apprises dans ce cours étaient assez fascinantes pour ce qui est d’apprendre à connaître la culture du groupe que l’on tente d’influencer, en vue de déterminer les déclencheurs à employer pour le faire pencher dans un sens ou dans l’autre. »
Le Dr Damian O’Keefe a un doctorat en psychologie du travail et des organisations et il étudie le comportement humain en milieu de travail. Tout comme le Dr MacIntyre, il compte 30 ans de service militaire et il travaille actuellement à titre de scientifique civil de la Défense à la Division recherche et analyse (personnel militaire) du ministère de la Défense nationale, où il dirige des recherches appliquées pour soutenir les politiques relatives au personnel des Forces armées canadiennes. Il s’empresse de souligner que les psychologues canadiens ne participent pas à la guerre psychologique.
« Nous avons presque tous obtenu nos diplômes au Canada, donc nous respectons tous le code d’éthique de la SCP. S’abstenir de faire du mal représente le principe fondamental qui nous guide. »
L’emploi le plus courant pour un psychologue en uniforme dans les forces militaires canadiennes est celui d’officier de sélection du personnel. La psychologie fait partie des forces militaires canadiennes depuis la Deuxième Guerre mondiale, quand les psychologues ont aidé l’armée à mettre en place un mécanisme efficace de sélection des volontaires qui allaient occuper divers postes dans l’armée. Depuis, les psychologues sont engagés dans la sélection du personnel militaire. Vous pouvez en apprendre davantage sur les origines de la psychologie dans le contexte militaire et le travail qu’accomplissent actuellement les psychologues dans un chapitre de l’ouvrage Canadian Handbook for Careers in Psychological Science, corédigé par Damian O’Keefe, Samantha Urban et Wendy Darr.
La Dre Wendy Darr travaille aussi à la sélection et à l’évaluation, et elle a récemment remplacé le Dr O’Keefe à la tête de la Section de la psychologie du milieu militaire de la SCP. Elle est également scientifique civile de la Défense et elle dirige des recherches et des analyses relatives au personnel pour les forces militaires. Les recherches de la Dre Darr sont axées sur l’élaboration de nouveaux outils de sélection pour la sélection et le recrutement de personnes qui souhaitent devenir des soldats, des marins et des aviateurs. Elle décrit les critères qui permettent aux candidats d’être acceptés dans l’armée au Canada.
« Nous souhaitons surtout trouver ce que 100 ans de recherche ont déterminé comme le meilleur prédicteur de rendement au travail, c’est-à-dire la capacité cognitive générale. Les forces armées canadiennes forment tout le monde, et une grande part de cette formation est très dispendieuse. Alors, nous voulons nous assurer d’investir dans les personnes qui possèdent les aptitudes et la capacité de réussir, particulièrement dans les emplois plus techniques. Ainsi, à la base, nous cherchons à voir si vous êtes sain d’esprit et possédez la capacité d’apprendre. La seconde dimension concerne la personnalité. Êtes-vous compatible avec les exigences d’un environnement militaire? Nous sommes à la recherche de personnes qui adhèrent aux valeurs militaires. Le candidat a-t-il l’aptitude innée de réussir dans un milieu reposant sur des règles, d’être organisé et structuré, et d’agir comme un meneur lorsque nécessaire? Nous cherchons également des personnes qui ont ce qu’il faut pour offrir un bon rendement dans un contexte d’adversité. Êtes-vous stable sur le plan émotionnel? L’entraînement militaire peut être ardu, alors nous voulons nous assurer que les gens ont ce qu’il faut pour composer avec les pressions de l’entraînement. »
Les forces militaires comptent sur toutes les disciplines de la psychologie. Elles disposent de psychologues du travail et des organisations, de psychologues spécialisés en psychologie sociale et de psychologues cliniciens pour soutenir les militaires lorsqu’ils sont aux prises avec des problèmes de santé mentale. Ces psychologues travaillent dans les cliniques militaires et dans certaines unités spécialisées. La vaste majorité des psychologues travaillent dans les 31 cliniques militaires situées partout au Canada, qui comprennent sept centres de soutien pour trauma et stress opérationnels (CSTSO) et prodiguent des soins de santé mentale très semblables à ce qui est offert dans les hôpitaux. (Aussi tiré du Canadian Handbook for Careers in Psychological Science.)
La Dre Susan Dowler est psychologie clinicienne en chef à la Direction de la santé mentale des Services de santé des Forces canadiennes. Elle est la responsable principale de la pratique en psychologie, ce qui signifie qu’elle participe à l’élaboration des lignes directrices relatives à la pratique et à la conformité, mène des enquêtes en cas de problèmes et met en place des formations éducatives. Au contraire des officiers de sélection du personnel, les psychologues cliniciens sont toujours des civils.
« Pour ce qui est des psychologues cliniciens, ils ne sont pas membres du personnel militaire, ils ne sont pas des personnes en uniforme. Ils sont soit des employés de la fonction publique ou des professionnels contractuels. Certains autres pays ont des psychologues cliniciens intégrés aux unités, par exemple les États-Unis, mais en général ce n’est pas le cas au Canada. »
En janvier 1994, Roméo Dallaire envoyait le désormais célèbre ‘fax sur le génocide’ au siège de l’ONU, alertant qu’un génocide était planifié au Rwanda. Quelques mois plus tard, le génocide s’amorçait : entre 500 000 et un million de Tutsis ont été tués sur une période de 100 jours. Dallaire, se sentant abandonné et ignoré par l’ONU et ayant témoigné de mois d’horreurs inimaginables, a beaucoup souffert d’un trouble de stress post-traumatique (TSPT) après le Rwanda. Il a milité en faveur de la création de services de santé mentale spécialisés pour traiter les blessures de stress opérationnel. Le Dr Dowler mentionne que le premier CSTSO a été créé en 1999.
Au fil du temps, les psychologues cliniciens sont de plus en plus engagés auprès de l’armée et ils jouent un rôle essentiel lorsque des problèmes surviennent. La stigmatisation associée à la recherche d’aide en santé mentale a toujours été omniprésente dans la société, mais plus particulièrement dans le milieu militaire où, comme le souligne le Dr MacIntyre, « on s’attend à ce que les gens soient forts ». Le Dr O’Keefe et lui-même se sont tous deux rendus en Australie, pour travailler avec l’armée australienne. Ils ont remarqué, il y a de nombreuses années, que tous les soldats qui avaient été déployés pour quelque raison que ce soit devaient consulter un psychologue à leur retour en Australie. Ce n’était qu’un dépistage, mais cette démarche éliminait une part de l’ostracisme entourant le fait d’avoir à parler à un professionnel, puisque tout le monde devait le faire. Le Dr Dowler indique qu’une pratique similaire est en place dans les forces militaires canadiennes.
« Nous faisons depuis longtemps du dépistage postdéploiement. Entre trois à six mois après le déploiement, les soldats remplissent des questionnaires et ont une entrevue avec un travailleur social. Si une information est jugée comme étant potentiellement problématique, le militaire est orienté vers les services de santé mentale. Pour voir un psychologue, il faut être aiguillé par le personnel médical. »
Le dépistage postdéploiement n’est qu’une partie du processus auquel sont soumis les soldats après avoir participé à des combats. Les psychologues ont ajouté une nouvelle étape pour rendre le retour au Canada et à la vie familiale un peu plus facile et plus réussi. Le Dr O’Keefe explique :
« Quand les soldats reviennent d’un déploiement outremer, ils passent par une “décompression dans un tiers lieu”. C’est-à-dire deux ou trois jours pendant lesquels ils sortent du théâtre des opérations qui étaient potentiellement très difficiles. Ils se rendent dans un endroit très calme et la plupart du temps au climat assez chaud, où ils reçoivent des breffages de la part de gens comme Susan (psychologues cliniciens) et d’autres professionnels qui leur disent “si vous ressentez ce symptôme, voici ce que vous devez faire”. On ne peut pas mettre des soldats dans un avion et les renvoyer chez eux directement d’Afghanistan. Ils ont besoin de temps pour décompresser et pour absorber ce qu’ils ont vécu. Et, évidemment, pour obtenir de l’aide professionnelle s’ils en ont besoin. »
Les psychologues font partie du processus militaire depuis le moment où un individu s’enrôle jusqu’aux années qui suivent sa dernière mission. Ils les aident à s’entraîner, à performer et à guérir pour qu’ils soient aussi sains, adaptés et émotionnellement stables que possible lorsqu’ils se rendront à leur soirée pizza.

Alejandra Botia

Emily Winters
Alejandra Botia et Emily Winters, section des étudiants
Les étudiants en psychologie, comme tous les étudiants, ont eu une adaptation difficile à faire ces deux dernières années. Alejandra Botia et Emily Winters nous ont parlé de ce qu’elles font pour aider leurs camarades étudiants à relever les nouveaux défis posés par la COVID.
Emily Winters est beaucoup moins verte, mesure environ un mètre et demi de plus que Yoda et parle de manière beaucoup moins énigmatique que lui. Elle est étudiante au doctorat en psychologie clinique à l’Université de Regina et elle est la première responsable de la JEDI de la Section des étudiants en psychologie de la SCP. C’est la première année que la Section des étudiants en psychologie dispose d’une personne responsable de la justice, de l’équité, de la diversité et de l’inclusion – eh oui, le nom a été choisi intentionnellement à partir des propositions d’autres membres étudiants.
« Je suis la première personne à occuper ce poste, et j’étais très heureuse lorsqu’on l’a créé. Nous avons déjà commencé à recruter des bénévoles pour former un comité JEDI, et cela devrait bientôt être terminé. Son rôle principal sera de compiler des listes de ressources qui seront mises à la disposition des membres de la section. Nous espérons également organiser un événement en vue du congrès de 2022, destiné aux étudiants et portant sur la justice, l’équité, la diversité et l’inclusion. »
Lorsque le Haut Conseil Jedi a été créé, ses membres ont été choisis très intentionnellement. Plo Koon était un Kel Dor originaire de Dorin – c’est lui qui devait porter des lunettes et un masque pour pouvoir respirer dans certaines atmosphères. Adi Gallia représentait le peuple tholothien, Ki-Adi-Mundi, avec son cerveau binaire, représentait Céréa. Et Mace Windu a été choisi pour satisfaire tous les admirateurs qui aiment vraiment voir Samuel L. Jackson en action. Le comité JEDI de la Section des étudiants en psychologie sera semblable – un comité chargé de la diversité et de l’inclusion doit également veiller à la représentativité.
« Comme il s’agit d’un rôle joué par la section pour les étudiants, c’est un objectif très important pour nous – rendre la population étudiante aussi diverse et équitable que possible. Il est également important de penser à long terme pour que les cliniciens, les chercheurs et les psychologues en général intègrent ces valeurs dans leur travail et leur pratique. J’essaie de garder à l’esprit qu’il ne suffit pas d’augmenter le nombre d’étudiants issus de groupes marginalisés pour obtenir des changements concrets. Cela ne peut être notre seule stratégie. Nous devons nous assurer que les psychologues pensent de cette façon : qui ils embauchent dans leurs laboratoires, à quoi ressemble la composition de leur cabinet. »
Cette idée, à savoir que le simple fait de recruter des étudiants d’origines diverses n’aboutira pas à une diversification à long terme, est également reprise au conseil d’administration de la SCP. Alejandra Botia est étudiante de troisième année en psychologie à l’Université de la Colombie-Britannique et elle est la présidente de la Section des étudiants en psychologie. Son rôle de présidente consiste notamment à représenter la section au conseil d’administration.
« J’ai rejoint le conseil d’administration à l’été 2020, à une époque où nous discutions beaucoup de la justice sociale et des injustices raciales. Ce qui me plaît le plus dans le fait d’avoir rejoint la SCP à ce titre, c’est de rencontrer des gens comme Emily, et de siéger au conseil d’administration aux côtés de personnes qui travaillent très dur et qui tiennent véritablement à se réunir pour discuter de sujets intéressants et difficiles. Il faut beaucoup de courage et d’humilité pour être capable de se présenter dans ces contextes. Ce que je constate, c’est que le conseil se réunit pour faire cela. Et je suis aussi très inspirée par les étudiants que j’ai rencontrés. Souvent, il faut encore plus de courage pour se montrer dans ce contexte, car en tant qu’étudiants, nous avons souvent moins de pouvoir. Au conseil d’administration, j’essaie de faire en sorte que la parole des étudiants soit de plus en plus entendue. L’une des choses merveilleuses que nous avons faites l’année dernière a été d’élaborer un sondage auprès des membres étudiants pour savoir ce qu’ils attendaient du rôle actuel d’Emily. Qu’est-ce qui était important pour eux? Ce qu’ils voulaient que nous considérions, même le nom. C’est là que je peux vraiment faire le lien entre ce que fait la Section des étudiants et ce que fait le conseil d’administration. »
Les membres du comité exécutif de la Section des étudiants en psychologie ont dû faire leur travail dans une période d’agitation sans précédent, la pandémie ayant fait que les réunions virtuelles sont devenues la norme. Les membres du comité exécutif sont tous désormais comme Ki-Adi-Mundi, qui n’a jamais assisté en personne à une seule réunion du Haut Conseil Jedi et qui s’est toujours présenté sous forme d’hologramme. Cela a présenté des difficultés non seulement pour le comité exécutif, mais aussi pour les étudiants en général.
Selon Emily, « la transition vers l’université a été assez difficile pendant la pandémie, probablement plus difficile qu’elle ne l’aurait été autrement – surtout pour les étudiants de premier cycle. La transition vers l’apprentissage en ligne a été difficile, et beaucoup de gens n’aiment pas ça. Pour certains, cela fonctionne très bien, mais pour beaucoup, c’est un véritable défi. Le fait d’être isolé a également été très difficile pour les étudiants. Beaucoup d’étudiants de mon programme quittent leur province d’origine pour faire des études supérieures. Ils cessent donc de vivre chez leurs parents pour aller vivre complètement seuls dans l’hiver très froid de la Saskatchewan. Être étudiant est difficile, et le fait d’avoir l’impression d’être seul rend les choses encore plus difficiles. »
Alejandra dit qu’en plus de l’isolement, il y a eu de nombreuses difficultés pratiques.
« Par ailleurs, les étudiants nous disent souvent que cela a perturbé leurs recherches et leur travail clinique. L’impossibilité de se rendre sur le campus et de mener leurs recherches comme ils en avaient l’habitude les oblige à faire preuve d’une grande créativité ou à mettre leur travail en veilleuse. Certains stages ne prenaient plus d’étudiants parce qu’ils ne pouvaient pas le faire. Le fait de devoir attendre, et peut-être de reporter certaines exigences de leur programme à cause de la pandémie, a vraiment préoccupé beaucoup d’étudiants. Les problèmes financiers ont également été soulevés – les étudiants ne sont pas très payés, si tant est qu’ils le soient; en raison de la pandémie, ils ont été privés des emplois qu’ils occupaient auparavant et des débouchés auxquels ils avaient accès auparavant. »
Pendant cette période, les liens, de quelque nature que ce soit, sont devenus plus importants que jamais. Le mentorat est l’un des moyens par lesquels ces liens se sont établis dans la Section des étudiants en psychologie. Où serait Luke Skywalker sans le mentorat de Yoda? Ou Anakin sans Obi-Wan… oubliez le dernier exemple. L’année dernière, Alejandra était la responsable du programme de mentorat étudiant de la SCP, et bien que le mentorat se soit toujours effectué de manière virtuelle, les étudiants de premier cycle et leurs mentors de deuxième et troisième cycles se trouvant rarement dans la même ville, et encore moins dans la même école, elle affirme que cette façon de communiquer est devenue plus importante et utile que jamais pendant la COVID.
« Le programme de mentorat a été formidable, en partie parce qu’il a permis d’établir des liens entre mentoré et mentor, mais aussi pour trouver des idées. Plusieurs questions ont surgi : « Je ne peux pas faire de stage, que puis-je faire d’autre? », et ainsi de suite. C’était une situation si peu habituelle, surtout pour des étudiants de premier cycle, que le fait d’avoir quelqu’un qui les aide à la traverser a été un exutoire très agréable. »
La pandémie a mis en lumière de nombreuses divisions au sein de la société canadienne, et plus particulièrement les inégalités dont souffrent plus lourdement que les autres les Noirs, les Autochtones et les personnes de couleur. Les étudiants en psychologie d’aujourd’hui et les membres de la Section des étudiants en psychologie ne font pas exception. Selon Alejandra,
« Les événements que nous avons vécus et dont nous avons été témoins ces dernières années ont également fait des ravages. Je pense aux Noirs et aux Autochtones, aux injustices raciales et à l’oppression systémique que beaucoup de personnes ont subies et continuent de subir. Je pense aussi aux crimes haineux contre les Asiatiques; de nombreux étudiants ont eux-mêmes fait l’expérience de la haine à caractère raciste pendant cette période. Pour les étudiants de couleur, ce fut une période particulièrement difficile. C’est l’une des raisons pour lesquelles il est si important de continuer à créer des lieux et des occasions permettant aux gens d’entrer en contact les uns avec les autres. »
Emily est maintenant chargée de créer l’une de ces possibilités de contact grâce à l’initiative JEDI. Le groupe vient juste de démarrer, mais elle et le reste du comité exécutif de la section ont une vision particulière de ce nouveau groupe.
« Il est encore tôt et je veux être sûre que le processus sera très collaboratif. Je veux m’assurer que le comité que nous allons créer est le plus diversifié possible du point de vue de la défense des intérêts. Je veux m’assurer qu’il y a, au comité, quelqu’un qui peut se concentrer sur la question des personnes handicapées, quelqu’un qui peut se charger des questions qui touchent les Noirs, etc. Nous voulons nous assurer d’avoir cette représentation dans la mesure du possible, sans attendre de ces personnes qu’elles parlent au nom de toute une communauté et qu’elles représentent un point de vue unique! Pour ma part, l’une des choses que je veux vraiment défendre, c’est la cause des peuples autochtones. Je suis de descendance inuite et européenne. La famille de mon père vient du Nunatsiavut, un territoire qui s’étend le long de la côte du Labrador; c’est donc une cause qui me tient personnellement à cœur. Je pense que c’est le cas pour beaucoup de gens, surtout avec la découverte des fosses dans les pensionnats; c’est un sujet qui intéresse beaucoup de gens. Comme responsable de la JEDI, une chose que j’aimerais faire, c’est de me plonger dans le rapport de la Commission de vérité et réconciliation et les appels à l’action. Pour voir ce que nous pouvons faire dans notre optique, et comme section. Et examiner où nous en sommes dans le domaine de la psychologie en général et où nous pouvons aller dorénavant et ce que nous pouvons mettre en œuvre. Je pense également qu’il est important de se pencher sur la COVID et sur la façon dont elle a touché particulièrement les communautés racisées, car il est évident que la pandémie a eu des répercussions disproportionnées sur les PANDC. »
Ce qu’Emily n’a pas dit – mais aurait peut-être pu dire – c’est « Tu dois désapprendre tout ce que tu as appris. Fais-le ou ne le fais pas! Il n’y a pas d’essai. »

Dr Jim Cresswell

Dr Thomas Teo
Dr Jim Cresswell et Dr Thomas Teo, Histoire et philosophie de la psychologie
Le domaine de l’histoire et de la philosophie de la psychologie est un champ d’études très vaste. Il implique en grande partie un mode de pensée axé sur une « vue d’ensemble ». Nous avons échangé avec le Dr Jim Cresswell et le Dr Thomas Teo sur leur manière de percevoir cette vue d’ensemble.
Histoire et philosophie de la psychologie
« Pensez aux films et aux émissions de zombis : les zombis sont littéralement des sous-hommes. Vous pouvez tuer les zombis, les maltraiter sans vergogne, ils n’ont aucun droit. En réalité, vous avez le devoir de tuer les zombis parce qu’ils menacent d’anéantir votre mode de vie. »
Le Dr Thomas Teo est membre de la faculté des études historiques, théoriques et critiques du programme de psychologie de l’Université York. Pendant toute sa carrière professionnelle, il a activement contribué aux avancées en matière de psychologie théorique, critique et historique. Il a commencé par s’intéresser à l’histoire du racisme, a travaillé sur la relation entre la psychologie et le racisme et sur la mesure dans laquelle la psychologie scientifique peut être une forme de violence, que le Dr Teo désigne comme de la « violence épistémologique » (l’épistémologie est une branche de la philosophie s’attardant aux connaissances). Récemment, il a étudié la réémergence de la subjectivité fasciste, reposant sur le concept de sous-humains et le racisme, ainsi que la notion de suprématie culturelle que nous observons en Occident.
« Tandis que le racisme peut dans une certaine mesure reposer sur la science, notamment à l’aide de chiffres et de graphiques, la notion voulant que des gens soient sous-humains ne le peut pas. L’idée d’une classe de sous-humains, pensez aux zombis, constitue strictement une ontologie [la branche de la philosophie qui traite de l’être] visuelle. Vous ‘voyez’ et savez ce qu’est un zombi et vous n’avez pas besoin d’une explication scientifique pour le faire. Et il en est ainsi pour certains individus quand ils voient, disons, des migrants qui arrivent à la frontière. Ils courent, forment une caravane, ils marchent dans la neige, transportant des valises, jusqu’à la frontière, vers un endroit où ils ne peuvent obtenir d’accès “régularisé”. Ce comportement semble “anormal”, déviant de la façon dont les Américains et les Canadiens “ordinaires” se comportent. Cela montre visuellement qu’“ils” ne sont pas comme “nous”, qu’ils sont une classe de sous-hommes. Vous pouvez les maltraiter, les séparer de leurs familles, les mettre en cage. »
Le Dr Teo avance en fait que de les mettre en cage représente un moyen de les faire paraître encore plus sous-humains aux yeux du grand public. Cette situation prend sa source dans une longue tradition de déshumanisation des autres, en les dépeignant comme dégoûtants, parasitaires, hirsutes et désespérés. Ce qui correspond exactement à ce à quoi ressembleront les migrants retenus en cage à la frontière, sans douche ou savon ou nourriture décente, des semaines ou des mois durant.
« Je fonde cet argument sur deux sources, poursuit-il, dont l’une est une auteure américaine [Lothrop Stoddard] qui a écrit sur le “sous-homme”, une catégorie comprenant les “races inférieures”, les gens pauvres, les communistes et les bolchevistes. La seconde source est un manuel éducatif produit par les SS en Allemagne nazie, un livret ayant réellement pour titre “Sous-humain”. Il y avait très peu de texte; il y avait tout bonnement des images qui opposaient les humains aux sous-humains. Les soldats allemands face aux soldats soviétiques; les bonnes mamans allemandes face aux mères juives; l’art allemand face à l’art dégénéré. Tout est visuel, nous pouvons observer que le “sous-humain” ne présente pas les caractéristiques d’un être humain complet. Les personnages représentés semblent être en mauvais état, sales, désorganisés. Cela signifie aussi que n’importe qui peut devenir un sous-homme. Non seulement les Noirs ou les Juifs, mais quiconque est un ennemi de l’Allemagne, Churchill et Roosevelt en faisant partie. Le concept du sous-humain est très malléable. Il ne signifie pas seulement que vous êtes inférieur aux autres, mais aussi qu’il est impératif de faire quelque chose. Si vous êtes un parasite, une coquerelle, un rat, “Je” dois vous exterminer ou vous faire disparaître. »
Le Dr Teo évoque fréquemment la « subjectivité », soutenant que la discipline de la psychologie doit se concentrer davantage sur cette dimension afin de donner un sens à l’immense quantité d’informations que nous avons glanées des études empiriques depuis des décennies. Par exemple,
« Nous avons divisé la subjectivité en pensée, sentiment et volonté. Puis, nous avons divisé la pensée en attention, perception, cognition et mémoire. La mémoire peut être divisée en mémoire à long terme, à court terme et épisodique. Puis, vous examinez la manière dont un seul petit aspect de la subdivision d’une subdivision est lié à un autre petit aspect. Et il devient très difficile de relier le tout à un ensemble, à un point de vue à la première personne (subjectivité). »
Poser un regard sur l’ensemble de la situation est le mantra des personnes qui travaillent dans le domaine de l’histoire, de la théorie et de la philosophie de la psychologie. Le Dr Jim Cresswell est professeur à l’université Ambrose et président de la Section de l’histoire et de la philosophie de la psychologie de la SCP. En plus de son travail dans les sphères de l’histoire et de la théorie, ses champs d’expertise sont, entre autres, la psychologie sociale et culturelle, ainsi que l’immigration et l’adaptation dans le contexte de la recherche communautaire. Il insiste également sur la nécessité d’adopter une perspective plus large.
« En tant que discipline, la psychologie se voit contrainte de composer avec le postcolonialisme, ce qui implique la mise en lumière de biais systémiques, subtils mais omniprésents, à l’égard des gens marginalisés de tout acabit. En psychologie, nous n’avons pas vraiment le bilan le plus reluisant, et cela résulte en grande partie du fait que nous n’avons pas beaucoup de formation nous incitant à réfléchir à ce que signifient nos théories sur le plan des grands enjeux comme la discrimination systémique. Nous focalisons le plus souvent sur le soutien aux individus et sur le travail empirique au moment présent. Or, les psychologues se trouvent ainsi dans une sorte de milieu culturel où se concentrer “uniquement sur ce que la science ou les données indiquent” à propos de l’individu ne passe plus la rampe comme c’était le cas auparavant. Nous devons nous demander comment et pourquoi nos efforts empiriques ont très bien fonctionné pour certaines populations, mais assez mal pour d’autres. » »
Bien que ces entretiens aient été menés il y a quelques mois, plusieurs des propos tenus pas les Drs Cresswell et Teo à ce moment-là trouvent un écho puissant aujourd’hui, particulièrement pour les « autres » populations qui vivent des situations très difficiles à la suite de l’invasion aberrante de l’Ukraine dirigée par Vladimir Poutine, sans compter la propagande aux effluves fascistes et les campagnes de désinformation qui l’accompagnent. Le Dr Teo décrit ainsi la « subjectivité fasciste » :
« Vous pouvez avoir des politiques fascistes, de l’autoritarisme, de la désinformation, de la propagande, et ainsi de suite. La subjectivité fasciste est une dimension individuelle. Si je crois que la richesse ne devrait pas être partagée avec “l’autre”, et que j’étaye ma croyance d’arguments racistes ou sous-humains, alors j’entre dans la subjectivité fasciste. Elle repose sur la notion que la richesse devrait exclure “l’autre” ou que la richesse peut être extraite de “l’autre”. Selon la subjectivité fasciste classique, je peux me rendre dans d’autres pays et extraire la richesse de “ces gens” parce qu’ils sont inférieurs, ils sont des sous-humains, ils sont des parasites. Ils peuvent même être exterminés s’ils deviennent un trop lourd fardeau. »
La pandémie mondiale des deux dernières années est un autre exemple de l’attitude de la société à l’égard de la vie humaine. Le Dr Teo établit une distinction entre ceux qui sont déshumanisés au point où leur extermination n’a que peu d’importance, et ceux qui sont déshumanisés au point où leur mort n’a que peu d’importance, quoique ces deux situations illustrent clairement les deux faces d’une même médaille.
« Nous avons certaines idées sur l’habilité à tuer et l’habilité à mourir. En vertu du nazisme classique, les Juifs sont tuables, tout comme les gitans, les homosexuels, les ennemis, et ainsi de suite. Puisqu’ils sont de races inférieures ou sous-humains, ils n’ont pas le même statut que nous et il n’y a aucun problème à les tuer. L’habilité à mourir est une notion plus intéressante, parce qu’elle nous mène de la subjectivité fasciste plus classique vers sa réémergence à notre époque, où elle s’applique aussi aux démocraties libérales. Dans cette culture, nous tenons des débats, particulièrement en temps de pandémie, où les gens disent que les personnes âgées peuvent être habilitées à mourir, les gens présentant des problèmes médicaux préexistants pourraient être habilités à mourir, les personnes en prison et les travailleurs précaires sont habilités à mourir. Les gens ont fourni des arguments économiques sur l’habilité à mourir de plusieurs de leurs concitoyens : “Si vous voulez préserver votre mode de vie, et votre économie, alors nous devons accepter que certaines personnes meurent.”
Au Canada, nous en avons témoigné depuis longtemps. Les peuples autochtones ont été considérés comme étant tuables, et on pourrait également avancer que dans plusieurs régions des États-Unis, les populations noires sont encore considérées comme tuables, sans conséquence. Actuellement, dans les démocraties libérales, il est impératif que nous discutions de ce problème et de la réalité de l’habilité à mourir, la version plus douce de l’habilité à tuer sous la subjectivité fasciste. »
Cette subjectivité, reposant sur une philosophie impliquant la pensée axée sur une vue d’ensemble et sur les théories fondamentales qui tentent de relier diverses écoles de pensée les unes aux autres, n’est pas nouvelle. Le Dr Cresswell affirme qu’à ses débuts, la psychologie était clairement centrée sur la subjectivité, mais qu’au cours du siècle, elle s’est éloignée du mode de pensée globale. Ce n’est que tout récemment qu’un effort concerté a été investi pour réintégrer de façon signifiante cette philosophie à la psychologie.
« Les premiers psychologues, James, Hall et Piaget pour n’en nommer que quelques-uns, avaient environ 100 ans d’avance sur leur époque concernant la façon de réfléchir à des sujets comme la subjectivité, la recherche et le pluralisme. Le behaviourisme et le cognitivisme, venus plus tard, se sont éloignés de ce mode de pensée initial, qui était plus large et plus systématique. Quand vous regardez en arrière et consultez certains de ces premiers auteurs, vous retrouvez beaucoup d’information pertinente pour le contexte actuel de la discipline de la psychologie.
Les psychologues du 20e siècle se sont largement concentrés sur le travail empirique, tout en délaissant la théorie qui sous-tend ce travail empirique. Le virage culturel a débuté dans les années 1990, provoqué par le discours sur l’éventualité que notre travail puisse être ethnocentrique. Il en résulte un tournant récent, où nous commençons à prêter attention à la théorie qui guide notre recherche et à ce que nous estimons être la signification de nos observations. »
Quoiqu’ils ne soient pas philosophes au sens strict du terme, le Dr Teo et le Dr Cresswell tiennent tous deux des propos plus philosophiques que ne le font la plupart des psychologues. En tant qu’observateurs de l’histoire, ils étudient également l’évolution de la philosophie qui inspire aujourd’hui la discipline. À l’instar de la pensée globale, le Dr Cresswell indique que la pensée philosophique dans la sphère de la psychologie a vu le jour il y a plus d’un siècle.
« Il est probablement plus juste de s’attarder aux personnages comme Sigmund Freud ou William James, en tant que théoriciens ayant mis de l’avant des présuppositions sur la façon d’appréhender le monde. En revanche, pensez à la manière dont les manuels de première et deuxième année parlent d’eux en tant que chercheurs qui ont été “réfutés” par les progrès de la science. Nous disons aux étudiants qu’ils peuvent passer outre à ces figures, sans poser de question sur ce qui est considéré comme de la science et selon qui. Ce message est une posture quelque peu problématique à adopter. Si vous prenez la théorie cognitive et que vous examinez le behaviourisme ou la psychanalyse du point de vue de votre paradigme cognitif, le behaviourisme ou la psychanalyse seront toujours “réfutés”. Si vous examinez la théorie cognitive à travers la lentille du behaviourisme ou de la psychanalyse, la théorie cognitive échouera toujours. Ce que je veux dire c’est que nous devons enseigner aux étudiants à composer avec les paradigmes antérieurs qui ont instauré les conditions permettant le travail empirique. Alors, quand un manuel affirme que nous avons dépassé ceci ou cela, il ignore le fait que la psychologie n’a pas suivi un développement progressif précis à titre de discipline unifiée. En réalité, elle est faite de multiples disciplines et nous devons reconnaître l’existence de différents paradigmes, ce qui suppose de former les étudiants sur la façon de réfléchir à l’histoire et à la théorie. »
Récemment, on a vu l’intérêt croissant que suscite le retour à certaines des périodes où ces idées ont pris de l’importance, particulièrement au tournant du 20e siècle et dans les années 1960 et 1990. Je sais que pour certains, le fait de penser aux années 1990 sous un angle historique pourrait sembler un peu déconcertant. Par exemple, il n’y a que quelques mois qu’Alanis Morisette lançait Jagged Little Pill, n’est-ce pas? (En fait, il y a 26 ans aujourd’hui, elle gagnait un Grammy pour cet album. Elle a maintenant 47 ans.) Le Dr Cresswell affirme que désormais, les années 1990 font réellement partie de l’histoire.
« Prenez Wilhelm Wundt, à qui on attribue le structuralisme et la création du premier laboratoire de psychologie. La moitié de son travail portait sur la völkerpsychologie, qui est la “psychologie de la communauté et des peuples”. Il est utile de revoir une telle théorie culturelle. Un autre corpus littéraire que nous voyons actuellement en histoire et en philosophie concerne la critique et la philosophie continentales. Les gens comme Foucault et les phénoménologues ayant en partie favorisé la naissance de la pensée postcoloniale qui s’est largement répandue travaillaient surtout à l’extérieur de la discipline de la psychologie. Cependant, il est utile de comprendre une telle théorie dans un milieu où nous sommes confrontés à l’injustice systémique. »
Le domaine de la psychologie appelle à se souvenir, et à apprendre, de sa propre histoire. Un aspect auquel nous aussi, en tant que société, devrions nous attarder bien davantage. Je me souviens d’un autre moment historique de la culture pop des années 1990, 1994 pour être plus précis. Une chanson de protestation lancée à la mémoire de Johnathan Ball et Tim Parry, deux enfants tués lors des attentats à la bombe de Warrington perpétrés par l’IRA l’année précédente.
« But you see, it's not me
It's not my family
In your head, in your head, they are fighting
With their tanks, and their bombs
And their bombs, and their guns
In your head, in your head they are crying »
- The Cranberries, Zombie

Dr. Veronica Hutchings

Dr. Reagan Gale
Dre Veronica Hutchings, Charlene Bradford, et Dre Reagan Gale, Psychologie des communautés rurales et nordiques
Vivre dans une petite communauté, en particulier dans le Nord, présente des défis particuliers. Être psychologue dans ces régions comporte également des défis particuliers. Nous avons parlé à la Dre Veronica Hutchings, à Charlene Bradford et à Dre Reagan Gale, de leur travail au Yukon et à Terre-Neuve.
Psychologie des communautés rurales et nordiques
« Les flics ont probablement la vie facile dans une petite ville.
Flic : “Pouvez-vous me décrire votre agresseur?”
Victime : “Oui, il mesurait environ 5’ 10’’…”
Flic : “mmh mmh”
Victime : “Il portait un manteau brun…”
Flic : “mmh mmh”
Victime : “Et c’était… Jim”. »
Je paraphrase un sketch comique d’un humoriste canadien que j’ai entendu un jour à l’émission Juste pour rire. L’identité de l’humoriste et la date du spectacle se sont avérées impossibles à trouver sur Google! Je me souviens d’avoir pensé à l’époque, oui, mais ça doit être difficile aussi pour le flic. La victime connaît Jim, car il connaît tous les habitants de la ville, mais il doit en être de même pour le policier, qui connaît également Jim. La situation est la même pour les psychologues qui travaillent en milieu rural et nordique.
La Dre Veronica Hutchings est psychologue aux services de counseling et de psychologie du campus Grenfell de l’Université Memorial, sur la côte ouest de Terre-Neuve-et-Labrador. Elle est également professeure agrégée aux facultés de médecine et de psychologie. La Dre Hutchings est l’actuelle présidente de la Section de la psychologie des communautés rurales et nordiques de la SCP.
« L’épuisement professionnel est un phénomène courant dans les régions rurales, si l’on considère les relations duelles et le défi que posent les frontières thérapeutiques, auquel on est confrontés dans les petites collectivités. Imaginez que votre liste d’attente s’allonge et que vous vous trouvez dans un petit endroit où les gens savent que vous êtes le seul psychologue ou l’un des rares psychologues de l’endroit. Vous vous retrouvez avec une forte pression : “puis-je prendre cette personne, elle va vraiment mal, puis-je en prendre une de plus?” Cela peut être très épuisant. Je travaille ici, sur le campus Grenfell, et dans la moitié des magasins où je vais, les employés sont des étudiants à qui j’enseigne. J’ai passé 10 ans à Halifax, et pendant cette période, je crois que je n’ai rencontré un client que deux fois! »
La fourniture de services dans les collectivités rurales et éloignées pose d’autres problèmes, parmi lesquels l’accès à Internet, surtout en cette période de pandémie. Mme Charlene Bradford est une psychologue agréée, enregistrée en Alberta, qui exerce en pratique privée au Yukon. Mme Bradford est la présidente de la Psychological Society of the Yukon.
« Au Yukon, nous avons incontestablement des problèmes d’Internet et tout le monde s’en plaint. L’Internet est très cher, et dans les collectivités situées plus au nord, l’accès est très inégal. Il vaut mieux ne pas faire trop de thérapie virtuelle, car il y a souvent un décalage, ou l’écran se fige et on perd contact avec la personne au mauvais moment. Lorsque la pandémie a frappé et que nous avons commencé à faire des choses de manière virtuelle, je suivais une formation sur la prestation de thérapies virtuelles et je me suis dit – bien sûr, cela va fonctionner ici à Whitehorse où les connexions Internet le permettent, mais il est impossible de se fier à la fiabilité de l’Internet dans les communautés rurales.
Au Yukon, nous avons la chance d’avoir une compagnie aérienne exceptionnelle qui dessert régulièrement plusieurs de nos communautés nordiques, ce qui donne lieu à de nombreux vols. Cela aide, mais il faut aussi avoir des cliniciens capables de se déplacer. »
La Dre Hutchings dit que certaines collectivités du Labrador ont les mêmes problèmes d’Internet. Tant à Terre-Neuve qu’au Yukon, certaines petites communautés ont entièrement fermé leurs portes ce qui fait en sorte qu’il n’y a pas de services psychologiques accessibles par avion. Mme Bradford a vu de petites communautés être durement touchées par le virus, qu’elle qualifie de « dévastateur ». La pandémie avait déjà entraîné une demande massive et des temps d’attente très longs, et les communautés touchées de plein fouet par la COVID n’ont fait qu’accroître le besoin d’aide psychologique.
La pandémie et la petite taille des communautés où travaillent les psychologues dans les zones rurales et nordiques ne sont que deux éléments qui ont une incidence sur la façon de travailler des psychologues et qui font que leur façon de fonctionner soit bien différente en zone urbaine. La Dre Reagan Gale est directrice de la psychologie clinique pour le gouvernement du Yukon. Elle est autorisée à exercer en Alberta, dans les Territoires du Nord-Ouest, au Nunavut et en Ontario, et elle est l’actuelle vice-présidente de la Psychological Society of the Yukon.
« J’ai grandi en Ontario, et ce que je peux dire depuis mon arrivée dans le Nord, c’est que je constate combien la nécessité de mettre l’accent sur la sécurité culturelle et les modes de connaissance et de compréhension autochtones devient encore plus cruciale lorsqu’on se déplace vers le Nord et lorsqu’on travaille dans certaines petites communautés des autres provinces où il y a une grande proportion de membres des Premières nations, d’Inuits et de Métis.
Je pense que les compétences nécessaires pour aider les personnes que nous recevons sont différentes et qu’il faut faire preuve de souplesse. Je reviens tout juste de l’Ontario où j’ai passé une semaine à faire des évaluations dans une communauté où la sécurité alimentaire est un problème majeur, où les enfants ont continuellement faim. Je suis sûre que c’est le cas pour de nombreuses personnes en milieu urbain, mais dans une petite communauté, nous parlons d’une norme culturelle de la faim. Ce n’est pas aberrant ou exceptionnel, c’est une norme dans la communauté : les enfants ont faim. Cela nous incite, en tant que cliniciens, à aborder la pratique différemment. »
Vous avez peut-être remarqué que Mme Bradford et la Dre Gale sont toutes deux « autorisées à exercer en Alberta », même si elles travaillent toutes deux au Yukon. Cela s’explique par le fait que le Yukon est la seule province ou le seul territoire du Canada où les psychologues ne sont pas encore soumis à une réglementation quelconque.
« Le Yukon est la dernière instance canadienne où tout est permis en matière de pratique professionnelle de la psychologie, en l’absence de réglementation, » explique-t-elle.
Si un psychologue du Yukon veut être agréé (et beaucoup le sont), il doit obtenir l’agrément auprès d’un organisme provincial en dehors de son territoire. Selon Mme Bradford, bien qu’il s’agisse d’une solution partielle, elle ne règle pas certains problèmes fondamentaux liés à l’absence de réglementation au Yukon.
« Il n’y a pas d’organisme de réglementation de quelque forme que ce soit au Yukon, de sorte que bon nombre d’entre nous qui exercent la profession de psychologue ont pris l’initiative de demander l’agrément dans une autre province ou un autre territoire. C’est bien, parce que nous passons par le processus de réglementation, mais c’est aussi problématique parce qu’il n’y a pas de réglementation au Yukon, ce qui signifie plusieurs choses. Premièrement, les ordres professionnels auprès desquels nous sommes agréés n’ont qu’une capacité limitée d’appliquer quoi que ce soit en dehors de leur compétence, ce qui est le cas du Yukon. L’autre problème est qu’il y a des gens qui exercent la psychologie et qui ne sont pas agréés au Canada, et ils peuvent le faire parce que ce n’est pas un titre
réservé ici. »
Beaucoup de choses peuvent arriver lorsque des personnes qui ne sont pas tenues d’adhérer à des normes de pratique particulières peuvent se faire appeler « psychologues ». Peut-être n’ont-ils pas satisfait aux critères d’accès à la profession dans un autre territoire. Un psychologue remplit des fonctions délicates et importantes, comme les évaluations diagnostiques. On imagine difficilement à quoi pourrait ressembler cette démarche pour les clients, dont beaucoup sont très vulnérables, lorsqu’elle est effectuée par une personne qui n’a pas les qualifications requises. La Dre Gale voit souvent cela dans son travail.
« En ma qualité de directrice de la psychologie clinique pour le gouvernement du Yukon, des gens me téléphonent pour me demander quelles sont les possibilités de pratique au Yukon. C’est souvent parce qu’ils n’ont pas satisfait aux exigences requises pour avoir l’autorisation d’exercer dans une autre province ou un autre territoire. Peut-être ont-ils passé l’EPPP (Examination for Professional Practice in Psychology) le nombre maximum de fois prévu et n’ont pas pu le réussir, de sorte qu’ils ne peuvent pas obtenir l’agrément dans la province ou le territoire dans lequel ils résident. Des cliniciens qui ont fait l’objet de mesures disciplinaires de la part de leur organisme de réglementation et qui pourraient perdre leur droit d’exercer en tant que “psychologue” ont également pris contact avec moi. Le Yukon est le seul endroit où il n’y a aucune interdiction de ce type de pratique. »
Comment peut-on corriger la situation? Et pourquoi le Yukon est-il la dernière instance au Canada à adopter une réglementation? Mme Bradford affirme que les deux autres territoires du Canada ont un système qui pourrait être reproduit au Yukon.
« Les Territoires du Nord-Ouest et le Nunavut ont conclu une entente avec le College of Alberta Psychologists, qui s’occupe de la réglementation. Nous aimerions avoir cela au Yukon, et les raisons en sont nombreuses. L’une des plus importantes est que nous sommes un petit territoire. La réglementation protège vraiment les gens. Si les choses ne se passent pas bien avec votre psychologue, ou si quelque chose vous semble bizarre, il existe une procédure de plainte. Dans une petite communauté, vous voulez être sûr lorsque vous déposez ces plaintes qu’elles ne seront pas adressées à votre ami, votre voisin, quelqu’un que vous croisez à l’épicerie [comme Jim]. Un grand organisme de réglementation offre cette protection aux habitants des petites provinces ou des petits territoires comme le nôtre. C’est le modèle que nous essayons d’adopter. »
La Psychological Society of Yukon est très petite, en ce sens qu’elle ne compte que 12 membres – des psychologues qui se sont regroupés pour collaborer et défendre les choses qui sont importantes pour eux.
« Notre association a pour objectif de promouvoir l’accès à des services psychologiques de haute qualité fondés sur des données probantes pour les Yukonais, dont beaucoup vivent dans des communautés nordiques éloignées. Bien sûr, Whitehorse est une ville nordique et rurale pour une grande partie du Canada, mais nous parlons de communautés beaucoup plus petites que Whitehorse. Elle a un autre objectif, à savoir défendre la réglementation de la psychologie. Je ne veux pas parler au nom des 12 membres de l’association, mais nous sommes ouverts à toute voie jugée la plus durable pour notre ministère des Services aux collectivités, qui est le ministère du gouvernement qui détient la compétence en cette matière. Personnellement, je pense que nous sommes un groupe trop petit pour nous autoréglementer. Pour ma part, je préférerais conclure un accord avec une instance du Sud. Mais si le gouvernement peut le faire, nous voulons nous associer à lui pour y parvenir. »
Mme Bradford se souvient d’un moment mémorable à l’Assemblée législative du Yukon – oui, il y a des débats à l’Assemblée législative du Yukon qui, bien que peu connus du reste du Canada, peuvent être mémorables!
« Le chef de l’opposition interrogeait la personne qui est censée encadrer la profession de psychologue. Il a dit : “Si je comprends bien, en l’absence de réglementation, je peux mettre ma propre plaque indiquant ‘Services psychologiques de Currie’, est-ce exact?” Le ministre responsable a dit “Oui, c’est ce que je comprends” ».
La question de la réglementation a deux volets. La réglementation de la psychologie instaure une norme de pratique qui garantit que les psychologues qui fournissent des services aux personnes dans les communautés rurales et nordiques le font à l’aide de méthodes fondées sur des données probantes; qu’ils seront guidés par des normes professionnelles qui, au minimum, tentent de ne pas nuire aux personnes avec lesquelles ils travaillent. Le deuxième avantage de la réglementation est de créer un mécanisme de plainte, de sorte que les personnes qui sont lésées par les services fournis disposent de recours et d’une procédure à suivre. La réglementation ne peut pas empêcher tous les préjudices, mais elle fournit un ensemble de règles qui réduisent au minimum les dommages potentiels. Selon Mme Bradford, le problème devrait être assez facile à résoudre.
« De notre point de vue, il n’y a pas beaucoup de raisons de ne pas aller de l’avant. Reagan a consulté des représentants juridiques pour savoir quelle est la façon la plus simple de faire avancer les choses, et cela pourrait être aussi simple qu’un protocole d’entente avec le College of Alberta Psychologists. Nous comprenons qu’il s’agit simplement d’un décret du gouvernement. »
Et pourtant, ce n’est pas encore fait. La Dre Gale nous en dit un peu plus.
« Les obstacles sont les obstacles normaux à l’élaboration des lois par le gouvernement. Notre gouvernement est petit et notre territoire est petit. Les membres de notre société sont reconnaissants pour les travaux de délivrance de permis que le gouvernement fait déjà. Il ne s’agit pas de critiquer les importants efforts en matière de réglementation qui sont déjà en cours – mais simplement que dans une région aussi petite, la capacité en ressources humaines pour ajouter une autre profession est une tâche difficile. Nous pensons que ce n’est pas beaucoup demander, mais dès qu’on élargit l’offre d’un gouvernement, il y a une décision politique qui se prend. Nos efforts de lobbying ont porté leurs fruits lors des élections territoriales du printemps 2021, et les trois partis se sont engagés à réglementer la psychologie, mais c’est le parti dont l’engagement était le plus vague qui a fini par former le gouvernement. Mais nous sommes chanceux que les deux autres partis soient intéressés et que le sujet de la réglementation soit abordé à l’Assemblée législative. »
L’un des avantages supplémentaires en aval de la réglementation est la stabilité. Mme Bradford est au Yukon depuis 19 ans (pas toutes en tant que psychologue agréée) et elle a vu un véritable changement dans le paysage de la santé mentale du territoire.
« Les gens qui travaillent comme psychologues au Yukon, et qui sont agréés, sont ici depuis un certain temps. Nous sommes investis dans la collectivité, nous assurons la continuité des services et nous établissons une relation de confiance qui a la possibilité de se développer au fil des ans, car les gens consultent la même personne. Dans le passé, il y avait un certain roulement, car les personnes qui occupaient certains postes en santé mentale n’avaient pas toutes forcément le même niveau de formation ou de connaissances pour être en mesure de gérer toutes les situations. Elles n’ont peut-être pas mis l’accent, comme la psychologie le fait, sur l’importance de prendre soin de soi et la prévention de l’épuisement. J’ai donc vraiment remarqué ce changement, car il y a maintenant plus de psychologues, et les gens restent, le roulement est réduit et les services sont plus efficaces. »
Ce type d’évolution vers les pratiques exemplaires, les traitements fondés sur des données probantes et la stabilité s’est également produit dans d’autres provinces et territoires. La Dre Hutchings est la première psychologue à travailler aux services de counseling et de psychologie du campus Grenfell.
« Il y a sept ans, lorsque je suis arrivée ici, on a fait pression pour que mon prédécesseur soit remplacé par un psychologue, car on reconnaissait l’importance de la psychologie. Il y a 10 ans, sur le même campus, il n’y avait pas de formulaires de demande ni de procédures pour obtenir le consentement. Les cliniciens qui y travaillaient n’étaient pas agréés par un organisme officiel. Désormais, il existe un processus, une procédure de consentement éclairé et un service plus structuré qui fonctionne dans un cadre réglementé. »
Les personnes vivant dans des communautés éloignées ont des besoins différents de ceux des petites communautés, bien qu’il y ait beaucoup de chevauchements. Par exemple, les communautés qui doivent être approvisionnées par avion peuvent avoir plus de difficultés à avoir accès à la nourriture, ce qui a des répercussions importantes sur la santé mentale. Cela signifie que pour les psychologues qui travaillent dans ces régions, il n’existe pas d’approche unique. Les statisticiens ont débattu pendant des années de ce qui constitue les communautés « rurales », et la Dre Hutchings tente de définir ce que « rural » signifie réellement pour les psychologues.
« Tout ce qui est au Nord est rural, mais tout ce qui est rural n’est pas au Nord. Et il existe des degrés de ruralité différents, bien sûr. Par exemple, Cornerbrook (population d’environ 20 000 habitants), où je me trouve, est une sorte de plaque tournante de la côte ouest de Terre-Neuve. Mais pour toute intervention médicale importante, il faut quand même faire huit heures de route pour aller à St. John’s. C’est un peu subjectif, mais je définis la ruralité principalement par la taille de la communauté, puis aussi par la distance qui la sépare d’un centre plus “urbain”. »
Ou, plus simplement, plus vous êtes en milieu rural, plus vous avez de chances de connaître Jim.

Dr Stryker Calvez

Dr David Danto
Dr Stryker Calvez et Dr David Danto, Psychologie des peuples autochtones
Aujourd’hui, la psychologie est confrontée à la nécessité de modifier ses pratiques pour accueillir les personnes autochtones et attirer des praticiens autochtones, et la Section de la psychologie des autochtones affirme que cela impliquera des discussions importantes et difficiles. Nous avons parlé de la question avec le Dr Stryker Calvez et le Dr David Danto.
Psychologie des peuples autochtones
« Le poisson est le dernier à découvrir l’eau. »
Le Dr Stryker Calvez est un Métis du territoire de la rivière Rouge, qui vit actuellement dans le territoire du Traité 6, à Saskatoon. Autrefois directeur des initiatives pédagogiques autochtones à l’Université de la Saskatchewan, il est aujourd’hui directeur principal, stratégie et habilitation en matière d’équité, de diversité et d’inclusion chez Nutrien. Le Dr Calvez est également le président de la Section de la psychologie des autochtones de la SCP et membre de longue date du Groupe de travail sur le partage des connaissances/comité permanent sur la réconciliation avec les peuples autochtones, aux côtés du Dr David Danto.
Le Dr David Danto est psychologue clinicien de formation, et le directeur du programme de psychologie de l’Université Guelph-Humber. Il a participé à un certain nombre d’efforts visant à autochtoniser et à décoloniser la psychologie, les établissements et les universités. Il est le président sortant de la Section de la psychologie des autochtones.
Eric Bollman est le spécialiste des communications de la Société canadienne de psychologie.
La conversation qui suit a eu lieu le 24 novembre 2021. Depuis, 93 tombes non identifiées ont été découvertes dans un ancien pensionnat de Williams Lake, en Colombie-Britannique. Douze ont été trouvées à Kamsack, en Saskatchewan, et 42, à Fort Perry, en Saskatchewan.
Eric : Je crois savoir qu’il est question de changer le nom de la Section de la psychologie des peuples autochtones pour mieux rendre compte de la nature collaborative du travail – pour se concentrer davantage sur le travail avec les peuples autochtones plutôt que d’en faire une section exclusivement consacrée aux peuples autochtones. Qu’est-ce qui a déclenché cette discussion?
Dr Calvez : Lorsque le nouveau comité de direction a été mis en place il y a environ un an, nous avons réalisé que nous étions majoritairement des non-Autochtones. En tant que communauté de personnes désireuses de soutenir les peuples autochtones du Canada, nous devrons peut-être changer notre façon de fonctionner. Nous devions donc vraiment réfléchir aux mécanismes de la section. La section a été conçue à l’origine pour soutenir les psychologues autochtones du Canada, pour leur donner un espace sûr et une plateforme pour s’exprimer. Bien que ce soit toujours notre mandat, nous voulions aussi reconnaître qu’il y avait un groupe croissant de personnes qui voulaient être utiles et apporter leur soutien. C’est pourquoi nous avons pensé que le nom devait en être le reflet. Plutôt que d’être une section constituée d’Autochtones, ce que nous devions faire, c’était travailler avec les Autochtones et réunir autant de personnes que possible pour créer un environnement sûr, où se trouve tout ce dont ils ont besoin et où discuter courageusement de ce qui leur est arrivé et de la façon de dépasser ce qu’ils ont vécu. Le changement de nom est censé traduire le développement d’une communauté qui veut travailler avec et pour les peuples autochtones. Et je pense que nous le faisons de la bonne façon. Nous avons beaucoup d’alliés, comme David.
Dr Danto : Il y a quelques années, j’ai travaillé avec Stryker à l’élaboration d’une réponse au rapport de la Commission de vérité et réconciliation au nom de la Société canadienne de psychologie et d’Esprits Sains Enfants Sains (connu à l’époque sous le nom de Fondation canadienne de psychologie). Ce qui est ressorti clairement des personnes présentes et des participants à ce processus, c’est que la psychologie n’a pas été une grande amie des peuples autochtones dans le passé, et même encore aujourd’hui, dans de nombreux cas. Cela est dû en grande partie à l’introduction dans les communautés autochtones d’une perspective et d’une approche occidentales externes de la psychopathologie, de la santé, du concept de la famille ou de la personnalité, etc. Et c’est dangereux. C’est ainsi que la psychologie a fait du mal aux gens. Cela s’est produit dans le contexte de l’éducation, de la recherche et de la pratique appliquée. Pour essayer d’appliquer nos principes éthiques sur un pied d’égalité avec tous les habitants de notre pays, nous avons la responsabilité de modifier ces pratiques néfastes et d’utiliser des approches adaptées. Nous devons poser les questions suivantes : « Comment la psychologie peut-elle être une bonne amie des peuples autochtones du Canada? » « Comment pouvons-nous être d’un bon soutien? » Dans bien des cas, je pense que la réponse à cette question est que nous pouvons respecter et reconnaître le fait qu’il existe déjà des méthodes de guérison, une sagesse et des connaissances qui sont utiles, qui favorisent la résilience, la force et le bien-être au sein des communautés. Comme je m’efforce d’apporter mon soutien de cette manière, je me demande ce que je peux faire au sein de ma profession pour encourager celle-ci à respecter davantage les modes de connaissance et de guérison autochtones et à faire preuve d’une plus grande humilité à leur égard. Ce n’est pas que la psychologie ne peut pas ou ne doit pas s’impliquer, mais nous devons décentraliser les approches que nous utilisons, et laisser la communauté locale guider et diriger ce qui a besoin d’être fait.
Dr Calvez : Il y a 1,7 million d’Autochtones au Canada et 38 millions de Canadiens. La (ré)conciliation ne concerne pas nécessairement que les Autochtones. Bien que les conséquences de la colonisation aient été principalement ressenties par les Autochtones, Murray Sinclair affirme que cette dernière a également porté préjudice aux non-Autochtones. Si l’on considère le mouvement actuel en psychologie, qui vise à répondre aux besoins des communautés autochtones du Canada, on constate qu’il n’y a pas assez de psychologues autochtones et pas assez de personnes formées adéquatement pour les soutenir. Nous devons donc réellement travailler avec des alliés, c’est-à-dire des personnes qui sont prêtes à investir du temps pour se familiariser avec les besoins des communautés autochtones et les comprendre, afin de fonctionner en tenant compte de leurs attentes.
Eric : David, vous avez parlé d’« humilité ». Est-ce la chose la plus importante qu’un allié doit posséder lorsqu’il entre dans cet espace?
Dr Danto : Tout ce que nous apprenons en psychologie concerne les façons de penser. Nous parlons de preuves « empiriques », et le mot « empirique » tire sa racine dans le mot « empeirikós », qui signifie « guidé par l’expérience ». Mais une grande partie de la méthodologie utilisée en psychologie a évolué pour se concentrer sur ce qui est objectif et ce qui est quantifiable objectivement. Ce n’est pas une mauvaise chose, mais lorsque nous parlons de l’expérience humaine, cela représente une abstraction de l’expérience. Le terme « empirique » a pris le sens de « quantitatif », mais ce n’est pas la même chose. « Empirique » signifie en réalité « conforme à l’expérience », et lorsque nous quantifions les choses, nous nous éloignons vraiment de cette description de l’expérience. C’est une façon de faire très occidentale. Nous respectons certains types de recherche en psychologie qui ne sont pas forcément adaptés aux conceptions et aux expériences culturelles de l’histoire. Parfois, ces approches occidentales de la connaissance nous enferment dans une ornière, je crois, qui nous fait penser que ce sont les seuls moyens de savoir qui soient valables, testables, vérifiables et concluants. Et cela signifie que nous manquons d’humilité face à d’autres modes de connaissance qui nous semblent inférieurs. Cela nous incite à ne vouloir mener que certains types de recherche dans des contextes qui ne s’y prêtent pas vraiment. Lorsque nous allons dans les communautés et utilisons des méthodes qui ne sont pas très adaptées, nous perdons le lien avec les participants à cette recherche. Ensuite, nous prenons les informations obtenues et nous les utilisons à notre manière, comme tout chercheur universitaire, et cela ne revient jamais à la communauté, la communauté n’a jamais l’occasion de donner son avis parce que les choses ne se font pas dans sa langue. Ce n’est pas une démarche participative ou collaborative, c’est plutôt une approche descendante. Et on se retrouve exactement dans la situation à laquelle nous sommes confrontés. Nous nous retrouvons avec des communautés qui ne font pas confiance aux universitaires et aux chercheurs, parce que, en faisant de la recherche en son sein, ils prennent une chose de plus de la communauté. On a pris la terre, on a pris les droits, et maintenant on prend le savoir, et au profit de qui? Au bénéfice de l’université et du chercheur, et non pour le bien-être de la communauté. Je pense que l’humilité est essentielle pour admettre qu’il y a de nombreuses façons de considérer les choses, et si vous pouvez prendre du recul et reconnaître que votre formation limite vraiment les possibilités qui peuvent être envisagées, plutôt que de les révéler – ce que ces méthodes sont censées faire!
Dr Calvez : Une autre facette de l’humilité culturelle est que l’éducation et le savoir occidentaux proviennent d’une position dominante. Toute la structure hiérarchique du monde occidental est construite de telle sorte que les uns dominent les autres en fonction de leur niveau d’éducation ou de leur groupe culturel. Et cela est intégré dans notre façon de voir le monde. L’humilité culturelle est un processus par lequel nous reconnaissons ce fait et le combattons. Nous devons décortiquer tout cela dans le contexte de la décolonisation, et l’humilité culturelle nous donne les outils nécessaires pour le faire.
Ce qui pourrait être plus important que l’humilité, c’est l’engagement. Le processus de (ré)conciliation va demander un effort énorme et va créer des tensions. Si l’on ne s’engage pas à aller jusqu’au bout de ce que nous tentons de faire, à savoir apporter la guérison aux peuples autochtones et non autochtones et au domaine de la psychologie, nous ne pourrons pas y arriver si les gens ne s’engagent pas à concrétiser leurs intentions.
Eric : Essayez-vous parfois de recruter davantage de personnes pour participer à cette (ré)conciliation, pour en faire des alliés, ou vous concentrez-vous davantage sur la création d’un espace où ces alliés peuvent apprendre et grandir aux côtés des Autochtones?
Dr Calvez : Un aspect important de la (ré)conciliation est que les gens doivent la trouver en eux-mêmes. Le point de départ est non pas de reconnaître les problèmes et de trouver des façons de les résoudre, mais de se connaître soi-même. Et se connaître en relation avec les peuples autochtones et avec une histoire plus que millénaire. Les gens doivent le découvrir par eux-mêmes. Plutôt que de la promotion [aller vers les gens pour les recruter afin qu’ils deviennent des alliés], il faudrait plutôt parler d’attrait [créer un espace où les gens veulent devenir des alliés et aller vers vous]. Nous voulons montrer aux gens que ce que nous faisons n’est pas nécessairement un droit absolu, quelque chose qui doit être fait – même si je pense que c’est vrai. Nous voulons leur montrer que cela profitera à tout le monde, y compris à notre profession. Il y a une bonne façon de procéder : nous en tirons tous des leçons, nous en profitons tous. Je pense que cela se fait non pas en disant aux gens qu’ils doivent le faire, mais en leur montrant les raisons pour lesquelles ils pourraient vouloir le faire. Les personnes qui se joignent à nous sur la base de leurs propres choix sont beaucoup plus à même de faire preuve de l’engagement dont j’ai parlé précédemment et de l’humilité culturelle.
Dr Danto : Dans le contexte postsecondaire, je pense que nous devons nous concentrer sur la création de lieux d’enseignement postsecondaire accueillants et culturellement sûrs, qui favorisent une pédagogie appropriée, réfléchie et critique pour les étudiants autochtones et non autochtones, plutôt que de recruter des étudiants autochtones. Si vous vous efforcez de poser les bonnes questions, de faire preuve d’autocritique à l’égard des processus mis en place et de créer un environnement sûr et culturellement accueillant, les gens seront plus nombreux à vouloir participer à ce que vous faites. Les Autochtones ont eu des expériences vraiment négatives en classe dans le cadre des cours de psychologie. Il y a des mythes sur les prédispositions génétiques, des hypothèses et des préjugés et des partis pris du fait de la longue histoire de la colonisation. J’utilise toujours l’expression « Le poisson est le dernier à découvrir l’eau ». Nous sommes tellement ancrés dans le contexte de la colonisation, qu’il s’agisse de la psychologie, des soins de santé ou de l’éducation, que même avec de bonnes intentions, il nous est très difficile de nous en rendre compte. Nous devons examiner attentivement les espaces dans lesquels nous invitons les Autochtones, car il se pourrait bien qu’ils soient exposés à de nouvelles expériences traumatisantes s’ils sont confrontés à des commentaires erronés, dépassés ou injustifiés. Nous avons le devoir d’être protecteurs.
Dr Calvez : Lorsque vous vous efforcez de recruter des gens uniquement parce que vous voulez plus d’Autochtones dans votre programme, c’est égoïste. Ce qui compte pour vous, ce ne sont pas les Autochtones, leurs besoins ou leurs désirs. Si c’est l’approche que vous adoptez pour soutenir les populations autochtones, vous échouerez à chaque fois. Nous devons modifier l’environnement pour que les autochtones y voient un lieu attrayant et intéressant où se poser. Que les choses soient claires : les collectivités autochtones ont tout autant besoin de professionnels de la santé mentale que le reste de la société. Nous devons nous y mettre maintenant, sans savoir avec certitude si nous allons attirer ces personnes, mais simplement parce que nous devons le faire comme communauté et comme profession. Je pense que nous allons dans cette direction. Beaucoup de changements ont été observés ces dernières années. Il va falloir que cela continue et s’accélère afin d’accroître l’intérêt des gens vis-à-vis de ce travail. Une fois qu’ils seront intéressés, ils se rendront compte que nous n’entravons rien de ce qui existe déjà dans la profession – au contraire, nous élargissons les possibilités et créons un espace plus vaste et plus ouvert pour que davantage de personnes trouvent ce qu’elles recherchent dans la profession.
Eric : Au cours des deux dernières années, on a découvert d’horribles fosses communes sur les sites des anciens pensionnats. Je pense que les Canadiens blancs ont été beaucoup plus choqués que les communautés autochtones, qui nous parlent depuis des années de l’existence de ces fosses communes. Est-ce vrai, et est-ce que cela a changé votre façon de travailler pour la (ré)conciliation?
Dr Calvez : Je pense qu’il est vraiment important de reconnaître que lorsque ces événements se produisent, ils traumatisent à nouveau les peuples autochtones. Nous sommes très affectés, car cela confirme ce que nous défendons depuis longtemps. Que la société canadienne ne nous a pas bien traités, et qu’elle est allée jusqu’à blesser et tuer des enfants pour en attester. Pour une personne issue de ces communautés, c’est l’expérience la plus horrible que l’on puisse vivre, de voir que même ses enfants ne sont pas en sécurité. J’ai des amis qui sont des survivants, et quand cela arrive, ça vous coupe le souffle, et il faut beaucoup de temps pour retrouver la conviction que tout va bien aller. C’est arrivé plusieurs fois cet été seulement. Nous savions que c’était grave, mais je ne pense pas que nous en connaissions l’ampleur. Je me réjouis que des personnes non autochtones réagissent à une situation qu’elles ne connaissaient pas. Réagir ainsi est tout à fait justifié – et il faut le faire. Mais imposer cette réaction aux Autochtones pour les aider à y faire face n’est pas forcément la meilleure chose à faire. Nous avons besoin que d’autres personnes se lèvent et s’expriment afin que nous n’ayons pas nécessairement à être sur le devant de la scène pendant que nous essayons de guérir. Voilà où nous allons en tant que profession. Nous devrions être en mesure de prendre la parole tout en reconnaissant qu’il est tout à fait inadéquat d’aller voir les personnes qui ont été blessées pour valider notre réaction. C’est un processus émergent, et tout cela est nouveau pour nous. Voilà ce qu’est la (ré)conciliation, c’est une idée nouvelle, que nous n’avons jamais vue ou eue auparavant. Nous allons devoir la découvrir et la construire à partir de nos expériences et de notre compréhension. Je pense que l’indignation que nous avons observée dans les communautés autochtones et non autochtones nous montre que nous allons dans la bonne direction parce que désormais, nous savons comment agir lorsque les gens sont extrêmement perturbés. Nous avançons dans la bonne direction en ce sens que nous essayons à présent de nous soutenir mutuellement dans ces processus. Je pense que c’est un moment fort pour nous en tant que communauté et en tant que société. Nous allons devoir faire face à de nombreuses tensions à mesure que de nouvelles révélations seront faites et que nous vivrons de plus en plus cette situation. Le plus important, ce sont les discussions que nous aurons sur ces questions et sur d’autres sujets – et ces discussions risquent d’être difficiles. Nous devons être prêts à discuter de ces questions, à la fois en tant que profession et en tant qu’individu.
Dr Danto : Je pense personnellement qu’un génocide a été commis à l’encontre des populations autochtones de notre pays. Il ne s’agit pas d’un « génocide culturel ». Mais d’un véritable génocide. Nous trouvons des corps sur les sites des pensionnats, et il ne fait aucun doute que nous en trouverons beaucoup d’autres, et que peu importe combien de corps seront retrouvés, beaucoup d’autres ne le seront pas. Je ne suis pas un Autochtone, mais je reconnais que cela s’est produit dans notre pays – qu’ici, dans notre pays, de nombreux Autochtones ont été tués en raison de leur identité. Si nous ne voulons pas l’admettre, nous devons nous demander pourquoi nous refusons de le faire. Pour moi, il est évident que c’est ce qui s’est passé. Pour avancer, cela fait partie de la vérité. Quand on nomme quelque chose, on a la responsabilité d’agir en conséquence.
Eric : Pourquoi les gens utilisent-ils le terme « génocide culturel » même s’il semble évident que ce qui s’est passé est un véritable génocide? Est-ce une façon de minimiser les dommages causés, ou d’utiliser un terme qui n’exige pas autant d’introspection de leur part, ou est-ce autre chose?
Dr Danto : Le système des pensionnats pour Autochtones au Canada a toujours eu pour but de « sauver » l’enfant tout en détruisant son côté autochtone. La rupture des liens culturels avec leur communauté et leur famille. Bien que cela ait pu être l’objectif déclaré du système des pensionnats et des adoptions forcées, les choses sont allées beaucoup plus loin. De nombreuses personnes ont perdu la vie dans ce système, et dans ces établissements financés par le gouvernement fédéral (et dans de nombreux cas, gérés par l’Église), de nombreux enfants ont perdu la vie. Il n’y a pas de doute sur qui en est responsable. Utiliser l’expression « génocide culturel » revient à choisir de définir les préjudices subis en fonction de leur intention, plutôt que de leur résultat. Nous ne ferions pas ça dans une cour de justice. Si votre intention était de harceler, mais pas de tuer, et que vous finissiez par le faire, vous ne seriez pas simplement accusé de harcèlement.
Dr Calvez : Nous devons reconnaître que le Canada, en tant que société, commence à peine à accepter ce qu’il a fait. Comme tremplin, ils ont procédé à un « génocide culturel ». Ils étaient encore persuadés que les pensionnats pouvaient être bénéfiques pour les enfants autochtones. Je pense que puisque nous voyons maintenant à quel point c’était faux, les gens vont accepter le fait que c’était plus qu’un génocide « culturel », que c’était purement génocidaire. Cela dit, je n’écarte pas la malveillance du génocide culturel lui-même. Je suis qui je suis grâce à mes ancêtres, mes croyances, mon identité, parce que tout ce que je suis est lié à la terre. Donc, m’enlever ma conception du monde, mes croyances et tout le reste, revient à me laisser avec rien. Bien que je puisse être là physiquement, je serais un étranger dans mon propre corps. L’utilisation du terme « génocide culturel » a constitué une avancée significative, mais nous sommes désormais plus précis. Nous avons compris les vérités qui l’entourent, et nous pouvons le désigner pour ce qu’il était vraiment, c’est-à-dire un génocide.
Eric : Vous avez dit que des progrès ont été réalisés et que nous allons dans la bonne direction. Pouvez-vous m’en donner un exemple concret?
Dr Calvez : Un grand groupe, auquel participaient David et moi, a élaboré la réponse de la psychologie au rapport de la Commission de vérité et réconciliation. Depuis lors, notre travail n’a pas été mis sur les tablettes. Nous observons l’émergence d’un dialogue stimulant à différents endroits dans le domaine de la psychologie. On assiste à un changement dans les normes d’éthique. Les normes vont changer, nous les renforçons et les améliorons, et nous y intégrons des méthodes qui soutiendront l’autochtonisation de la psychologie et la promotion de la (ré)conciliation. Le CSPP (Conseil des sociétés professionnelles de psychologues) et l’ACPRO (Association des organisations canadiennes de réglementation en psychologie) se mobilisent et redéfinissent la façon dont ils souhaitent voir les organismes de réglementation commencer à aborder ces questions. Et David donnera un atelier pour le CCPPP (Conseil canadien des programmes de psychologie professionnelle) avec Ed Sackaney intitulé « Allyship, Reconciliation and the Profession of Psychology ». Donc, même au sein de notre profession, nous commençons à observer d’énormes changements. Cela ne fait que commencer et les répercussions sur la profession commencent à se faire sentir.
Profils du Mois de la psychologie : Dre Lindsay McCunn et Dr John Zelenski, Environmental Psychology

Dre Lindsay McCunn
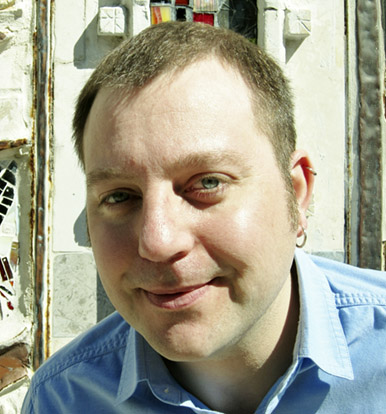
Dr. John Zelenski
Dre Lindsay McCunn et Dr John Zelenski, Environmental Psychology
La psychologie de l’environnement compte deux branches principales. Nous avons parlé à la Dre Lindsay McCunn de la branche de la psychologie de l’architecture (la conception de bâtiments et de pièces pour le bien-être des occupants) et au Dr John Zelenski, de la psychologie écologique (qui s’intéresse aux comportements écologiquement durables par l’intermédiaire de la connexion des gens à la nature).
Psychologie de l’environnement
« Quand je dis que je ne vous juge pas, je pense que je veux vraiment dire “pas plus que les autres.” ».
Je suis un peu nerveux à l’idée que, pendant notre réunion Zoom, la Dre Lindsay McCunn et le Dr John Zelenski puissent juger mon arrière-plan, décidément très encombré. Tous mes appareils électroménagers sont placés sur une tablette derrière moi, ce qui donne l’impression (exacte, il se trouve) que mon bureau à domicile est un coin exigu près de la cuisine. La Dre McCunn et le Dr Zelenski sont des psychologues de l’environnement, c’est-à-dire des spécialistes des espaces que nous occupons et de la manière dont nous interagissons avec eux. Le Dr Zelenski est plutôt gentil et honnête – en tant qu’êtres humains, nous percevons des indices subtils, à partir des espaces de chacun, mais cela n’est probablement pas propre aux psychologues de l’environnement. Nous jugeons tous les arrière-plans Zoom, ne serait-ce qu’un peu.
La Dre Lindsay McCunn est professeure de psychologie à l’Université Vancouver Island. Elle est la présidente de la Section de psychologie de l’environnement de la SCP et la rédactrice en chef adjointe du Journal of Environmental Psychology. Selon elle, les arrière-plans Zoom des gens ou la façon dont ils aménagent leurs jardins ou leurs espaces de vie sont sources de curiosité pour chacun d’entre nous.
« La façon dont les gens s’expriment, organisent leur domicile et placent des objets importants est vraiment intéressante. Sam Gosling a écrit un livre intitulé Snoopologie; il s’agit d’une étude portant sur la façon dont on peut déduire la personnalité et la façon de penser des gens en fonction de la manière dont ils rangent leurs bibelots et leurs affaires dans leur maison et leur bureau. »
La Dre McCunn se spécialise en psychologie de l’environnement et décrit ainsi sa spécialité.
« La psychologie de l’environnement, c’est l’étude des transactions entre les personnes et les lieux. Et j’entends par là beaucoup de types d’endroits – un café, un bureau, une école, un parc, un océan, une montagne. Nous étudions les différentes façons dont les gens interagissent avec leur environnement. De la même manière qu’un psychologue social étudie et analyse les relations et les interactions entre les individus et les autres, les psychologues de l’environnement étudient et analysent les relations entre les personnes et les lieux. Dans mes recherches, je m’intéresse à la façon dont les gens interagissent dans les collectivités et les milieux de travail, en particulier dans les hôpitaux, les écoles et les bureaux. À ce titre, je me penche sur le personnel, principalement, et sur les personnes qui utilisent les environnements d’une manière différente de celle à laquelle on pourrait s’attendre, comme les étudiants et les patients, les enseignants, etc. ».
Le Dr John Zelenski est professeur au département de psychologie de l’Université Carleton. Il est également un psychologue de l’environnement, mais il se spécialise dans un domaine bien différent de celui de la Dre McCunn. On pourrait dire que l’un et l’autre représentent les deux principales branches de la psychologie de l’environnement – la psychologie de l’architecture (Dre McCunn) et la psychologie de l’écologie (Dr Zelenski).
« En plus d’être un psychologue de l’environnement, je me considère aussi comme un psychologue de la personnalité qui se réclame de la psychologie positive. Je me suis beaucoup intéressé à ce que nous appelons le rapport à la nature, ou ce que d’autres appellent “la connexion avec la nature”. Je parle ici des impressions subjectives des gens : font-ils partie de la nature ou la nature est-elle distincte d’eux et n’a pas grand-chose à voir avec leur perception d’eux-mêmes? Je me suis aussi beaucoup intéressé de façon générale par ce que j’appelle un “chemin heureux vers la durabilité”. C’est l’idée que nous savons que la nature est capable de rendre les gens de bonne humeur. La nature est associée au bonheur, tant sur de longues périodes que sur le moment. Nous savons que les gens qui passent beaucoup de temps dans la nature et qui se sentent très liés à la nature adoptent des comportements proenvironnement et écologiquement durables. Au cours des dernières années, nous avons commencé à penser que l’inverse est peut-être vrai aussi. Si l’on peut amener les gens à faire quelques petits gestes pour la nature, en adoptant des comportements écologiquement durables, il serait possible de se servir de cela pour qu’ils se sentent plus proches de la nature et plus heureux de pratiquer ces activités. Nous pensons que les actions en faveur de l’environnement ne doivent pas nécessairement être onéreuses et que nous pouvons les associer à des émotions positives. »
Ce que « consacrer du temps dans la nature » signifie pour chaque personne est subjectif. Il s’agit peut-être de prendre un week-end pour faire de la randonnée dans les collines, de passer une journée à pêcher sur la glace ou simplement d’aller dans son jardin et s’occuper de son potager de radis. Pour la Dre McCunn, cela a entraîné de grands changements depuis le début de la pandémie de COVID-19. Elle nous parle par Zoom dans ce qui semble être un chalet dans les bois. Depuis quelques années, elle et sa famille vivaient dans le centre-ville de Nanaimo, en Colombie-Britannique, en face du service d’ambulance, du service de police et de la caserne de pompiers. Les sirènes ont augmenté considérablement lorsque la pandémie a commencé, leurs habitudes de sommeil ont commencé à en être affectées et ils ont décidé de louer un endroit à la campagne.
« Ce fut en quelque sorte une bonne étude de cas en psychologie de l’environnement, dans la mesure où nous pouvions réaliser ce qui nous stimulait dans notre environnement familial, puis décider comment le modifier pour notre santé mentale. Nous avons donc pensé à déménager dans un cadre naturel plus vaste où nous pourrions avoir un peu plus de contrôle sur les choses qui nous stimulent. Nous avons été très chanceux de pouvoir louer quelque chose à la campagne. C’était intéressant, parce que j’étais très attachée à la maison que nous possédions. L’une des choses que nous étudions, comme psychologues de l’environnement, est le “sentiment d’appartenance” ou un sentiment d’appartenance à un lieu, un sentiment identitaire ou un sentiment de dépendance. Au début de la pandémie, j’ai entendu beaucoup de questions sur la façon dont les gens faisaient face au sentiment de perte qu’ils ressentaient depuis qu’ils travaillaient à domicile. Pas seulement un sentiment de perte en rapport avec des éléments sociaux, mais aussi une perte des moyens habituels par lesquels ils se rendaient à leur lieu de travail. Peut-être prenaient-ils le même autobus tous les jours ou arrêtaient-ils au même café lorsqu’ils se rendaient à l’école ou au travail. Même le caractère physique de l’environnement de bureau ou de la salle de classe elle-même – cet environnement leur manquait. Je me suis donc demandé comment je réagirais lorsque je m’éloignerais de mon environnement familier auquel je m’étais vraiment attaché. Je ne voulais pas me mettre dans une position où je perdrais mon lien avec mon cadre habituel, mais je me suis rapidement attachée à cet endroit et aux caractéristiques naturelles qui l’entourent. Ce fut une belle aventure d’explorer la psychologie de l’environnement de l’intérieur et dans ce contexte. »
Se sentir proche de la nature, ce peut être aussi simple que de pouvoir sortir et toucher à un arbre, ou regarder par la fenêtre une montagne ou une variété d’espèces d’oiseaux. Alors, comment cela peut-il se traduire par des comportements plus respectueux de l’environnement, au moment où le changement climatique est devenu le problème le plus urgent de notre époque? Le Dr Zelenski donne l’exemple que voici.
« Nous avons beaucoup de bonnes preuves circonstancielles et d’études de laboratoire, et nous essayons de les assembler. Quelques programmes ont été prometteurs! Mon ancienne étudiante, amie et collaboratrice, Lisa Nisbet, a collaboré avec la Fondation David Suzuki pour relever le Défi nature 30×30. Ce défi consiste à consacrer 30 minutes dans la nature chaque jour pendant 30 jours. Les personnes qui s’inscrivent à ce défi ont tendance à être plutôt écologistes et déjà très proches de la nature. Mais au cours de ce mois, cette connexion semble se développer. Ce n’est pas un essai contrôlé randomisé, mais il semble que le fait de passer du temps dans la nature donne à ces personnes le sentiment d’être plus proches, ce qui les incite à adopter des comportements écologiquement durables. »
L’écologie est une division de la psychologie de l’environnement (relativement) nouvelle, et elle a sans aucun doute pris beaucoup d’ampleur au cours des 20 dernières années, les changements climatiques étant rapidement devenus un sujet de premier plan pour beaucoup d’entre nous. Le Dr Zelenski n’est pas le seul à avoir évolué dans cette direction.
« L’attention et l’importance accordées à l’aspect écologique de la psychologie de l’environnement semblent s’être accrues au cours des 10 ou 15 dernières années. Je suis venu à la psychologie écologique après mon doctorat, par simple intérêt personnel, et j’ai l’impression d’être l’un des millions de personnes qui ont suivi le mouvement, et ce, pour plusieurs raisons. Les gens semblent de plus en plus manifester des symptômes de dépression, d’anxiété, etc., et la nature semble offrir un répit agréable. De plus, la prise de conscience relative aux changements climatiques ne cesse de croître, car nous en voyons de plus en plus les effets. Et les décideurs politiques souhaitent savoir ce que les sciences sociales peuvent apporter pour résoudre ces problèmes. »
La dimension écologique de la discipline a émané naturellement de la branche traditionnelle de la psychologie de l’architecture, qui existe depuis les années 1960. Selon la Dre McCunn, il existe quelques programmes d’études supérieures officiels en « psychologie de l’environnement » au Canada, mais il y en a plus en Angleterre et aux États-Unis, aux Pays-Bas et en Amérique du Sud. Donc, lorsqu’elle dit aux gens qu’elle est une « psychologue de l’environnement », ceux-ci savent souvent ce qu’elle veut dire.
« Certaines personnes, à juste titre, divisent la dimension de la psychologie de l’architecture et la dimension de la psychologie de l’écologie. Je le fais aussi si je veux expliquer aux gens ce que j’étudie, parce que je suis plutôt du côté de l’architecture. Je travaille avec des ingénieurs, des gestionnaires d’installations et des urbanistes, mais j’ai aussi des collègues, comme John, qui s’intéressent au lien avec la nature et travaillent avec des personnes qui étudient les attitudes et les comportements proenvironnement. L’idée de conservation de la nature est devenue très populaire dans le domaine de la psychologie de l’environnement, sans pour autant prendre le pas sur la dimension architecturale, qui s’intéresse à l’infrastructure des immeubles, etc. En fait, la psychologie de l’environnement a débuté dans le contexte de l’architecture, mais elle s’est largement étendue à son autre volet, qui consiste à poser aux gens des questions sur leur conscience écologique et leur rapport à la nature. »
Les deux branches vont de pair. Pensez à la tendance à construire des bâtiments « verts », avec du chauffage à faible consommation d’énergie, des panneaux solaires, voire un jardin sur le toit.
Selon la Dre McCunn, « Quand un ingénieur me demande : “devrions-nous concevoir ce bâtiment en tenant compte de la durabilité”, il veut en réalité savoir – “les gens vont-ils le remarquer? S’en soucient-ils? Vont-ils apporter des changements à leurs comportements à l’intérieur (et à l’extérieur) de l’immeuble pour cette raison?” Je peux les aider à étudier la manière dont les gens se comportent, travaillent et fonctionnent dans des bâtiments plus (ou moins) durables. J’ai fait une étude dans une école d’études supérieures qui a montré que le fait qu’un immeuble de bureaux soit “vert” ou durable ne signifie pas nécessairement que cela permettra de prédire une forte productivité ou une forte satisfaction. Il est important de garder un œil critique sur ce que l’on attend d’une conception durable et sur ce que l’on n’attend pas. »
Pensez à des espaces dans lesquels vous vous êtes sentis immédiatement à l’aise avec les personnes qui vous entouraient – et d’autres où ce n’était pas le cas. Il est possible que ce ne soit pas les personnes présentes qui en soient la cause, mais la conception de l’espace qui a rendu les interactions plus embarrassantes, ou qui a rendu cette pièce, ce bâtiment ou ce wagon plus confortable. La Dre McClunn précise.
« Si l’on veut qu’un certain espace soit accueillant et confortable, on peut le concevoir pour qu’un certain nombre de personnes puissent s’y asseoir à une certaine distance. Je pense à la conception d’un café, ou un restaurant ou même une salle de classe où l’on veut que les gens s’assoient d’une certaine façon et cohabitent d’une certaine manière.
Je pense qu’il est important d’utiliser différentes méthodes, tout comme les autres psychologues le font. Nous sommes capables d’intégrer une variété de méthodes combinées dans notre travail. Nous utilisons l’observation naturaliste pour observer et voir comment les gens se déplacent et se comportent dans un espace afin de prendre des décisions de conception à partir de nos observations. Nous effectuons beaucoup de sondages et d’entrevues et, à partir de ceux-ci, nous pouvons aider les architectes et les concepteurs à rendre les bâtiments les plus humains possible. Si l’objet du travail clinique et d’autres types d’intervention psychologique est d’aider les gens à se sentir bien, alors la psychologie de l’environnement est tout à fait en phase avec cela. Nous voulons que les bâtiments soient conçus de manière à aider les gens à se sentir aussi bien, motivés, enthousiastes et en forme que possible. »
Le Dr Zelenski jette également un pont entre les deux côtés de la psychologie de l’environnement, et ce, de différentes manières. La collaboration avec des groupes qui font déjà un travail environnemental lui permet de recueillir plus facilement des données, et l’analyse de ces données permet à ces groupes de fonctionner de manière plus efficace et efficiente.
« J’ai collaboré avec un architecte, faisant ainsi le pont entre ces deux composantes de la psychologie de l’environnement. Il était très intéressé par la construction de bâtiments qui donneraient envie aux gens de se comporter de manière écologique. De même, il ne s’agit peut-être pas seulement de l’intérieur du bâtiment, mais aussi des espaces naturels proches du bâtiment qui pourraient encourager ces comportements. Il s’agit de poser une question plus nuancée sur les types de milieux naturels à proximité qui pourraient aider les gens à se sentir mieux, à être plus heureux et plus productifs.
Il y a un petit organisme sans but lucratif qui fournit des trousses d’analyse de l’eau. Il les distribue aux gens, qui les utilisent pour tester la qualité de l’eau à proximité; les gens téléchargent ensuite leurs données dans un genre de base de données participative qui permet de voir si le lac ou la rivière près de chez eux est en bon ou en mauvais état, et comment cela évolue au fil du temps. Il serait difficile pour moi de monter une expérience dans laquelle je distribuerais des tas de trousses d’analyse de l’eau, mais je peux essayer de suivre les personnes qui le font déjà pour voir si cela change leur sentiment de connexion avec la nature, si cela les rend heureux et si cela leur donne envie de faire d’autres choses bonnes pour l’environnement que de simplement tester l’eau. »
Depuis la mise en place de mesures de confinement en raison de la pandémie, nous entendons beaucoup de personnes dire qu’elles apprécient davantage la nature. C’est un moyen sûr de sortir de chez soi. Si on ne peut pas aller dans un centre commercial bondé ou à un concert, on peut toujours aller dans un parc et se promener. Les gens voient la nature comme une source de bien-être et un bon moyen de s’adapter, et certaines études indiquent que la nature est l’une des choses les plus positives que les gens ont ressenties au cours des deux dernières années, où la distanciation physique était imposée. Mais ce lien avec la nature, ainsi que la prise de conscience de la grave menace que représente le changement climatique, crée à certains égards de nouveaux problèmes.
Selon le Dr Zelenski, « Beaucoup de gens parlent d’écoanxiété et le fait que les gens soient de plus en plus conscients des changements climatiques pourrait être une arme à double tranchant. Cela peut donc être motivant – ce qui est un résultat positif, les gens voulant se comporter d’une manière plus écologique – mais certaines personnes pourraient être bouleversées ou inquiètes à tel point que cela créera de nouvelles formes de stress et d’inquiétude qui, chez elles, peuvent être inadaptées. »
L’un des moyens de lutter contre l’écoanxiété, un nouveau mot à la mode dans le domaine de la préservation de l’environnement, consiste à faire connaître les psychologues de l’environnement et à solliciter leurs conseils. Cette sensibilisation accrue se ressent également dans la dimension architecturale, car les contributions des experts de ce domaine sont maintenant perçues par beaucoup comme étant inestimables. La Dre McCunn dit qu’elle a vu ce changement directement.
« Lorsque je rencontre des ingénieurs, des architectes et des urbanistes, je constate qu’ils sont davantage sensibiliés à la psychologie de l’environnement et qu’ils sont tout à fait disposés à travailler avec nous. Lorsque je faisais ma maîtrise, j’ai remarqué que très peu de personnes occupant ces postes voulaient travailler avec un spécialiste en sciences sociales. Plusieurs d’entre eux disaient qu’ils faisaient ce genre de recherche accessoirement, et qu’ils “savaient déjà comment étudier les gens”. Aujourd’hui, ils font appel à moi car ils veulent intégrer cette dimension professionnelle à leur activité ou à leurs processus.
La cognition spatiale, par exemple, est un sujet très habituel en psychologie de l’environnement. Je pense qu’il est important de le mentionner car la population vieillit. Les psychologues de l’environnement consultent souvent les concepteurs pour savoir comment aider les personnes atteintes de démence à s’orienter dans une maison de soins, par exemple. Nous pouvons les observer et les aider avec des pancartes et des symboles, et des moyens d’intégrer leur psychologie dans la conception pour leur faciliter la vie. »
Êtes-vous déjà allé dans un magasin où il y a, sur le sol, un motif très simple qui se transforme un peu à l’approche des toilettes, et un peu plus près de la caisse? Peut-être y a-t-il des rampes d’escalier de couleur vive le long des murs, et le siège des toilettes est-il d’une couleur nettement différente du reste des toilettes. Le magasin est bien éclairé, mais pas trop, car il y a peu de surfaces réfléchissantes et pas de miroirs. Un magasin qui ressemble à ça a probablement été conçu pour être accessible aux personnes atteintes de démence, avec l’aide de psychologues de l’environnement.
Les personnes atteintes de la maladie d’Alzheimer et de différents types de démence sont généralement suivies par une équipe de soins, notamment par un neuroscientifique (voir le portrait de la neuropsychologie clinique présenté plus tôt ce mois-ci). De plus en plus, les psychologues de l’environnement travaillent au sein d’équipes interdisciplinaires plus larges, et les neurosciences elles-mêmes prennent une place plus importante dans la discipline. La Dre McCunn dit qu’elle le constate grâce aux articles proposés au Journal of Environmental Psychology.
« Il y a beaucoup d’articles qui fusionnent les neurosciences et la psychologie de l’environnement. Je fais aussi cela dans mon propre travail – j’ai presque terminé une deuxième maîtrise en neurosciences appliquées, simplement pour approfondir mes recherches dans le domaine des neurosciences environnementales. J’aime chercher à comprendre des concepts tels que “que se passe-t-il dans le cerveau lorsque nous ressentons un attachement à un lieu? Est-ce différent de l’attachement que l’on ressent face à une personne? Que se passe-t-il dans le cerveau lorsque nous rencontrons différents contextes?” Ce sont des questions importantes qui, je pense, sont de plus en plus populaires. »
La psychologie de l’environnement devenant une discipline de plus en plus demandée, l’expertise des personnes travaillant dans ce domaine est appliquée à une variété de sujets sans cesse croissante. La Dre McCunn espère que cette tendance se poursuivra, afin que l’ensemble des compétences de ses collègues puisse être utilisé pour aider à résoudre des problèmes importants.
« Je souhaite que la psychologie de l’environnement fasse partie d’un grand nombre d’équipes très diverses. Bien sûr, les architectes et les urbanistes, mais aussi les cliniciens, les médecins, les neuroscientifiques, etc. Je crois que nous sommes de bons partenaires et nous pouvons ajouter des facettes aux questions de recherche qui peuvent enrichir une réponse et la rendre plus complète. Il est très difficile de tirer des conclusions à partir de quelques variables seulement. La mobilisation des données et de la modélisation dans le domaine de la psychologie de l’environnement peut nous aider à aider les autres à obtenir des réponses plus fiables à de vastes questions de société sur ce qui pousse les gens à agir et à penser de telle ou telle manière. J’aimerais voir la psychologie de l’environnement mettre à contribution son expertise dans toutes sortes de contextes et dans toutes sortes d’équipes. »
Mais soyez rassuré – si un psychologue de l’environnement se retrouve chez vous, il ne jugera pas la disposition de votre argenterie ni l’endroit où vous avez placé votre saucière, à côté du pot de Nutella. Du moins, pas plus que n’importe qui d’autre.

Dre Maria Rogers

Dre Maria Kokai
Dre Maria Rogers et Dre Maria Kokai, Psychologie éducationnelle et scolaire
Bien que les termes « psychopédagogie » et « psychologie scolaire » soient parfois utilisés de manière interchangeable, ils peuvent également faire référence aux deux composantes de la psychologie tel qu’elle se pratique dans le système d’éducation : d’une part, les chercheurs qui élaborent les meilleures pratiques fondées sur des données probantes, et d’autre part, les psychologues scolaires qui mettent en œuvre les résultats de leurs recherches. La Dre Maria Rogers et la Dre Maria Kokai se sont jointes à nous pour nous donner plus d’explications.
Psychologie éducationnelle et scolaire
« C’est comme apprendre aux enfants à nager bien avant qu’ils n’aient la chance de plonger dans la partie profonde de la piscine. »
La Dre Maria Kokai est une psychologue scolaire qui a passé 30 ans au Toronto Catholic District School Board, dont les 14 dernières années comme chef du service de psychologie du conseil. Maintenant à la retraite, elle est la présidente désignée de la Section de la psychologie éducationnelle et scolaire de la SCP. Au cours de sa carrière, elle a constaté un changement dans le domaine de la psychologie scolaire, qui est passée d’une approche axée sur les évaluations et l’intervention auprès des enfants en difficulté à un modèle plus axé sur la prévention, mais cette évolution est trop lente.
« La COVID a vraiment attiré l’attention sur l’importance de la santé mentale et de son traitement sur une base régulière et cohérente. Elle a également mis en lumière les inégalités qui ont résulté des nombreuses fermetures d’écoles et des autres conséquences de la pandémie. Selon moi, une leçon à tirer, pour nous et pour les écoles, est de s’assurer que la santé mentale est abordée de manière préventive, sur une base régulière et intentionnelle – comme nous l’avons fait avec la lutte contre l’intimidation – afin que les enfants apprennent à faire face aux difficultés, à établir des relations et à résoudre les problèmes. Ils peuvent ensuite appliquer ces compétences dans des situations difficiles (ce qu’a été la COVID) afin de s’adapter plus facilement et avec moins de stress.
La psychologie scolaire au Canada est très différente selon les endroits. À certains endroits, les psychologues scolaires offrent toute la gamme de services qu’ils sont en mesure de fournir, tandis que dans d’autres, ils se concentrent sur les évaluations et les problèmes. Ce que nous aimerions voir dans la profession, ce serait de pouvoir fournir des services équitables et accessibles à tous les étudiants, quel que soit leur lieu de résidence, quelle que soit la province, la ville ou la région rurale. Dorénavant, tout le monde devrait avoir accès à des services de façon équitable. Nous ne sommes pas encore là. »
L’accent mis sur la prévention est un élément que les psychologues scolaires souhaitent voir dans tous les conseils scolaires du Canada. Des progrès importants ont été réalisés dans ce sens au cours des 10 dernières années environ, mais il reste encore beaucoup de travail à faire. Maria Rogers est professeure à l’École de psychologie de l’Université d’Ottawa. Elle est la présidente de la Section de la psychologie éducationnelle et scolaire de la SCP.
« Cela met en évidence des problèmes systémiques plus vastes dans ce domaine, dit-elle. Il n’y a pas assez de psychologues scolaires, et il n’y en a pas assez qui sortent des programmes d’études supérieures au Canada. Il n’y a pas assez de ressources affectées à la santé mentale dans les écoles. Nous voulons vraiment adopter une approche préventive en matière de santé mentale qui favorise la réussite scolaire. Certains conseils et districts sont plus en mesure que d’autres (avec de meilleures ressources) d’adopter une approche préventive. Cependant, de nombreux districts scolaires de plus grande taille travaillent selon une approche attentiste, où l’on ne réagit que lorsque l’élève est en échec scolaire, ce qui est vraiment regrettable. Il existe des parallèles avec notre système de soins de santé, où nous attendons souvent que quelqu’un soit vraiment malade pour la prise en charge au lieu de prendre des mesures préventives en amont. »
Certains des retards observés dans la mise en œuvre de programmes de prévention proviennent d’un malentendu fondamental dans le public sur ce que font les psychologues scolaires. Dans l’esprit de beaucoup de gens, la psychologie scolaire se résume aux tests et aux évaluations psychopédagogiques. Il s’agit là d’une description plutôt étroite et inexacte de la psychologie scolaire et de ce à quoi les psychologues scolaires sont formés pour contribuer au système d’éducation. Cette idée trouve son origine dans un modèle beaucoup plus ancien du travail de la psychologie scolaire, qui a vu le jour vers le milieu du XXe siècle. À l’époque, de nombreuses écoles classaient les élèves en fonction de leurs capacités et de leurs déficiences, et elles demandaient aux psychologues scolaires de participer à cette classification en évaluant les élèves pour déterminer leur admissibilité à divers programmes. Toutefois, les psychologues scolaires possèdent un éventail beaucoup plus large de compétences et d’expertise. Et une mauvaise compréhension ou une sous-utilisation de cette expertise peut priver les étudiants d’un large éventail de services qu’ils pourraient autrement recevoir. La Dre Kokai précise.
« Une grande partie du public pense encore que les psychologues scolaires s’occupent principalement des élèves en difficulté. C’est l’une des raisons pour lesquelles les gens parlent beaucoup des listes d’attente pour obtenir une évaluation, qui sont interminables et constituent un problème récurrent. Si les psychologues scolaires avaient la possibilité de se concentrer sur des mesures préventives – prévention et promotion de la santé mentale, et dépistage et intervention précoces des problèmes potentiels d’apprentissage et de santé mentale –, ces problèmes graves pourraient souvent être évités et il serait moins nécessaire de les évaluer. Nous préconisons une gamme complète de services de psychologie scolaire et c’est justement pour cette raison – en passant des problèmes proprement dits à une approche plus préventive, nous n’attendons pas que ces problèmes s’aggravent. »
Certaines régions ont adopté plus rapidement que d’autres une approche axée sur le bien-être des élèves, et la Dre Kokai cite un endroit où cela fonctionne.
« Un organisme appelé Santé mentale en milieu scolaire Ontario, qui joue un rôle consultatif auprès du ministère de l’Éducation et sert de ressource aux conseils scolaires, en est un bon exemple. Il y a environ 10 ans, le ministère de l’Éducation de l’Ontario a ajouté le bien-être des élèves à ses objectifs, en plus de la réussite scolaire. Cela signifie que les écoles sont désormais tenues de se concentrer sur le bien-être et la santé mentale des élèves et de s’occuper des problèmes liés à la santé mentale. Au cours de cette décennie, beaucoup de progrès ont été réalisés en général, et certains progrès ont été accomplis en ce qui concerne l’utilisation des compétences des psychologues scolaires pour soutenir les domaines de la prévention et de l’intervention précoce. »
Le plus grand changement en psychologie scolaire qui s’est opéré au cours des 30 dernières années est la réduction de l’écart entre la recherche et la pratique. Nous avons assisté à un effort systématique accru pour transférer les connaissances des chercheurs aux praticiens, afin de garantir que les psychologues et les autres professionnels de l’éducation qui travaillent avec des enfants puissent accéder aux résultats de la recherche et appliquer ces connaissances dans le cadre de pratiques fondées sur des données probantes destinées aux enfants dans les écoles. La Dre Rogers porte les deux chapeaux, étant à la fois chercheuse et praticienne.
« Je fais de la recherche en psychologie éducationnelle et je suis aussi praticienne. Je pense que, dans l’ensemble, la recherche nous a permis de mieux comprendre les liens entre la santé mentale des enfants et leur apprentissage. À une certaine époque, les deux concepts auraient été considérés comme des éléments distincts. La recherche a réuni ces disciplines pour comprendre comment ces éléments sont indissociables dans la vie d’un enfant. Je constate également que les chercheurs du monde entier sont de plus en plus nombreux à travailler ensemble et à apprendre les uns des autres. Nous mettons en commun les données et les ressources de plusieurs régions du monde afin de favoriser des études à plus grande échelle et dans une perspective plus large. »
La différence entre « psychopédagogues » et « psychologues scolaires » n’est pas aussi simple et ne tient pas à l’idée que le terme « pédagogie » désigne les chercheurs et le terme « scolaire », les praticiens. Dans certaines régions du Canada et ailleurs dans le monde, les termes sont interchangeables. Toutefois, pour la Section de la psychologie éducationnelle et scolaire de la SCP, les termes « pédagogie – recherche » et « scolaire – pratique » sont devenus des raccourcis utiles et sont bien compris par les personnes qui travaillent dans ce domaine. Les chercheurs produisent le savoir, les praticiens appliquent celui-ci. La Dre Kokai explique.
« La psychologie scolaire applique les connaissances scientifiques de la psychologie au milieu scolaire. Les psychologues scolaires appliquent leurs connaissances et leur expertise dans les domaines de l’apprentissage, de la santé mentale, du comportement et du développement de l’enfant pour aider tous les élèves à s’épanouir et à se développer le mieux possible. Ils établissent également des liens avec les personnes les plus importantes dans la vie des enfants – parents, enseignants, collectivités – et les soutiennent. Il s’agit d’un travail très collaboratif qui s’effectue dans l’intérêt de nos enfants et de nos jeunes. »
Cette collaboration a porté ses fruits au cours des dernières décennies, dans la mesure où les pratiques évoluent et où les priorités changent dans le but d’aider au mieux les élèves à maintenir leur bien-être et à s’épanouir dans un cadre scolaire. La Dre Rogers en donne un exemple.
« Au début des années 2000, les chercheurs ont commencé à s’intéresser vraiment au concept d’autorégulation ou de régulation des émotions. Certains chercheurs ont commencé à l’examiner dans le contexte éducatif et à étudier les effets de l’autorégulation sur l’apprentissage. Certains chercheurs, et des personnes orientées davantage vers la pratique, comme Stuart Shanker, ont élaboré des programmes et des outils pour les enseignants sur le thème de l’autorégulation et de son incidence sur le comportement. Cela a permis aux éducateurs de mieux comprendre le concept. »
Les psychologues et les chercheurs ont également collaboré à l’élaboration de nouvelles méthodes d’apprentissage de la lecture pour les enfants. Le SickKids de Toronto est l’un des endroits où une grande partie de ce travail a été effectué. Lorsque la Dre Kokai était la chef du service de psychologie du Toronto Catholic District School Board, celui-ci était l’un des sites expérimentaux du SickKids. Il s’agissait d’un lien direct entre les praticiens de l’éducation et les chercheurs. La Dre Rogers faisait son internat au SickKids il y a une quinzaine d’années, lorsque ce nouveau programme a été lancé.
« Ces dernières années, on a beaucoup parlé de la manière dont nous devrions apprendre à lire aux enfants. De nombreux chercheurs au Canada, principalement au SickKids, ont consacré des années de recherche au traitement phonologique et à la compréhension de la lecture. Ils ont élaboré un programme appelé « Empower », un programme de remédiation pour les élèves ayant des difficultés de lecture, qui est extrêmement rigoureux et fondé sur des preuves. Lorsque je faisais mon internat au SickKids, il y a environ 15 ans, Empower commençait tout juste à être mis en œuvre dans les écoles de Toronto, et il est désormais utilisé dans les écoles de l’ensemble du pays et les enseignants reçoivent une formation sur le programme. »
L’influence des connaissances scientifiques sur la psychologie scolaire n’est qu’une partie de ce vaste système de collaboration. Les psychologues de toutes disciplines collaborent et apprennent les uns des autres. Les compétences transmises par un psychologue scolaire peuvent être utiles à d’autres personnes que l’élève. La Dre Kokai se souvient de l’aide qu’apportait aux familles l’aide donnée à un enfant.
« Si vous êtes un parent, vous utiliserez les mêmes méthodes de communication et de gestion du comportement que celles que nous recommandons aux enseignants. Comment communiquer, comment établir des relations positives avec les enfants, pour les aider à devenir plus indépendants et à composer avec la pression des pairs ou les intimidateurs. Beaucoup de ces compétences s’appliquent également aux adultes. Les relations que vous entretenez dans votre milieu de travail, votre collectivité, et ainsi de suite. »
La Dre Rogers, qui travaille comme psychologue clinicienne en plus de ses fonctions à l’Université d’Ottawa, constate l’influence qu’un tel esprit de collaboration a eue sur tous les aspects de la discipline.
« Une des choses que la psychologie clinique a pu apprendre de la psychologie scolaire est la vision holistique de l’enfant dans ce système. Lorsque nous travaillons avec un enfant dans le cadre de la psychologie scolaire, nous travaillons avec lui dans le contexte de l’environnement scolaire, ou de sa famille, ou du système d’éducation dans son ensemble – souvent les trois. Généralement, la psychologie clinique a tendance à être plus axée sur l’individu, et de grands enseignements sont venus des écoles. »
Vous avez probablement lu et vu en ligne des parents qui se plaignent des « mathématiques modernes ». La manière dont les mathématiques sont enseignées dans de nombreuses écoles est en train de changer et de nombreux parents, en particulier les parents de la génération Y, la trouvent difficile à comprendre – que voulez-vous dire par « on ne retient plus 1 »? C’est ainsi que j’ai appris à calculer et qu’on m’a forcé à le faire, ça a marché pour moi! (Nous faisons bien sûr référence aux membres de la génération Y qui parlent comme des prospecteurs du XIXe siècle.) Il n’y a vraiment pas de « mathématiques modernes ». Les maths ne changent pas. 2 + 2 = 4. n! est égal à n x (n-1)… 1. Ce qui a changé, c’est la méthode d’enseignement, qui met davantage l’accent sur la compréhension des concepts que sur l’obtention de la bonne réponse. Mais le processus qui en résulte est si différent que les parents et les enfants ne se comprennent pas bien lorsqu’ils essaient de travailler ensemble sur les devoirs de mathématiques. La Dre Kokai affirme que, bien que les chercheurs étudient cette question depuis un certain temps, à sa connaissance, les psychologues n’ont été que peu ou pas du tout impliqués dans la mise en œuvre de ces nouveaux programmes.
« Cela semble être un exemple de “cloisonnement”, dont nous parlons parfois en éducation. Les psychologues n’ont pas collaboré à l’élaboration de cette nouvelle méthode d’apprentissage des mathématiques, qui s’est faite de façon cloisonnée. Ce que les psychologues scolaires essaient de faire, c’est de soutenir les élèves ayant des difficultés d’apprentissage pour les aider à acquérir des compétences en mathématiques. Mais je sais qu’il y a des chercheurs, ici en Ontario et probablement ailleurs, qui s’intéressent aujourd’hui aux mathématiques et aux compétences de base en mathématiques. Nous devrons écouter ces scientifiques et ces chercheurs et élaborer un programme de mathématiques qui tient compte des résultats de leurs recherches. »
Il existe beaucoup de bonnes raisons de faire intervenir les psychologues – dans tous les domaines de l’éducation, bien sûr, mais plus particulièrement en mathématiques. La Dre Rogers dit que « contrairement à la plupart des autres matières, les mathématiques comportent un aspect cognitif et psychologique qui fait que l’on a l’impression d’être bon en maths ou de ne pas l’être. Et cette perception de soi semble commencer très jeune. » Aider les enfants à franchir cette étape dès leur plus jeune âge est au cœur même de l’argument de la prévention : plus tôt on peut intervenir, meilleur est le résultat pour l’élève, tant sur le plan émotionnel que scolaire. Et plus il y a de chances qu’il soit capable de nager lorsqu’il arrivera dans la partie profonde de la piscine.

Photo: Enje Daniels Photography
Dre Cranla Warren
La Dre Cranla Warren est la vice-présidente du développement du leadership à l’Institute for Health and Human Potential. Son travail est axé sur le leadership et le mentorat, à la fois auprès des professionnelles et des jeunes filles noires.
« Tu es ma thérapeute depuis nos 13 ans. »
L’amie d’enfance de la Dre Cranla Warren a communiqué avec elle pour la féliciter d’avoir été nommée parmi les 100 femmes noires canadiennes les plus remarquables de 2022 (voir Top 100 Accomplished Black Canadian Women for 2022). Elle affirme ne pas avoir été surprise de l’honneur rendu à la Dre Warren, puisqu’elle aide les gens depuis aussi loin qu’elle se souvienne, en jouant entre autres le rôle de « thérapeute » auprès de ses amis, et ce, dès son plus jeune âge. « Je n’ai jamais douté que tu serais thérapeute, comme tu as été la mienne depuis mes 13 ans! Mais tu as aidé énormément de personnes au fil des ans, dont les vies ont sans aucun doute changé après t’avoir connue. »
Pour la Dre Warren, cette passion transcende le simple fait d’offrir une épaule sur laquelle pleurer ou une oreille attentive. Elle est celle vers qui tous ses amis se tournent pour parler de leurs difficultés ou de leurs problèmes, et elle commence à étudier sérieusement ce qui motive et stimule les gens. Elle commence à lire des ouvrages de psychologie; ils étaient plutôt rares dans les années 1970, mais elle lit tous ceux qu’elle arrive à dénicher, comme les livres de la Dre Joyce Brothers, l’une des seules femmes psychologues renommées à cette époque.
« À l’adolescence, je suis devenue une étudiante du comportement humain, lisant tout ce qui me tombait sous la main, tentant de comprendre tout ce que je pouvais. J’ai réalisé que c’était la voie que je voulais emprunter, mais l’itinéraire fut très sinueux. »
Son parcours débute en travail social, puis elle se dirige vers la psychothérapie, pour finalement aboutir en affaires. À travers toutes ces expériences, la Dre Warren poursuit son étude du comportement humain, trouvant le moyen de nouer des liens avec les gens à toutes les étapes de son parcours. Elle obtient son doctorat en psychologie des organisations. Elle est actuellement la vice-présidente du développement du leadership à l’Institute for Health and Human Potential (IHHP), où elle se spécialise en culture organisationnelle et (comme son titre l’indique) en développement du leadership.
Une large part de son succès en tant que psychologue, professionnelle et personne vient de son habileté à comprendre les autres. Mais ce succès n’a pas été facile à atteindre. En réalité, tout a débuté de façon plutôt chaotique.
« Ne cherche pas à devenir psychologue, ce n’est pas dans tes cordes car tu auras trop d’obstacles à surmonter. Choisis quelque chose de réalisable, comme devenir secrétaire. »
Ce conseil est donné à une jeune Cranla Warren par un conseiller en orientation avant qu’elle ne fasse une demande à l’université, avant qu’elle ne façonne son cheminement de carrière, et avant que le titre de « Dre » ne soit inscrit devant son nom. Ce qui joue en sa défaveur : elle est une jeune fille noire, quelqu’un pour qui la réussite scolaire est peu probable, et pour qui le parcours vers le succès serait parsemé de dizaines d’obstacles inexistants pour les autres. Elle surmonte ces obstacles grâce, dit-elle, à une famille qui la soutient et à une succession de formidables mentors rencontrés non seulement à l’école, mais plus tard, tout au long de sa vie professionnelle.
« Je suis très chanceuse, j’en prends conscience tous les jours. J’ai eu d’incroyables mentors à chaque étape de mon parcours professionnel. Par contre, j’estime aussi que je suis allée activement les chercher. Ce n’est pas tout le monde qui sait comment être proactif à cet égard. Lorsque j’ai été embauchée par une entreprise pharmaceutique, j’avais travaillé dans un hôpital où j’étais clinicienne, mais je n’avais jamais travaillé dans une entreprise. J’avais donné une conférence, quelqu’un l’avait vue, et ils ont adoré ce que j’avais présenté, et ils savaient que j’étais une défenseure de la santé mentale. Ils voulaient une personne comme moi dans leur groupe d’éducation médicale. On m’a mise en contact avec les gens qui occupaient les postes de pouvoir et ils ont dit “Je crois en ce que je vous vois faire et je vais vous aider à monter dans cette entreprise”. Même si éventuellement, cela aurait pu mettre leur carrière en danger. Mes supporteurs, mentors et parrains du monde des affaires ont toujours été des hommes blancs, puisque c’est eux qui détenaient traditionnellement les sièges du pouvoir. »
Cette approche proactive dans les efforts de trouver des mentors et des parrains au sein d’une organisation est une dimension que transmet la Dre Warren à plusieurs professionnelles qui communiquent avec elle précisément à cette fin.
« On communique avec moi assez fréquemment, des femmes noires et des femmes de couleur en particulier, qui disent vouloir apprendre à briser le plafond de verre, tel qu’il existe dans leurs organisations. Elles veulent être des dirigeantes dans leur entreprise. Mais elles se heurtent continuellement à tant d’obstacles systémiques qu’elles ne savent pas comment s’y prendre. Je suis formée en coaching, et j’aide à les coacher en créant un plan de développement distinct de leurs organisations, pour les mener sur la voie du leadership. Cela commence surtout par la connaissance de soi, l’intelligence émotionnelle, votre façon de vous présenter. À partir de là, ça s’étend à l’organisation elle-même. Qui peut agir en tant que mentor pour elles? Qui pourrait être un parrain éventuel? Les femmes noires sont fréquemment ignorées et elles sont invisibles dans plusieurs organisations. »
La Dre Warren a déconstruit son propre parcours afin de cerner où se situent les obstacles, où se concentrent les sièges du pouvoir, et ce qu’il faut pour percer dans les organisations, particulièrement pour les femmes noires.
« À moins de compter sur une personne qui a son mot à dire et prend part aux décisions, et qui plaide en votre faveur, qui est votre champion, votre parrain, qui parle de vous et de vos habiletés quand vous n’êtes pas présente, il est très, très difficile d’avancer. »
Après avoir déconstruit son propre parcours et contribué à créer celui qui permettrait à plusieurs femmes noires de réussir dans les organisations de toute l’Amérique du Nord, la Dre Warren ne s’est pas arrêtée là. L’idée du mentorat, et la valeur qu’il transmet sont au cœur de sa philosophie à tout point de vue. Elle transmet également cette idée aux femmes et aux filles de sa région.
« Je suis mentore auprès des femmes et des filles noires depuis peut-être 20 ans. Au cours de la dernière décennie, très formellement, sous l’égide d’un groupe de coordination appelé Trust 15, où j’ai travaillé avec la fondatrice, Marcia Brown, pour offrir diverses expériences aux personnes inscrites à ses programmes Girls on the Rise et Ladies on the Rise. Elles n’avaient jamais rencontré auparavant une personne qui avait mon niveau d’instruction, et je me rendais à Toronto pour être un modèle, pour être une mentore, pour les soutenir dans leurs efforts de créer efficacement leurs rêves, et par la suite, élaborer un plan pour les réaliser. »
La Dre Warren a mis sur pied un programme qui permet à de jeunes Noires des quartiers défavorisés dont elle est la mentore de se rendre à Stratford, où elle vit, pour assister au célèbre festival du même nom. Elles ont la possibilité de visiter l’entrepôt et de rencontrer toutes sortes de personnes impliquées dans les productions théâtrales, des acteurs aux décorateurs. Elles sortent de cette expérience avec un sentiment nouveau de ce qui est possible. “Vraiment, on peut travailler dans la conception de costumes, la création d’accessoires ou la fabrication de perruques? Vous voulez dire que ça pourrait être de véritables emplois?” »
« Le conseil que m’a donné mon conseiller d’orientation [de ne pas viser trop haut] date des années 1970, et nous voilà dans les années 2020, et les jeunes filles noires entendent toujours le même message. Nous les emmenons donc en autobus à Stratford, en partenariat avec le festival, et nous leur offrons un tout nouveau regard sur le monde. C’est une expérience incroyable que de se promener le long de la rivière et de déjeuner à l’extérieur – des choses que ces filles n’ont généralement pas l’occasion de faire dans leur propre quartier. »
Pour les jeunes filles noires des quartiers défavorisés de Toronto, le simple fait d’être exposées à un monde de possibilités jusqu’ici inconnu peut ouvrir des portes, créer des rêves et des cheminements de carrière qui peuvent leur sembler inatteignables. Pour celles qui se lancent dans la réalisation de ces rêves, la valeur du mentorat reste tout aussi élevée, ce qui reste, à tout moment, une priorité pour la Dre Warren.
« En réalité, c’est grâce à mon mentor-parrain de l’industrie pharmaceutique, un homme blanc qui occupait un poste à la vice-présidence, que je suis maintenant ici à l’IHHP [Institute for Health and Human Potential]. Lorsqu’ils cherchaient quelqu’un, il leur a dit : “Voilà la personne dont vous avez besoin”. C’est toujours une question de savoir “qui est votre champion de l’intérieur?” »
Pour beaucoup trop de femmes et de filles noires au Canada et aux États-Unis, la réponse à cette question est « personne ». Mais plusieurs d’entre elles auront une réponse, si jamais on leur pose la question.
« Qui vous soutient? »
« La Dre Cranla Warren. »

Dre Andrea Howard
Dre Andrea Howard, Psychologie du développement
La psychologie du développement couvre tout, de la petite enfance à la vieillesse, car les êtres humains se développent continuellement tout au long de leur vie. La capacité de changer au fur et à mesure que nous évoluons est appelée « plasticité », et nous en avons parlé avec la Dre Andrea Howard.
« Le plastique ».
Lorsque Walter Brooke a lancé cette phrase mémorable à Dustin Hoffman dans Le Lauréat, nous étions en 1967. Brooke, qui jouait le rôle de M. Maguire, essayait de transmettre sa sagesse au jeune Benjamin Braddock, lui disant où se trouvait l’avenir. À l’époque, les spectateurs étaient au courant des capacités du plastique, mais ils auraient probablement été surpris de voir à quel point cette affirmation était prémonitoire. En 1976, le plastique était le matériau le plus utilisé aux États-Unis et est encore aujourd’hui le plus utilisé dans le monde. Rien n’indique que cette tendance va bientôt ralentir.
En raison de l’omniprésence du plastique, nous avons tous une idée prédéterminée de ce qu’il est, et lorsque nous entendons un terme comme « plasticité », cela peut sembler étrange. Lorsque nous pensons au plastique, nous pensons à des formes plutôt définies – des roues de voiture miniature et des bouteilles de Fresca, des rennes gonflables et d’autres objets. Pourtant, la « plasticité » est un terme utilisé pour indiquer la capacité d’être modelé, de changer, de s’adapter à un nouveau contenant en fonction des circonstances.
La Dre Andrea Howard est une psychologue du développement. Professeure agrégée au département de psychologie de l’Université Carleton et directrice du Pickering Centre for Research in Human Development de la même université, elle étudie le bien-être de la personne pendant les transitions importantes du développement comme le passage à l’âge adulte. Elle parle beaucoup de plasticité.
« Une personne peut à tout moment être modelée ou modifiée d’une façon ou d’une autre. Soit par elle-même, soit par son environnement, ses gènes ou une combinaison de tout cela. C’est un terme qui s’est imposé il y a de nombreuses années et que nous utilisons pour décrire le potentiel. Il n’y a vraiment jamais un moment dans la vie où autre chose ne pourrait pas arriver. Nous disons souvent que les gens partent d’un point commun. Comme deux enfants qui ont eu tous les deux des parents universitaires, ayant des revenus similaires, et des expériences de jeunesse semblables, mais qui ont fini à des endroits très différents. »
Il y a de cela de nombreuses années. Le terme a été utilisé pour la première fois dans les années 1630 et était souvent relié aux arts (sculpture, poterie, etc.). Le terme « plasticité » ne vient pas du mot « plastique », et lui est en fait antérieur de plusieurs siècles. Ils ont plutôt la même racine – « plasticus » en latin ou « plastikos » en grec, ce qui signifie « capable d’être modelé sous diverses formes ». Il est également à l’origine d’autres mots, comme « plâtre » et « plasticine ». La Dre Howard dit qu’il y a deux périodes dans la vie où la plasticité est le plus prévalente – la petite enfance et l’adolescence.
« La psychologie du développement a beaucoup appris sur le développement de l’enfant et les périodes cruciales de la vie pour tirer parti de cette plasticité – et son rôle dans la progression ou le recul d’un enfant par rapport à son potentiel. Les progrès nous ont permis de constater à quel point les trois premières années de vie – mais en réalité les six premières années – sont essentielles. Par exemple, l’école maternelle et les garderies préscolaires basées sur le jeu sont le résultat de ce travail. Nous ne traitons plus les enfants comme des adultes miniatures parce que nous comprenons qu’ils ont des besoins différents, et leur capacité à traiter les informations, à se développer et à s’épanouir est très différente de celle des adultes. La maternelle en Ontario, par exemple, est le reflet de la science du développement de l’enfant. Elle est très différente de celle que je fréquentais quand j’étais plus jeune. »
Pendant la petite enfance, l’enfance et l’adolescence, beaucoup de choses se produisent en très peu de temps. C’est pourquoi le développement des enfants présente un intérêt non seulement pour les psychologues, mais aussi pour les parents, les enseignants, les enfants eux-mêmes et le grand public. Mais la psychologie du développement est un champ d’études qui s’intéresse à toutes les étapes de la vie.
« Je pense que les gens ont l’impression que la psychologie du développement concerne seulement la psychologie de la petite enfance et de l’enfance, et ce n’est pas tout à fait vrai. Tous nos fondements théoriques portent sur les changements qui surviennent tout au long de la vie, et une grande partie des premiers travaux en psychologie du développement sont issus du vieillissement. Plusieurs des chercheurs les plus influents ont étudié le développement de la personne dans la dernière partie de la vie ainsi que le vieillissement cognitif. Aujourd’hui, beaucoup de psychologues du développement importants se concentrent encore sur cette étape de la vie. »
Lorsque j’étais étudiant à l’université, j’avais deux colocataires, Sang et Kent. Une année, nous avions organisé une fête du Super Bowl et mon père était là. Je me souviens d’un jeu où aucune des deux équipes n’avait pu récupérer un ballon perdu, et où le ballon a fini par sortir des limites du terrain. Mon père s’est tourné vers moi et m’a dit : « Aucune des deux équipes n’a été foutue de ramasser ce maudit ballon! » C’est à ce moment-là que j’ai senti que j’étais entré dans l’âge adulte. Papa me parlait comme à un ami, avec un juron tout à fait banal! En s’adressant à moi! Je suis un adulte! La Dre Howard étudie cette transition vers l’âge adulte, qui, selon elle, se présente différemment selon les personnes.
« Devenir adulte, cela ne se fait pas en un rien de temps. Les enfants commencent à se rapprocher de l’âge adulte dès leur naissance, mais beaucoup de choses se succèdent rapidement lorsque les adolescents arrivent à la fin du secondaire, apprennent à conduire à 16 ans et deviennent majeurs à 18 ans. La plupart des gens considèrent que la transition vers l’âge adulte commence à la fin de l’adolescence et se termine à la fin de la vingtaine, mais ce processus est très fluide et très individualisé. Certaines personnes auront l’impression d’avoir atteint l’âge adulte plus tôt que d’autres lorsqu’elles assument des rôles conventionnels comme occuper un emploi à temps plein, être chef de famille et payer ses propres factures.
Il y a beaucoup de gens de 60 ans et de 70 ans qui disent « Vous savez, je ne me sens pas vraiment comme un adulte ». Ou ils ont l’impression que d’une certaine manière ils le sont, mais que d’une autre manière, ils ne le sont pas. Il n’y a pas de règles officielles prescrivant le moment où un individu « devient » un adulte. Il n’existe pas de définition juridique de l’âge adulte, et lorsqu’un individu a 19 ans, il est majeur et a des droits légaux. Mais sur le plan du développement, nous sommes plus intéressés par la façon dont les gens se perçoivent et perçoivent les autres relativement à l’âge adulte.
Au cours des 30 dernières années, dans les pays occidentaux – les pays ayant plus de ressources – on a commencé à s’intéresser à des indicateurs moins tangibles de l’âge adulte. Comme la capacité de prendre soin de soi-même de manière générale et d’être responsable de ses actions, ou de se distinguer de ses parents dans une relation interpersonnelle, tandis qu’auparavant les marqueurs étaient le mariage, la maternité, le travail à temps plein, l’indépendance financière, et ainsi de suite. Mais ces choses ont beaucoup moins d’importance, et beaucoup de personnes qui n’ont pas nécessairement franchi toutes ces étapes du développement de la personne se sentent tout à fait adultes. Depuis longtemps, nous constatons que les gens se soucient davantage des caractéristiques intangibles pour déterminer si on a franchi le cap de l’âge adulte. »
L’adolescence, au moment où l’on s’approche de l’âge adulte – quelle que soit la définition que l’on donne à ce terme – est un moment clé du développement. Encore une fois, c’est parce que c’est une période où la plasticité est très forte. Selon la Dre Howard, le développement du cerveau des adolescents a fait l’objet de beaucoup de recherches au cours des dernières décennies.
« L’une des contributions les plus importantes de la psychologie du développement concerne la perception que nous avons des adolescents et la nécessité de les traiter comme des enfants plutôt que comme des adultes. Cela vient en grande partie de notre compréhension du développement du cerveau entre 10 ans et 25 ans. La neuropsychologie du développement nous a permis de comprendre que le cerveau continue de changer de façon très importante, et que l’adolescence en particulier est une période d’activité extrêmement élevée et de changements neurologiques. Cela est semblable à l’enfance pour ce qui est du niveau d’activité. Au fil des ans, notre façon d’envisager la prise de décision et la prise de risque chez les adolescents, ainsi que le fait de faire preuve de bon ou de mauvais jugement dans des situations intenses, a changé. Nous savons très bien qu’un jeune de 16 ans peut raisonner aussi bien qu’une personne de 30 ans pendant une situation calme sans implication émotionnelle – une situation qui ne nécessite pas une prise de décision rapide sous pression. Comme voter, par exemple. Mais le jeune de 16 ans n’est pas aussi doué pour décider s’il faut ou non brûler un feu rouge. Lorsqu’ils se trouvent avec leurs amis, les adolescents ont tendance à choisir des comportements plus risqués. C’est une constatation qui a aidé la société à décider de la manière de traiter les adolescents dans les situations décisionnelles et judiciaires. »
Donc, si les jeunes de 16 ans sont tout aussi capables que les adultes de prendre une décision comme choisir pour qui voter, pourquoi ne peuvent-ils pas voter? La Dre Howard poursuit.
« À une époque, les personnes de 18 ans ne pouvaient pas voter non plus, mais comme il fallait plus de gens pour faire la guerre, on a abaissé l’âge du vote. La décision d’interdire aux jeunes de 16 ans de voter n’a pas de base développementale. La question de savoir si notre pays choisira cette voie a davantage à voir avec la volonté des adultes de céder une partie du contrôle de la prise de décision à des personnes plus jeunes. Les études sur le développement des adolescents indiquent qu’un jeune de 16 ans devrait être en mesure de prendre une décision aussi éclairée qu’un adulte. »
Et pourtant, les jeunes de 16 ans ont le droit de conduire. Ceux d’entre nous qui ont, à un moment ou à un autre, été (ou ont eu) des adolescents se souviennent peut-être des primes d’assurance incroyablement élevées que nous devions payer – beaucoup plus élevées que celles des adolescentes, et astronomiquement plus élevées que celles de nos parents ou nos grands-parents. Je me souviens du moment où l’Ontario a instauré son programme de « délivrance graduelle des permis de conduire ». J’étais juste un peu trop jeune pour être exempté, et cela a ajouté une étape supplémentaire (et deux années supplémentaires) au processus d’obtention du permis de conduire. Cela a augmenté les dépenses, mais pas autant que les primes d’assurance. La Dre Howard dit qu’il y a une bonne raison à cela.
« Si votre assurance automobile était si chère lorsque vous aviez 17 ans, ce n’est pas parce que des psychologues du développement ont dit aux assureurs qu’il devait en être ainsi, mais parce que les compagnies d’assurance reconnaissaient que les adolescents étaient impliqués dans beaucoup plus de collisions que les autres conducteurs. Et cela est dû aux différences liées au développement. Le programme de délivrance graduelle des permis de conduire contribue grandement à faire des conducteurs novices des conducteurs plus prudents. »
En plus de modifier sa façon d’aborder les enfants en bas âge et les adolescents à l’adolescence, la psychologie du développement s’est orientée au cours des trois dernières décennies vers les études longitudinales. Les pionniers très influents dans le domaine se concentraient autrefois sur l’idée que le développement de la personne présentait une grande universalité. Jean Piaget, par exemple, est à l’origine de la célèbre théorie des « stades » du développement, qui divise la vie humaine en quatre stades distincts. Selon la Dre Howard, nous voyons les choses un peu différemment aujourd’hui.
« À une certaine époque, les questionnements portaient sur l’idée que les enfants atteignent un stade et ne peuvent pas ensuite régresser, et que tout le monde est assez semblable à chaque stade de leur développement. Nous savons désormais que cette façon de voir les choses est un peu trop figée. Notre domaine s’est éloigné des théories du développement par stades. En ce qui concerne la conception des études, je pense que le changement le plus important a été le passage des enquêtes et des expériences ponctuelles à la collecte de données sur une longue période (données longitudinales). Les données longitudinales ont toujours existé, mais elles sont devenues une composante beaucoup plus importante de la psychologie du développement qu’elles ne l’étaient, disons, dans les années 1990. Aujourd’hui, quand on fait une étude, on s’attend presque à recueillir des données sur des mois, des années, voire des décennies. »
Nous commençons à voir apparaître des études longitudinales plus importantes en raison de la COVID. La plupart d’entre nous ont été invités à participer à un sondage quelconque concernant leur santé mentale au cours des deux dernières années, leurs habitudes quotidiennes et leur perception de la pandémie à différents moments pendant cette période. La Dre Howard ne fait pas exception, même si, pour l’une de ses études, elle affirme que la COVID a fini par être davantage une parenthèse intéressante qu’un point central.
« En 2019, nous avons recueilli des données auprès d’étudiants de premier cycle de l’Université Carleton, des jeunes de 16 à 19 ans en première année. Ils sortaient tout juste de l’école secondaire et entamaient la transition vers l’université et nous pensons qu’une transition aussi importante que celle-là offre de grandes possibilités de changement. Nous avons recueilli des données quatre fois pendant la première année scolaire, pour voir si les indicateurs de bien-être que nous mesurions évoluaient d’un mois à l’autre. Des problèmes comme la dépression et l’anxiété ont tendance à s’aggraver entre le début et la fin du semestre, ce que nous avons constaté à maintes reprises. Ce qui a été vraiment utile pour nous dans cette collecte de données, c’est que nous avons fini par recueillir certaines données au moment où les confinements commençaient en raison de la COVID à la fin de l’année scolaire. Le fait de recueillir des données à différents moments me donne un ensemble de données qui me permettent de déterminer comment les personnes appartenant à la population étudiée se portaient avant et pendant la transition vers la nouvelle situation imposée par la pandémie. Cela permet de voir non seulement comment les groupes de personnes en général évoluent dans le temps, mais aussi comment les individus eux-mêmes évoluent par rapport à leurs propres références au fil du temps. »
La COVID a bien sûr été, pour nous tous, le principal sujet de discussion au cours des deux dernières années, mais depuis une dizaine d’années, ce sont les médias sociaux qui occupent une place prépondérante. LinkedIn a été lancé en 2003, suivi rapidement par MySpace. Twitter a été lancé en 2006, et en 2008, Facebook a dépassé MySpace pour devenir le site le plus populaire. Aujourd’hui, nous avons aussi Pinterest (2010), Instagram (2010), Snapchat (2011), TikTok (2017), la liste est longue et le paysage est sans fin. Il s’agit d’un sujet important dans le domaine auquel s’intéresse la Dre Howard, à savoir la transition vers l’âge adulte.
« On discute beaucoup sur la mesure dans laquelle l’utilisation des médias sociaux est problématique pour la santé mentale et le bien-être général des jeunes. Les psychologues du développement tentent de rappeler au monde que les choses qui se trouvent sur les téléphones ne sont pas des activités statiques que l’on fait, mais des contextes dans lesquels la vie se passe. Lorsque les enfants vont à l’école, ils découvrent tout un environnement avec des personnes autour d’eux qui peuvent les influencer, et ils influencent également l’environnement et les autres personnes par leur présence. Par exemple, une plateforme Instagram est un contexte de développement dans lequel les gens évoluent, ce qui est nouveau par rapport à ce que c’était il y a dix ans. Ainsi, aborder l’utilisation des médias sociaux sous l’angle du développement nous aidera à comprendre non seulement si le fait d’être sur la plateforme est bon ou mauvais pour la personne, mais aussi quels types d’expériences qui se vivent sur cette plateforme peuvent être malléables – en vous influençant d’une manière positive ou en générant des risques et des expériences négatives. »
À la fin de 2021, une étude menée par la plateforme Facebook elle-même a marqué l’actualité mondiale. La principale manchette était que Facebook savait qu’Instagram (dont il est propriétaire) a un effet négatif profond sur l’image corporelle des jeunes filles. Pour ajouter au caractère sensationnel de cette nouvelle, l’étude a été révélée par un lanceur d’alerte, et il semble bien que Facebook ait tenté de la dissimuler. Mais, selon la Dre Howard, les psychologues du développement ne croient pas aux titres sensationnels, aux résultats de l’étude, ni même à la validité de l’étude elle-même.
« Cette étude a vraiment posé problème, car elle n’est pas bien faite. Facebook a été accusé d’avoir caché cette recherche, mais il s’agissait d’un travail de très faible qualité qui ne montre pas du tout qu’Instagram est néfaste pour les adolescentes. Mais parce qu’elle a été enterrée et qu’une personne a lancé l’alerte à son sujet, elle a beaucoup de visibilité aujourd’hui. Dans le public, les parents et les politiciens s’inquiètent souvent du fait que les médias sociaux nuisent à nos adolescents. Du point de vue du développement, ce n’est pas la bonne question à poser. Les adolescents sont sur les réseaux sociaux, tout comme les adultes et certains enfants. Alors, que se passe-t-il dans ces environnements qui soit bon et mauvais? Qu’est-ce qui permet d’améliorer le potentiel de développement des individus et qu’est-ce qui l’entrave? L’étude révélée par le lanceur d’alerte a rassemblé des jeunes qui avaient répondu à des questions sur l’image corporelle et qui manifestaient une image corporelle négative, et leur a demandé à quel point ils pensaient qu’Instagram avait nui à leur image corporelle. Influencer les participants en leur disant : “C’est une des raisons pour lesquelles tu as une mauvaise image corporelle. À quel degré cette raison est-elle mauvaise?” n’est pas un bon moyen d’obtenir une réponse qui puisse nous renseigner sur la plateforme. Mais plus encore, quelque 70 % de ces filles, même après avoir été “conditionnées”, ont déclaré que ce n’était pas un problème, ou que cela les avait aidées. Mais on a mis l’accent sur les 30 % de filles qui ont dit que le fait d’être sur Instagram les faisait se sentir moins bien dans leur peau, ce qui a fait la une des journaux. Donc, la méthodologie de l’étude était mauvaise, la façon de poser la question était mauvaise, et les résultats ont été mal interprétés. Les psychologues du développement recommanderaient d’aborder cette question très différemment. »
Les médias sociaux ont certes des avantages et des inconvénients, et ont entraîné des développements positifs ainsi que des effets négatifs, plus médiatisés. Selon la Dre Howard, on peut dire la même chose de pratiquement tous les domaines étudiés par les psychologues du développement.
« Ce qui rassemble les gens sous la bannière de la psychologie du développement, c’est le fait qu’ils adhèrent à un cadre théorique définissant la façon dont ils considèrent la durée de vie. Les gens changent continuellement tout au long de leur vie. Le développement de la personne comporte toujours une part de plasticité et de malléabilité et les gens peuvent toujours changer. Il existe un potentiel de croissance positive ou négative en tout temps. Ce qui module notre expérience est ce qui se passe dans notre environnement. Nous adoptons une perspective théorique très large sur la façon dont les gens évoluent tout au long de leur vie, ce qui permet de rapprocher les psychologues qui étudient la petite enfance dans cette perspective et ceux qui étudient le vieillissement et la démence en fin de vie. »
La plasticité est toujours là. Et nous l’appellerons toujours « plasticité », même si nos conceptions modernes laissent entendre qu’un nom différent pourrait évoquer une représentation plus appropriée de sa mécanique. Cela dit, nous ne sommes pas malléables au point de la confondre avec le plastique.

Dr. Elizabeth Hartney

Dr. Mari Swingle
Dre Elizabeth Hartney et Dre Mari Swingle , Électrophysiologie quantitative
Aujourd’hui, le Mois de la psychologie met en vedette l’électrophysiologie quantitative, c’est-à-dire l’étude de l’activité électrique du cerveau. Nous avons parlé avec la Dre Elizabeth Hartney et la Dre Mari Swingle de la valeur réelle des détecteurs de mensonges et des bienfaits de l’ennui.
Électrophysiologie quantitative
Aucun mensonge détecté
Il y a une scène dans un épisode de Seinfeld où Jerry est interrogé à l’aide d’un détecteur de mensonges par un sergent de police qui ne le croit pas lorsqu’il lui dit qu’il n’a jamais regardé un épisode de Place Melrose. Grâce aux conseils de George (« ce n’est pas un mensonge si tu crois que c’est vrai! »), il s’en sort plutôt bien jusqu’à ce que l’anxiété prenne le dessus et qu’il craque sous la pression, admettant être vraiment accro à Place Melrose. Pour en savoir plus sur la « féminophobie » présente dans cette scène, voir l’article sur l’orientation sexuelle et l’identité de genre présenté plus tôt dans le cadre du Mois de la psychologie!
Nous avons tous déjà vu des scènes semblables à la télévision et dans les films, où les gens ont des électrodes attachées à leurs doigts et à leurs mains, et où la machine quantifie les réponses données aux questions posées. Je pense que la plupart d’entre nous savent aujourd’hui que la machine ne mesure pas vraiment l’honnêteté mais plutôt l’anxiété. Et bien qu’elle ne soit pas très utile dans son but présumé – la détection des mensonges –, cette technologie est en fait très utile pour détecter l’anxiété! C’est le domaine de l’électrophysiologie quantitative.
La Dre Mari Swingle est psychologue clinicienne, chercheuse, auteure et conférencière. Elle a un doctorat en psychologie et une maîtrise en éducation, et elle a un certificat en neuroélectrophysiologie. Elle est la trésorière de la Section d’électrophysiologie quantitative de la SCP. Elle décrit la discipline de la façon suivante :
« Nous lisons l’activité électrique du cerveau, ce qui nous révèle beaucoup de choses. Nous pouvons lire à partir des niveaux supérieurs du cortex et obtenir beaucoup d’information, et nous pouvons aussi aller très profondément dans les structures et les circuits du cerveau. Il faut de l’équipement extrêmement perfectionné pour faire cela, et il faut des cliniciens extrêmement perfectionnés pour lire tout cela. »
La Dre Elizabeth Hartney, la présidente de la Section d’électrophysiologie quantitative, figure parmi ces cliniciens extrêmement perfectionnés. La Dre Hartney est psychologue agréée en Colombie-Britannique et elle possède une certification en neurofeedback et en biofeedback (deux formes courantes d’électrophysiologie quantitative).
« Nous sommes agréées par la BCIA, qui signifie Biofeedback Certification International Alliance. L’organisme offre la certification en biofeedback dans le monde entier. Le biofeedback englobe quelques sous-disciplines. Celle dans laquelle Mari et moi travaillons le plus étroitement est le neurofeedback EEG (électro-encéphalogramme) – mais nous pratiquons aussi le biofeedback avec capteurs périphériques, qui recueille d’autres informations biologiques pertinentes (p. ex., la réponse ectodermique – un mot compliqué pour désigner la sueur ou les cycles respiratoires) ailleurs dans le corps. Nous pourrions donc poser des électrodes sur le bout de vos doigts, sur la paume de votre main, pour lire la variabilité de la fréquence cardiaque ou la conduction cutanée. Il s’agit en fait de tout ce que l’on voit dans les détecteurs de mensonges à la télévision – qui ne sont pas vraiment efficaces pour détecter les mensonges, mais qui le sont pour détecter l’anxiété. L’anxiété est l’une des choses avec laquelle nous travaillons beaucoup. »
Le biofeedback est une thérapie qui permet de prendre conscience des fonctions de son propre corps et de mieux les contrôler. Il peut être utilisé pour aider les personnes présentant divers symptômes, allant du syndrome du côlon irritable aux effets secondaires de la chimiothérapie. La Dre Harney poursuit :
« Nous travaillons avec les gens pour obtenir des informations sur leur respiration, leur rythme cardiaque, leur tension artérielle, toutes sortes de phénomènes qui peuvent être psychosomatiques et impliquer à la fois l’esprit et le corps. Il y a des thérapeutes qui se spécialisent dans d’autres domaines, comme l’incontinence urinaire. Dans ce cas, l’approche utilisée vise à apprendre à l’individu à prendre le contrôle de son corps et de son cerveau – et dans certains cas, de sa vessie! »
Comme si les mots « électrophysiologie quantitative », « neurofeedback » et « biofeedback » n’étaient pas si rébarbatifs, les cliniciens spécialisés dans cette discipline ont tendance à en ajouter quelques-uns. Comme la physiologie, qui décrit aussi leur travail! Il y a la neurophysiologie, qui s’intéresse aux signaux du cerveau. Il y a aussi la physiologie générale, qui s’intéresse au corps en entier, y compris au cerveau. Selon les circonstances, les cliniciens spécialisés en électrophysiologie quantitative parleront uniquement du corps, uniquement du cerveau, ou des deux en même temps. La Dre Swingle parle des dimensions différentes que cela peut avoir.
« Beaucoup de recherches se sont faites sur ce que nous appelons la “cartographie cérébrale”. Alors, comment lire l’électricité et que nous dit-elle? Nous travaillons à partir de bases de données cliniques ou normatives. Les données normatives sont des mesures prises à partir du cerveau de personnes qui n’ont pas de symptômes ou de diagnostics déclarés. Elles ne souffrent pas de TDAH, de dépression, de psychose, etc. Nous regardons à quoi ressemble le cerveau dans ce cas, et nous pouvons ensuite traiter les personnes atteintes de TDAH, de dépression ou de psychose, et les aider à retrouver leur état normal (ou typique). Ce qu’Elizabeth et moi faisons principalement relève de l’autre volet, à savoir travailler à partir de bases de données cliniques. Cela signifie que nous mesurons l’activité électrique du cerveau des personnes qui souffrent réellement d’anxiété, d’insomnie, de difficultés scolaires, et ainsi de suite. Nous entraînons ensuite le cerveau à s’éloigner de cette mesure. »
Cela consiste principalement à exploiter les processus en cours dans certaines zones du cerveau et à en augmenter ou en diminuer la force. Cela peut être efficace pour traiter la dépression, l’anxiété, le TDAH et d’autres pathologies. Dans les situations où le cerveau lui-même a subi des dommages, le traitement est très différent.
Comme l’explique la Dre Swingle, « lorsque nous avons affaire à des AVC très graves ou des différences structurelles du cerveau, nous cherchons alors des connexions différentes [ce qui est souvent appelé neuroplasticité – la capacité du cerveau à compenser les parties endommagées en apprenant à utiliser d’autres parties pour accomplir les mêmes fonctions]. La majorité du travail que nous faisons vise à améliorer l’efficacité des connexions existantes. Certaines ne sont pas assez puissantes et d’autres, trop puissantes. Les travaux précurseurs de Davidson en sont un bon exemple. Il a étudié l’équilibre entre les lobes frontaux, le lobe gauche et le lobe droit. Il a découvert que si les activités électriques corticales étaient supérieures de plus de 15 % sur un lobe par rapport à l’autre, cela indiquait presque toujours une dérégulation émotionnelle. »
Montrer plus facilement le cerveau
Le domaine de l’électrophysiologie quantitative a beaucoup changé au cours des vingt dernières années, notamment en raison de l’avènement de l’ordinateur personnel et d’une plus grande puissance technologique. Pour une discipline qui dépend énormément de la technologie, cela a été une aubaine, mais a également rendu les pathologies, et leur traitement, beaucoup plus complexes. La Dre Harney réfléchit à cette évolution.
« En fait, les choses sont devenues plus faciles – mais aussi beaucoup plus compliquées – avec l’expansion des ordinateurs personnels. Ils ont rendu beaucoup plus divertissant le processus de réception et de renvoi de la rétroaction à partir du cerveau et vers le cerveau. Mais il y a là un problème. Avant d’avoir des ordinateurs, des psychologues comme nous utilisaient des lumières qui s’allumaient ou des sons qui résonnaient lorsque le cerveau accomplissait ce pour quoi nous l’entraînions. C’est la partie “rétroaction ou feedback” des termes “neurofeedback” ou “biolofeedback”. Et cela fonctionnait très bien! Aujourd’hui, nous avons des jeux d’ordinateur sophistiqués, des casse-tête et des vidéos qui s’allument et s’éteignent selon ce que fait le cerveau et nous disposons de tableaux impressionnants, qui nous permettent d’observer la fréquence des ondes cérébrales des gens à plusieurs endroits différents à la fois ».
La Dre Swingle donne un exemple précis du genre de travail qu’elle et la Dre Hartney pourraient réaliser pour un client. « Nous pourrions vouloir augmenter une onde cérébrale à un endroit particulier du cerveau dans un but bien précis. Par exemple, nous voulons augmenter les ondes thêta [un type d’ondes cérébrales] à l’arrière du cerveau parce que lorsque le niveau d’ondes thêta à l’arrière du cerveau est plus élevé, la tolérance au stress est plus grande. Nous pouvons utiliser cela pour aider à combattre l’insomnie, l’anxiété, les dépendances, tous des types de troubles qui pourraient bénéficier du calme du cerveau. Nous attachons une électrode à un endroit très précis et demandons à l’individu d’interagir avec un ordinateur. Une façon très simple de procéder est de faire sauter un criquet à l’écran lorsque les ondes thêta se déplacent par petits mouvements. Disons que nous avons affaire à une jeune personne qui souffre d’anxiété extrême et qui a besoin d’aide pour se calmer. Tout ce que nous faisons, c’est lui demander de faire sauter le criquet. Les petits enfants ne demandent pas comment on fait ça, pourquoi on fait ça. Ils disent simplement “OK”. Il est donc très facile de travailler avec les enfants! Dans les coulisses, nous observons les formes d’onde pures, les amplitudes et les rapports afin de voir la fréquence thêta monter, et nous manipulons les seuils pour faciliter ou compliquer le saut du criquet. Ce que nous faisons, c’est donner à cet enfant le contrôle pour augmenter les ondes thêta par lui-même. Quand on montre au cerveau un moyen plus facile de faire quelque chose, il le fait. »
Cultiver l’ennui
Pendant que je rédige le présent portrait, il y a derrière moi un téléviseur en sourdine. À l’écran, Équipe Canada est en train de jouer pour la médaille d’or contre les États-Unis aux Jeux olympiques. Mon téléphone est à côté de moi et émet constamment des notifications – Jonathan Stea vient tout juste de partager mon gazouillis, CTV Ottawa a lancé sur Instagram une vidéo en direct des manifestations au centre-ville d’Ottawa. Je n’ai pas joué à Words With Friends avec mes amis depuis trois semaines, et ils veulent que je sache que je leur manque. À tout moment, je dois arrêter de taper, car les notifications par courriel bloquent l’écran, et j’en ai reçu 14 depuis que j’ai commencé à écrire. La Dre Swingle a écrit un livre intitulé i-Minds: How Cell Phones, Computers, Gaming, and Social Media are Changing our Brains, our Behavior, and the Evolution of our Species qui traite justement de ce genre de choses.
« Un problème qui se pose dans notre discipline est que les choses sont devenues si sophistiquées qu’elles ne sont plus aussi efficaces, explique-t-elle. Un criquet qui saute pendant cinq minutes, c’est amusant. Un criquet qui saute pendant quarante minutes, c’est ennuyant! Et les enfants retournent à leurs jeux vidéo incroyablement évolués et spectaculaires. Nous obtenons donc de très bonnes données pendant la séance, mais le cerveau ne change pas de façon permanente. Lorsqu’on travaille avec des enfants, surtout ceux qui ont des difficultés d’attention, les écrans doivent être un peu ennuyants pour que le traitement fonctionne. C’est devenu une sorte de conflit intérieur dans notre discipline. »
Comment les choses ont-elles changé au cours des dernières décennies? Les enfants trouvent-ils le criquet ennuyant aujourd’hui parce qu’ils sont habitués à passer beaucoup de temps devant un écran interactif et à être davantage stimulés? S’ils avaient été exposés à cet exercice en 1988, auraient-ils trouvé le criquet divertissant plus longtemps? La Dre Swingle répond « oui » et « non ».
« Il y a 20 ans, on pouvait maintenir l’attention plus longtemps avec des stimuli moindres, mais c’était tout aussi ennuyant! Le problème est plus important maintenant parce que les nombreuses interactions avec la technologie influencent le développement du cerveau des enfants. Beaucoup d’enfants ne savent pas comment “supporter la monotonie” parce que tout se passe à un rythme effréné dans leur vie. Si l’enfant fait une heure de neurothérapie par semaine, mais consacre 20 heures aux jeux vidéo par semaine, le jeu l’emportera probablement. Et cela fait exactement le contraire de la neurothérapie; le cerveau s’entraîne à ne répondre qu’à l’excitation. »
Si vous vous entraînez sur un tapis roulant ou un rameur pendant 30 minutes par jour, c’est sûrement très bon pour vous, mais si vous passez le reste de la journée à ne manger que de la poutine et des coupes au beurre d’arachide, les effets du rameur seront probablement très diminués, et il est peu probable que vous obteniez les résultats que vous recherchez.
En même temps, si vous allez au centre de conditionnement physique tous les jours pendant trois mois et travaillez avec un entraîneur personnel pour trouver le programme d’entraînement qui vous convient, vous serez peut-être capable de maintenir le niveau de forme physique que vous désirez par la suite en n’y allant qu’une fois par semaine. C’est l’objectif de l’électrophysiologie – que les changements opérés dans votre cerveau fassent partie de vous-mêmes et se maintiennent après le processus.
Selon la Dre Hartney, « l’objectif ultime, c’est que votre client apprenne à changer d’état sans l’aide de la rétroaction. Or, nous constatons que les jeunes voient la thérapie par biofeedback comme une forme de divertissement et ne comprennent pas nécessairement qu’il s’agit d’un processus éducatif. Nous essayons de leur apprendre à changer d’état, mais parce qu’ils sont inondés de gadgets et d’animations, il est beaucoup plus difficile pour eux de généraliser ce qu’ils ont appris pendant une séance hors de l’environnement thérapeutique. »
Sur la valeur de l’ennui
Chaque vendredi soir, ma famille et moi faisons une soirée de jeux sur Zoom. Nous jouons à un jeu sur nos téléphones et nous partageons tous un même écran. Les progrès rapides de la technologie réalisés au cours des dernières années ont rendu possibles des choses extraordinaires, et c’est formidable de pouvoir nous retrouver de cette manière, en particulier pendant une pandémie où d’autres méthodes de communication ne sont pas nécessairement disponibles. Mais je remarque que les enfants abordent cela un peu différemment des adultes. Pendant que nous attendons le chargement du jeu, ils jouent à un autre jeu sur leur téléphone. Ou, bien que ce ne soit pas leur tour, ils distribuent les cartes sur la table de jeu ici, à la maison; ils peuvent donc jouer à un autre jeu pendant les 90 secondes d’interruption du jeu. La Dre Hartney explique pourquoi cela est de plus en plus courant.
« Nous sommes d’un âge où le fait de s’ennuyer était normal lorsque nous étions enfants. Si nous allions voir nos parents pour nous plaindre de nous ennuyer, ils nous donnaient une corvée ou nous disaient de nous occuper par nous-mêmes. Nous avons grandi avec l’idée que les choses étaient un peu ennuyantes et que nous devions chercher nous-mêmes comment nous amuser. La génération actuelle n’a tout simplement pas le même genre de référence. »
Comme la Dre Hartney, la Dre Swingle adore l’ennui!
« Toute la créativité et toutes les innovations émanent de l’ennui. Si vous ne vous ennuyez pas, vous n’avez pas l’occasion de développer votre curiosité, vous n’avez pas le temps de remarquer les choses par vous-même, de les assimiler, de voir les modèles, etc. Veuillez noter que la curiosité personnelle (interne) (générée par l’ennui) et l’exploration qui suit sont très différentes de la curiosité générée par un divertissement (externe) (générée par une excitation externe ou un divertissement externe plutôt que par l’éveil interne). Nous allons bien au-delà de nos travaux en électrophysiologie quantitative, mais ces éléments sont intrinsèquement liés. »
Avant d’aller trop loin au-delà de l’électrophysiologie quantitative, nous allons en rester là.
Alors, ennuyez-vous, les amis!
Profils du Mois de la psychologie : Dre Jen Theule et Dre Cathy Costigan , Psychologie de la famille

Dr. Jen Theule

Dr. Cathy Costigan
Dre Jen Theule et Dre Cathy Costigan , Psychologie de la famille
Le domaine de la psychologie familiale est aussi dynamique et complexe que les familles elles-mêmes. Nous avons parlé avec Jen Theule et Cathy Costigan des familles, des définitions et des vastes « systèmes » qui les englobent tous.
« Aucune personne saine n’est totalement indépendante. »
À la fin du troisième film de la saga du Parrain, Michael Corleone (Al Pacino) meurt seul dans une cour, ayant, semble-t-il, coupé tous les liens avec sa famille et l’entreprise familiale. Cependant, en y regardant de plus près, il ne peut pas avoir complètement coupé les liens avec sa famille – c’est elle qui a fait de lui ce qu’il est et qui a façonné la trajectoire de sa vie entière. En fait, même la cour où il est assis lorsqu’il s’effondre et meurt se situe dans la villa appartenant à Don Tommasino, un ami de la famille Corleone.
Dans notre culture, nous avons tendance, la plupart du temps, à considérer les gens comme des individus. De cette façon, nous considérons un individu sain séparément de sa famille et nous pensons rarement à lui dans ce contexte élargi. Les psychologues de la famille, quant à eux, pensent constamment à ce contexte. La Dre Jen Thele est professeure agrégée à l’Université du Manitoba et enseigne aux programmes de psychologie scolaire et de psychologie clinique; elle est également la présidente de la Section de psychologie de la famille de la SCP. Selon elle, beaucoup de choses que nous vivons dans notre vie quotidienne sont le résultat de la psychologie de la famille.
« Permettre aux parents de garder leur bébé avec eux dans la chambre d’hôpital après sa naissance au lieu de le garder à la pouponnière, comme cela se faisait autrefois, c’est un sujet qui intéresse la psychologie de la famille. Inviter les membres de la famille aux consultations médicales et aux discussions avec le médecin. Les réunions parents-enseignants. Tout ce qui permet d’impliquer la famille et d’impliquer plus de personnes aux discussions, c’est le genre de choses que les psychologues de la famille encouragent. »
Quand Amerigo Bonasera vient rendre visite à Don Corleone le jour du mariage de sa fille pour lui demander un service, il n’y a pas que lui et le parrain dans la chambre. Il y a d’autres personnes, dont le consigliere de la famille, Tom Hagen (Robert Duvall). Les décisions ne sont pas prises par le parrain seul. Il accorde de l’importance à la parole des personnes les plus proches de lui.
D’une part, il y a les découvertes apportées par la science et l’étude des familles, et d’autre part, il y a les applications de ces découvertes dans la gestion de la dynamique familiale, souvent, mais pas toujours dans le cadre d’une thérapie.
« Pour moi, la psychologie de la famille a deux volets, dit la Dre Theule. Premièrement, il s’agit de l’étude de “la famille” – les relations parents-enfants, les relations amoureuses, les familles multigénérationnelles, les groupes d’amis proches, ainsi de suite. Comprendre le fonctionnement des familles, autant les grandes unités familiales que les sous-systèmes qui les composent. Et deuxièmement, c’est l’application des connaissances ainsi acquises aux interventions. La thérapie familiale, le counseling matrimonial, par exemple. »
La Dre Cathy Costigan est professeure au département de psychologie de l’Université de Victoria.
« J’enseigne ce que nous appelons la “psychopathologie du développement”, ou les problèmes de santé mentale des enfants et des jeunes. J’enseigne cela à partir d’une optique familiale forte, qui consiste à comprendre le développement normal et anormal des enfants. J’enseigne également la thérapie familiale aux étudiants diplômés, laquelle implique des moyens d’intervention au “niveau des systèmes”. Nous ne voyons pas les problèmes comme “il y a quelque chose de défectueux chez l’enfant que nous devons réparer”; nous examinons plutôt les relations entre les différents membres de la famille et leurs modes de communication. Ce sont ces problèmes “systémiques” plus larges qui sont susceptibles de générer du stress dans une famille ou de le perpétuer. Il se peut que ce soit l’enfant qui exprime le stress vécu dans la famille, par exemple, en se comportant mal à l’école ou en faisant des crises à la maison, mais pour aider l’enfant, on doit aider toute la famille. »
La Dre Theule et la Dre Costigan parlent beaucoup de « systèmes ». C’est une façon d’être un peu plus général et inclusif lorsqu’on parle de la famille. Il ne s’agit pas seulement de la famille nucléaire composée de deux mères et de deux enfants – le terme peut également désigner la famille élargie formée par les grands-parents et les cousins, ou un groupe d’amis très soudé, ou encore une grande commune hippie de Californie, qui existe depuis les années 1970.
Comme l’explique la Dre Thele, « Tout le monde est touché par divers systèmes. Que ce soit les gens avec qui vous travaillez, avec qui vous vivez ou avec qui vous êtes lié, ou votre groupe d’amis. Toutes ces entités fonctionnent de façon similaire aux familles. La plupart des gens considèrent une famille d’accueil comme une unité familiale, mais le reste du monde aura probablement du mal à répondre à des questions du genre : “est-ce que mon colocataire est un membre de ma famille?” Dans l’ensemble, la société considère toujours la “famille” comme une famille nucléaire – une mère et un père et de un à quatre enfants. Mais dans certaines communautés, les familles sont définies de manière plus large et sont plus nombreuses. Ainsi, lorsque j’utilise le terme “système”, les gens acceptent davantage l’idée que la famille peut comprendre matante et grand-maman – ou même les colocataires. »
Quelle est la taille exacte de la « famille » Corleone, dans la saga du Parrain? Se limite-t-elle aux membres de la famille immédiate – Vito, Michael, Fredo, Sonny et Connie? Inclut-elle les époux et les épouses? Les enfants? Tom Hagen, adopté officieusement par les Corleone à un jeune âge, est-il vraiment un membre de la famille? Qu’en est-il de tous les « membres » de la mafia? Sont-ils officiellement admis dans l’organisation ou dans la famille elle-même? En fait, où finit la « famille » et où commence l’« entreprise criminelle »?
Chaque communauté et chaque culture définissent la « famille » de manière un peu différente. Ce sont ces définitions de la famille, et les différences culturelles de ce qui constitue une famille saine, qui intéressent la Dre Costigan.
« Ces temps-ci, mes travaux de recherche portent surtout sur les familles d’immigrants et de réfugiés. J’étudie les moyens par lesquels les familles exploitent les ressources et les forces qui sont en elles lorsqu’elles passent d’un pays à l’autre, ainsi que les divers traumatismes qui ont pu accompagner leur périple vers le Canada. Comment font-elles pour maintenir des liens familiaux solides dans un contexte où les différences culturelles sont nombreuses et où chaque membre de la famille peut être amené à s’adapter à la culture canadienne par des moyens différents et à des rythmes différents, ce qui peut créer des tensions au sein de la famille? »
Ces tensions se manifestent notamment dans le cas des parents qui sont ici au Canada, mais dont les parents et la famille élargie vivent encore dans leur pays d’origine. Avec la technologie mondialisée d’aujourd’hui, ils sont plus connectés que jamais aux membres éloignés de leur famille. Parfois, cette connexion met les parents dans une situation difficile. Dès lors, il se peut que les attentes de leurs propres parents quant à la façon d’élever les enfants contrastent beaucoup avec celles de leurs propres enfants qui grandissent au Canada. C’est ce genre de tension que la Dre Costigan constate souvent dans les familles avec lesquelles elle travaille.
La psychologie de la famille, en tant que discipline, évolue dans cette direction depuis un certain temps. Elle met un accent accru sur les variations culturelles dans les familles. On s’éloigne de la prémisse implicite selon laquelle le contexte canadien (la famille blanche aux valeurs occidentales) constitue le modèle d’une famille qui fonctionne bien. Au lieu de cela, on met l’accent sur ce à quoi ressemble une éducation parentale efficace ou une bonne communication au sein de la famille. Bien sûr, cela varie beaucoup selon la culture. Le fonctionnement sain d’une famille n’est pas le même pour tout le monde, et le fait de le reconnaître a constitué un grand pas en avant pour la psychologie de la famille au cours des dernières décennies. La Dre Costigan en donne un exemple :
« Dans la culture occidentale blanche, la relation maritale entre conjoints, qu’ils soient de même sexe ou de sexe opposé, est au premier plan. Les conjoints sont les chefs de la famille et il devrait y avoir des limites claires autour de la prise de décision dans la famille, et les enfants n’en font pas vraiment partie. Nous pourrions considérer comme un problème le fait que les enfants soient trop au courant des problèmes des adultes ou trop impliqués dans les décisions des adultes. Dans certaines cultures, cependant, la relation qui prime est la relation parent-enfant. On peut souhaiter que les enfants contribuent à la famille à un degré beaucoup plus élevé que celui auquel on s’attend dans la culture canadienne dominante. Remplir ces obligations familiales est vraiment une force, et cela fait partie d’une adaptation saine de l’enfant dans cette optique culturelle. »
Le travail des psychologues spécialisés dans le domaine de la famille peut porter sur chaque moment de la vie, de l’arrivée d’un nouveau-né dans la famille jusqu’à la planification des soins de fin de vie d’un parent ou d’un grand-parent. Selon la Dre Costigan, dans toutes ces situations, bien que l’approche puisse être très différente, les principes fondamentaux demeurent les mêmes.
« Les principes fondamentaux des systèmes de fonctionnement familial entourant la communication et la résolution de problèmes présentent un intérêt à chaque phase de la vie. Comment aider les familles à exprimer ce qu’elles pensent de manière respectueuse et utile, comment les aider à résoudre des problèmes de façon à ce que tout le monde se sente entendu? Souvent, dans notre culture, les enfants majeurs vivent leur vie de façon assez indépendante. Ensuite, lorsque leurs parents vieillissent, ils doivent interagir les uns avec les autres et échanger beaucoup plus, dans un contexte très chargé émotionnellement. Certaines vieilles blessures résultant des interactions familiales peuvent resurgir et perturber vraiment ce processus. C’est un exemple de moment privilégié, survenant plus tard dans la vie, où les psychologues pourraient vouloir s’impliquer pour aider une famille à traverser cette phase difficile de la vie. »
Ou, peut-être, les psychologues pourraient vouloir s’impliquer immédiatement après le décès d’un patriarche de la famille. Cela pourrait éviter des désaccords et des trahisons futurs, et faire en sorte que Fredo ne scelle pas son sort en prenant parti contre la famille. Je crois que peut-être. Le Parrain présentait une dynamique familiale plutôt difficile, et peu de psychologues.
Au cours des deux dernières années, un nouveau défi a été posé aux familles et, par extension, aux psychologues de la famille qui les aident. Non seulement la pandémie a fait augmenter les problèmes de santé mentale, mais elle a également rendu plus difficile l’accès au soutien qui aurait pu alléger certains de ces problèmes.
Comme l’évoque la Dre Theule, « Les deux dernières années ont imposé une forte pression sur les familles qui vivent sous le même toit. La pandémie a fait disparaître une grande partie du système familial et du soutien qui vient avec, comme les grands-parents. Nous disposons de beaucoup d’innovations technologiques, mais ces innovations ne viendront pas prendre soin de vos enfants lorsqu’ils sont malades ou changer les couches à votre place. Elles ne répondent pas aux besoins du quotidien. Selon moi, de nombreuses recherches menées au cours des deux dernières années ont révélé beaucoup de choses à l’extérieur du domaine de la psychologie de la famille. Les psychologues s’y attendaient tous, mais de voir le stress que subissent les enfants, les personnes handicapées et les personnes âgées – les personnes qui comptent un peu plus sur le système familial – l’impact sur ces personnes du stress des aidants. Ainsi, les gens se sont rendu compte que, en se concentrant sur les adultes qui aident les personnes qui ont besoin de soins supplémentaires, on aide les personnes qui ont besoin de soins supplémentaires. Pour toute personne qui dépend des autres, un aidant est vraiment important et je pense que cela peut être un changement dans l’ensemble de la communauté. »
Encore une fois, la Dre Thele parle de systèmes. L’avenir de la psychologie de la famille réside dans l’intégration des connaissances actuelles des experts dans un système beaucoup plus vaste et complexe que nous pouvons désigner sous le nom de “famille” ».
« La psychologie de la famille ne fait qu’effleurer la surface de l’ensemble du système. Nous savons très bien comment examiner les parties du système – ce qui se passe dans un couple, la dynamique entre un parent et un enfant, et ainsi de suite – mais une famille n’est pas seulement un ensemble de petites parties, elle est plus grande que la somme de ses parties. Alors, comment faire pour examiner et mesurer quelque chose d’aussi complexe qu’un système familial? Chaque famille est différente par sa taille, sa culture et sa dynamique. C’est là que nous tentons d’aller – regarder les grands systèmes. Des recherches sont actuellement menées sur la dynamique des triades, comme un parent et deux enfants ou deux parents et un enfant. Mais la complexité qu’ajoute le passage de deux à trois personnes est telle qu’il s’agit déjà d’un énorme changement. »
Imaginez un diagramme que vous avez dessiné sur une feuille de papier. S’il y a deux personnes (deux points sur le diagramme), une seule ligne peut être tracée entre elles. Ajoutez une troisième personne (troisième point) et trois lignes peuvent maintenant être tracées entre les individus. Une personne de plus – trois fois plus complexe. Ajoutez un quatrième point, et cinq lignes peuvent être tracées. Et ainsi de suite. Vous pouvez donc imaginer à quel point cela doit être difficile de travailler avec un système familial entier, dans lequel neuf, dix, voire trente personnes sont impliquées. Comprendre ces systèmes pourrait être la tâche colossale à laquelle la psychologie de la famille devra s’attaquer dans les prochaines années.
La Dre Theule et la Dre Costigan seront de la partie – comprendre l’incroyable complexité des systèmes familiaux et mettre au point des interventions et des traitements plus efficaces. Toutefois, il reste peut-être une question à laquelle elles ne pourront répondre. Qu’est-ce qui a, au juste, convaincu Francis Ford Coppola et Al Pacino que faire le troisième film du Parrain était une bonne idée?
 Dre Donna Ferguson
Dre Donna FergusonFévrier, c’est le Mois de l’histoire des Noirs, et la SCP met en vedette, tout au long du mois, des psychologues noirs contemporains. La Dre Donna Ferguson est psychologue clinicienne et travaille pour le Programme travail, stress et santé du CAMH; elle exerce également en pratique privée, où elle effectue, entre autres choses, des évaluations de l’admissibilité au statut de réfugié et des évaluations des besoins humanitaires.
« C’est agréable de recevoir les commentaires d’un avocat qui vous dit que votre rapport a vraiment été déterminant dans la cause qu’il défendait. »
Il est rare que les avocats communiquent avec la Dre Donna Ferguson pour lui faire une quelconque mise à jour. Mais quand c’est le cas, elle éprouve un immense plaisir car elle sait qu’elle a joué un rôle décisif dans la situation d’un réfugié qui demandait l’asile au Canada. La Dre Ferguson est psychologue clinicienne et travaille pour le Programme travail, stress et santé du CAMH; elle exerce également en pratique privée, où elle effectue, entre autres choses, des évaluations de l’admissibilité au statut de réfugié et des évaluations des besoins humanitaires.
« Il se peut qu’un avocat ait un client venu de son pays d’origine, où il a peut-être subi un traumatisme, dit-elle. Il s’agit parfois d’un traumatisme causé par un conjoint ou un époux, ou d’un traumatisme encore plus grave, par exemple de la violence politique. Dans certains cas, le client pourrait avoir peur pour sa vie. Dans le cadre de la demande de statut de réfugié de son client, l’avocat peut demander une évaluation psychologique pour établir un diagnostic. »
Le diagnostic posé par la Dre Ferguson et son équipe ne sert pas à décider si une personne restera ou non au Canada, ou si sa demande de statut de réfugié est légitime. Les évaluations ne sont pas des tests de polygraphie comme ceux que l’on voit parfois dans les films. La Dre Ferguson et son équipe évaluent plutôt la personne et font des recommandations en fonction de ce que celle-ci a vécu et de ce qu’elle pourrait vivre dans le futur.
« Si par exemple, un diagnostic de syndrome de stress post-traumatique (SSPT) était posé, nous monterions un dossier pour expliquer ce qui s’est passé et, si possible, faire en sorte qu’elle reçoive un traitement ici, au Canada. Et nous pourrions dire que si elle était renvoyée dans son pays d’origine, ses symptômes s’aggraveraient, et nous ferions des recommandations à cet égard. »
Dans le contexte de la pandémie, ces évaluations sont de plus en plus rares – les réaliser sur des plateformes virtuelles s’est avéré difficile, surtout lorsqu’un traducteur doit être ajouté à la démarche. Durant cette période, la Dre Ferguson s’est concentrée davantage sur son travail au CAMH, où elle s’est éloignée de sa spécialité d’origine, la dépendance au jeu, pour s’intéresser davantage à la santé mentale au travail.
« Je participe à de nombreux groupes de travail au CAMH en tant que responsable de la santé mentale en milieu de travail et je donne des conseils aux chefs d’entreprise. Nous travaillons pour le compte de la Commission de la sécurité professionnelle et de l’assurance contre les accidents du travail (CSPAAT), et les personnes que nous voyons sont principalement de leurs clients. Au cours des 20 dernières années, j’ai beaucoup appris sur les milieux de travail! Ce qu’il faut faire et ne pas faire pour que les chefs d’entreprise s’occupent de leurs employés, et comment faire pour que les gens se sentent bien au travail. »
Encore une fois, la pandémie a un peu bouleversé les choses. Des années d’apprentissage des tenants et aboutissants de la culture d’entreprise, des meilleures pratiques et de l’analyse des données issues de toutes sortes d’études n’ont préparé personne au passage soudain à des activités commerciales virtuelles.
« Une grande partie de ce travail est en cours. Les gens ont dû faire preuve de créativité très rapidement lorsqu’il a fallu faire face à la pandémie, pour créer un environnement virtuel. Le CAMH l’a fait de nombreuses façons – notre programme est entièrement fonctionnel en mode virtuel. Nous avons restructuré nos outils d’évaluation pour qu’ils soient virtuels, nos programmes de traitement individuels et de groupe, et toutes nos réunions sont devenues virtuelles. Le CAMH dans son ensemble, et pas seulement notre programme, a vraiment fait beaucoup de choses de manière virtuelle, et les connaissances acquises ont permis d’aider d’autres organisations. »
Qu’il s’agisse d’aider les entreprises dotées d’une culture de longue date à s’adapter à la pandémie tout en veillant à la santé mentale de leurs employés ou d’aider les gens issus de cultures très différentes à trouver de l’aide ici, au Canada, le programme de la Dre Ferguson reste chargé. Et le travail qu’elle accomplit, quelle que soit sa forme, reste gratifiant!

Dr. Brigitte Sabourin

Dr. Nicholas Carleton
Dre Brigitte Sabourin et Dr Nicholas Carleton, Psychologie clinique
La psychologie clinique est la branche de la psychologie à laquelle pensent la majorité des gens quand ils entendent le mot psychologue. Mais nous avons largement dépassé le cliché patient-allongé-sur-un-divan, et la pratique clinique est entrée dans le monde virtuel en ligne. Nous avons échangé avec la Dre Brigitte Sabourin et le Dr Nicholas Carleton sur la situation actuelle de la psychologie clinique.
Au début de sa carrière, Sigmund Freud se spécialise en hypnose. Il hypnotise ses patients pour les amener à s’ouvrir sur leurs symptômes, diminuant supposément leur gravité. Il est novice en la matière, a peu d’habiletés, ses patients doivent donc être le plus détendus possible : il leur demande de s’allonger sur un divan, pendant qu’il fume son cigare en leur disant qu’ils ont très envie de dormir.
Éventuellement, il découvre qu’il peut être encore plus efficace que les patients parlent simplement de leurs symptômes dans une atmosphère détendue. Il abandonne l’hypnose, mais conserve le divan (et le cigare). D’autres psychanalystes qui ont suivi les traces de Freud ont également adopté le divan, à tel point que dans les années 1940, l’Imperial Leather Furniture Company de New York devint une entreprise richissime grâce aux « divans de psychanalyse ». Il y a plus de 70 ans, le psychanalyste au cigare et au divan austère devient en quelque sorte un « mème », un « mème » qui persiste à ce jour.
Que seraient les dessins humoristiques du New Yorker sans le divan du psychologue? Bob Mankoff, lui-même ancien psychologue expérimental, est le responsable des dessins humoristiques du New Yorker. Il affirme que le divan du psychiatre dans les caricatures est un raccourci utile, qui traduit immédiatement une dynamique de pouvoir. Dans Les Soprano, lorsque Tony voit sa thérapeute, il s’assoit dans un fauteuil commun et confortable, mais le divan est là en arrière-plan, au cas où nous oublierions de quel type de bureau il s’agit.
Évidemment, le domaine de la psychanalyse a beaucoup évolué depuis les beaux jours de l’Imperial Leather Furniture Company. Et s’asseoir derrière la tête d’un patient alors qu’il est sur votre divan à vous parler est chose du passé. Toutefois, des images fortes, ancrées dans la culture populaire, peuvent encore exercer une certaine emprise bien longtemps après leur date de péremption. Pendant que l’image cigare-divan-psychologue s’estompe, il en va de même pour l’ostracisme que subissent les personnes qui cherchent de l’aide pour traiter un problème de santé mentale.
Le Dr Nicholas Carleton est professeur de psychologie à l’Université de Regina, psychologue clinicien agréé en Saskatchewan et actuel directeur scientifique de l’Institut canadien de recherche et de traitement en sécurité publique. Il se réjouit des progrès que fait la discipline en démystifiant et en démantelant l’ostracisme qui frappe les gens qui cherchent du soutien psychologique.
« Je crois que nous assistons au déclin de la stigmatisation, et je pense que c’est largement dû au fait que les psychologues sont de plus en plus présents dans la collectivité. L’idée que vous vous retrouverez comme dans un épisode de Mad Men quand vous entrerez dans le bureau d’un psychologue, avec un grand canapé en cuir et quelqu’un qui fume un cigare, tout cela peut sembler très inquiétant – j’imagine que c’est en grande partie disparu de la réalité. Je pense également que cette idée aujourd’hui mythique au sujet de ce qui se produit lors d’une visite chez un thérapeute disparaît peu à peu. »
La Dre Brigitte Sabourin est professeure adjointe à l’Université du Manitoba, au département de psychologie clinique de la santé, et praticienne en psychologie clinique à Winnipeg. Elle est la présidente de la Section de psychologie clinique de la SCP, et dit que le domaine a beaucoup progressé, mais que ses objectifs fondamentaux demeurent les mêmes.
« Nous pouvons nous définir comme un champ d’activité où nous avons affaire au fonctionnement humain. La psychologie clinique va de la détermination des problèmes humains et de leurs solutions, à la promotion globale du bien-être physique, social et mental. Cela implique l’évaluation, le traitement, la consultation, l’élaboration de programmes, la recherche, le mentorat, l’enseignement… »
La Dre Sabourin se spécialise en psychologie clinique de la santé, au carrefour de la psychologie de la santé et de la psychologie clinique. Elle évolue dans une clinique de soins tertiaires auprès de personnes atteintes de douleurs chroniques. Son travail englobe l’examen des aspects biopsychosociaux chez les gens qui vivent avec un problème de santé chronique, et la mise en application des compétences en psychologie clinique et des principes relatifs aux comportements liés à la santé pour tenter de les soutenir. La plupart des psychologues cliniciens ont une spécialisation de ce type, que ce soit en milieu hospitalier ou dans le traitement de troubles de l’humeur particuliers. Ce n’est pas le seul changement qui s’est opéré dans ce champ d’activité depuis les dernières décennies.
Comme le souligne la Dre Sabourin, « je crois que d’une part, le domaine est devenu plus diversifié. Traditionnellement, il était dominé par des hommes blancs, et ça continue de changer. Notre engagement envers la pratique fondée sur des données probantes poursuit son évolution, réunissant l’ensemble de nos connaissances sur ce que nous savons de tout ce qui touche les troubles mentaux jusqu’à l’épanouissement humain. Nous utilisons désormais ce savoir pour améliorer nos services et rendre des comptes aux personnes que nous aidons. Je pense également que les milieux où nous pratiquons ont changé. On trouve des psychologues cliniciens partout, que ce soit dans les soins primaires jusqu’aux soins hyperspécialisés, avec pour résultat que les populations et les milieux auprès desquels nous intervenons sont beaucoup plus diversifiés qu’ils ne l’étaient auparavant. De plus, je crois que la reconnaissance de l’aide que peut apporter l’accès aux services a progressé. Il ne s’agit pas de savoir si quelque chose ne va pas chez vous ou si vous êtes fou : la stigmatisation a commencé à s’atténuer et les gens réalisent que nous pouvons aider n’importe qui, de l’athlète d’élite à la personne qui éprouve de réelles difficultés à accomplir les tâches essentielles du quotidien. »
Le fait de rassembler ces connaissances et de les utiliser en pratique clinique est une question que connaissent bien la Dre Sabourin et le Dr Carleton. Ils sont tous deux chercheurs, en plus d’être cliniciens. Le Dr Carleton reçoit, et traite, plusieurs intervenants de première ligne à Regina – particulièrement à la GRC, puisque l’École est située dans la ville. Il réalise également plusieurs recherches auprès de la GRC et d’autres membres du personnel de la sécurité publique (PSP). Récemment, lui et son équipe ont créé un outil en ligne anonyme où les membres du PSP peuvent évaluer leur propre santé mentale, pour ensuite chercher le soutien dont ils ont besoin.
« Je crois que nous observons une meilleure intégration de la science et de la pratique, poursuit-il. Nous améliorons nos façons de nous connecter les uns aux autres, et nous entretenons des relations fondées sur la pratique réflexive entre les psychologues qui font de la recherche et les psychologues praticiens. Nous constatons combien la science oriente la pratique et vice versa, de manière beaucoup plus dynamique. Par exemple, on a assisté à des changements considérables pour ce qui est du SSPT. Grâce aux interactions étroites entre la pratique clinique et la science, il existe désormais quatre groupes de symptômes plutôt que trois. Les diagnostics de SSPT peuvent dès lors être posés sans qu’il y ait un événement unique, mais en considérant l’ensemble des événements accumulés. Il ne fait aucun doute que, pour nos intervenants de première ligne et les autres membres de la sécurité publique, il s’agissait de deux immenses pas en avant. Les membres du personnel de la sécurité publique avaient de la difficulté à préciser quel incident leur causait le plus de problèmes parce qu’ils en avaient vécu des centaines, voire des milliers, au cours d’une seule année. Auparavant, ils se rendaient chez un psychologue en disant “J’ai des problèmes”, ce à quoi le psychologue aurait pu répondre “J’en ai aussi car je ne peux établir de diagnostic à moins que vous ne choisissiez un seul événement”. Nous avons corrigé ces choses, et nous réalisons des améliorations progressives et d’importantes avancées. »
Une autre évolution avec laquelle nous sommes tous familiers aujourd’hui est de nature technologique. Je mène la présente entrevue avec la Dre Sabourin et le Dr Carleton via Zoom, et il existe des dizaines d’autres plateformes virtuelles disponibles pour tenir des rencontres, et même des séances de thérapie.
La Dre Sabourin précise : « Je crois qu’un autre élément qui a pris de l’ampleur, particulièrement depuis la pandémie, est le rôle de la technologie et de l’innovation sur le plan de l’accès aux services psychologiques. L’idée de devoir se rendre dans un cabinet de psychologue même pour une séance de 15 minutes, quelque part dans un édifice menaçant, ce n’est plus ainsi que nous envisageons la psychologie clinique. Aujourd’hui, nous avons recours aux plateformes de visioconférences, aux applications sur nos téléphones, et ainsi de suite. Par exemple, nous faisons beaucoup de programmes de groupe où les participants peuvent demeurer dans le confort de leur domicile, sans avoir à se rendre en voiture à l’hôpital et payer le stationnement, et tenter de trouver le chemin, et ainsi de suite. Le fait de diminuer les obstacles aux soins et d’augmenter la souplesse dans notre façon de faire représente un progrès enthousiasmant. Ce mouvement existait déjà depuis un moment, mais depuis deux ans, depuis le début de la pandémie, il a pris de l’essor. »
Il y a deux ans, avant le début de la pandémie, la thérapie virtuelle était plutôt marginale. Cependant, bien des choses ont changé depuis. Les psychologues qui étaient réticents à l’idée d’organiser des séances de thérapie sur les plateformes virtuelles ont appris à le faire efficacement, et la prévalence de ce type de technologie a éliminé certains des obstacles aux soins, accru l’aide psychologique disponible et largement contribué à atténuer la stigmatisation persistante entourant la recherche d’aide en santé mentale. Le Dr Carleton souligne que cela a aussi aidé d’autres façons.
« Au risque de dire une hérésie, j’estime vraiment que le fait d’être obligé de travailler à distance, quoique cela ait pu faire obstacle à certains congrès, a réellement rehaussé la collaboration, et ce, sous plusieurs angles. Je peux rencontrer quelqu’un de l’Australie à la fin de ma journée et au début de la sienne : nous pouvons échanger des notes pendant une demi-heure. Nous ne sommes pas préoccupés parce que l’un de nous deux devra bientôt prendre un vol de 16 heures. »
La Dre Sabourin acquiesce. Non seulement les collaborations sont plus faciles, mais il est également plus facile de fournir des soins psychologiques à un plus grand nombre de personnes.
« Nous examinons comment augmenter les ressources et notre portée. Une part de ce travail consiste à adapter le modèle de soins par paliers qui se déploie dans tout le pays. Au premier palier, on offre du soutien à beaucoup de personnes, et puis, quand les besoins augmentent et se complexifient, on offre aux personnes des services psychologiques plus soutenus et intensifs. Nous lisions un article paru dans une revue scientifique à propos de ce modèle à Ottawa, et le directeur de ma clinique disait “J’aimerais que nous puissions prendre un vol vers Ottawa, nous asseoir et discuter avec cette personne! » Et j’ai répondu “Je vais organiser une rencontre Zoom ce mardi”. Ça peut s’organiser si rapidement et nous sommes si habitués à ces plateformes que nous avons l’impression de nous rencontrer en personne lorsque nous échangeons de cette manière. »
Je commande souvent de la nourriture à des fermes locales de ma région, qui me livrent des aliments à domicile. La nourriture est livrée par Miles [nom fictif], un homme très costaud, qui porte une barbe qui lui descend jusqu’à la boucle de ceinture et qui conduit un énorme camion réfrigéré. Il y a peu de temps, nous discutions de mon nouvel emploi à la Société canadienne de psychologie, et Miles m’a parlé d’un de ses collègues dont il s’inquiétait parce qu’il devenait de plus en plus replié sur lui-même. Il s’inquiétait de la santé mentale de son ami. Est-ce que je devrais lui parler? Est-ce que je devrais le laisser seul? En tant que non-psychologue, je ne pouvais lui donner de bons conseils sur ce qu’il fallait faire au juste, mais je pensais que lui offrir gentiment son aide ne pouvait faire de mal. Les autres fois où j’ai vu Miles, il me donnait des nouvelles de son ami. Un jour, l’été dernier, alors que je travaillais dans mon garage, Miles et son collègue étaient tous les deux dans le camion et sont venus s’asseoir quelques minutes. Depuis, à chaque fois qu’ils font une livraison chez moi, nous nous assoyons pendant une quinzaine de minutes et nous parlons un peu de notre propre santé mentale. Comment nous tenons le coup avec la pandémie, quels genres de problèmes nous et nos familles avons affrontés. Le Dr Carleton indique que ce genre de situation se produit de plus en plus.
« Nous avons observé d’extraordinaires améliorations dans le discours entourant la santé mentale. Plutôt que de taire le sujet, les gens en parlent avec franchise. Le fait que nous en soyons à une étape où nous essayons de mobiliser les connaissances sur la santé mentale pour faciliter la transition vers des changements réels – c’est un virage phénoménal même au cours des deux dernières décennies. Nous ne savons peut-être pas exactement où nous irons ensuite, mais au moins, nous ne nions plus que nous pouvons offrir beaucoup d’aide et de formes d’aide aux personnes souffrant de problèmes de santé mentale. Je crois qu’une large part de ce changement est le résultat des activités de représentation des intérêts menées par les psychologues cliniciens et d’autres professionnels de la santé mentale. »
Nous n’avons pas encore terminé : un certain ostracisme demeure et persiste, comme l’image du divan et du cigare. Mais les professionnels de la santé mentale poursuivent leurs efforts pour l’éradiquer, et les psychologues cliniciens n’y font pas exception. La Dre Sabourin résume très bien le message.
« C’est normal d’avoir des problèmes, vous êtes humain. Ce n’est pas facile pour un être humain d’habiter notre planète! Nous essayons tous de vivre nos vies, mais nous n’avons pas choisi nos parents, nous n’avons pas choisi nos gènes, nous n’avons pas choisi le fait que nos cerveaux sont probablement encore programmés pour nous aider à survivre comme il y a 20 000 ans, et notre environnement s’est considérablement transformé depuis. Il s’agit de normaliser le fait que ce n’est pas grave si certains moments de votre vie sont plus difficiles que d’autres. Nous voyons des êtres humains exceptionnels qui se sont épanouis, comme Clara Hughes, l’athlète olympique qui a reconnu avoir des problèmes. Il y a des acteurs renommés et des politiciens qui s’ouvrent sur leurs difficultés et affirment que l’on peut faire quelque chose à ce sujet. En tant que société, nous reconnaissons qu’il n’est pas possible d’être soit en bonne santé, soit malade. Vous pouvez trouver des trucs. Vous pouvez trouver des moyens de vous faciliter la tâche, d’être mieux dans votre peau, d’être plus présent auprès de vos enfants. Nous sommes plusieurs à éprouver des difficultés, et le fait de voir un psychologue ne signifie pas que quelque chose cloche chez vous : simplement, nous sommes tous des êtres humains qui tentent de faire de leur mieux dans un monde difficile. »

Dr. Keira Stockdale

Dr. Sandy Jung
Dre Keira Stockdale and Dre Sandy Jung, Criminal Justice Psychology
La discipline de la justice pénale est vaste et les psychologues sont impliqués dans presque toutes ses facettes, de la prévention jusqu’à la libération conditionnelle. Nous nous sommes entretenus avec la Dre Keira Stockdale et la Dre Sandy Jung à propos de leur travail dans ce domaine, et avons discuté de l’avenir de la profession.
« Je faisais partie des personnes qui regardaient des émissions comme CSI : Les experts quand elles ont commencé à être diffusées à la télé… »
La Dre Sandy Jung lève les yeux au ciel. « Oh non! Non, Keira, ne dis pas ça! Noooooon! »
La Dre Keira Stockdale est psychologue au service de police de Saskatoon et professeure auxiliaire au département de psychologie de l’Université de la Saskatchewan. Elle est l’actuelle présidente de la Section de la justice pénale de la SCP. Elle explique ce qui l’a intéressée à la psychologie, et en particulier, à la psychologie dans le contexte de la justice pénale.
La Dre Sandy Jung est professeure à l’Université MacEwan, à Edmonton. Ses recherches portent sur la psychologie médicolégale, et elle tente de garder son calme quand elle entend les mots qu’elle redoute le plus. Les émissions de télévision qui représentent la science pénale de manière inexacte et trompeuse l’agacent au plus haut point depuis longtemps, semble-t-il!
« Je grimace parce que j’entends cela constamment de mes étudiants. Ils s’intéressent aux sciences criminelles parce qu’ils regardent ces émissions de télé et que c’est attrayant, captivant. Honnêtement, je ne regarde jamais d’émissions policières et je les déteste encore à ce jour! Alors, quand les étudiants me recommandent une émission comme Dexter, je ne peux pas. Je ne la regarderai pas. »
Tout étudiant qui pense entrer dans le monde de CSI à la fin de leurs études est rapidement déçu. Aucun crime ne se résout en une heure par l’analyse de l’ADN ou par l’identification d’eucalyptus sur la semelle d’un soulier. Il est très rare que des enquêtes progressent en enlevant, puis en remettant ses verres fumés, avec pour musique de fond le riff grandiose de Won’t Get Fooled Again. C’est aussi vrai, bien sûr, pour la Dre Stockdale.
« Je suis allée à l’Université de Toronto pour obtenir un diplôme en sciences médicolégales, poursuit-elle. Et pendant que je faisais des comparaisons d’ADN pour vérifier s’il y avait correspondance avec une scène de crime, j’ai réalisé que les cours qui portaient sur les personnes qui commettaient ces crimes étaient beaucoup plus intéressants. Puis, j’ai eu la chance de faire un stage à la PPO, dans son unité d’analyse du comportement. Après cela, j’ai simplement continué à me concentrer de plus en plus sur les gens, ce qui m’a menée vers la psychologie clinique médicolégale! »
Oui, l’unité d’analyse du comportement existe vraiment. Plusieurs d’entre nous connaissent même toutes les abréviations – UAC! Unsub (unknown subject – suspect inconnu)! CODIS (Combined DNA index system)! Merci beaucoup Esprits criminels! Vous ne serez probablement pas étonné de savoir qu’aucune unité d’analyse du comportement réelle ne dispose d’avions privés, de produits dérivés comme des jeux vidéo, pas plus que vous y verrez de grands acteurs comme Jason Alexander.
Comme l’atteste la Dre Stockdale, « lorsque vous entrez dans les locaux, il n’y a pas de photos d’individus sur les murs ou de téléphones qui sonnent sans arrêt, et ainsi de suite; c’est un bureau silencieux où les gens font de l’excellent travail d’enquête. Ils conçoivent aussi des outils d’évaluation du risque et d’autres méthodes que nous pouvons utiliser pour combattre la criminalité, comme la violence familiale ou l’exploitation sexuelle par Internet. »
Alors concrètement, que font les psychologues spécialisés en justice pénale? Est-ce que cela ressemble à ce que fait le personnage de B.D. Wong dans La loi et l’ordre, ou est-ce que cela ressemble davantage au personnage de John Francis Daley dans Bones? « Non ». La Dre Jung indique qu’il y a deux types principaux de psychologues dans le domaine de la justice pénale, mais que la discipline est très vaste et comporte des centaines de spécialisations.
« Le clinicien est probablement le prototype de ce à quoi nous pensons quand nous parlons d’un psychologue en justice pénale, mais ce n’est qu’une partie de la réalité. L’autre partie englobe les volets de la recherche et de la psychologie expérimentale. Non seulement de la recherche dans des contextes concrets, comme les établissements correctionnels ou les centres de traitement, mais également de la recherche sur le croisement entre le système de justice et la psychologie. Toutes les décisions que nous prenons ont une dimension psychologique : il s’agit de décider comment interroger un témoin ou un suspect. Comment collecter les données et comment les interpréter. Et dans le contexte des tribunaux, il y a une multitude de décisions qui sont examinées par les psychologues, comme la détermination de la peine et les décisions concernant la composition des jurys. »
Vous voulez dire influencer les jurys, comme dans Bull? La Dre Stockdale mentionne que la plupart des psychologues qui travaillent dans ce domaine sont en quelque sorte des touche-à-tout qui maîtrisent plus particulièrement un ou deux aspects de leur travail.
« Pour être psychologue dans le domaine médicolégal, de la justice pénale ou auprès des services de police, il faut être un excellent généraliste. Nous apportons beaucoup de nos connaissances générales en psychologie et de notre compréhension clinique à ce champ de pratique. Actuellement, auprès des services de police, je fais partie d’une équipe interdisciplinaire qui tente d’évaluer les risques et d’intervenir auprès des délinquants violents dangereux. L’équipe est composée de procureurs, de policiers, d’agents de probation, de représentants des établissements correctionnels, de travailleurs en santé mentale et de résidents en psychologie. En tant que psychologues, nous avons conçu des outils d’évaluation des risques qu’utilisent nos partenaires du maintien de l’ordre et des libérations conditionnelles. Ainsi, une partie de notre travail consiste à informer cette équipe sur la façon de collaborer pour aider réellement les individus ayant des démêlés avec la justice et des antécédents de violence. Plusieurs d’entre eux ont des besoins en santé mentale, et nous voulons les aiguiller vers les services dont ils ont besoin tout en préservant la sécurité communautaire. Présentement, nous examinons les possibilités de développer plus de services virtuels et nous réalisons d’excellents progrès en ce qui concerne les mégadonnées, les analyses prédictives et la modélisation, en vue d’améliorer les technologies d’évaluation du risque. Comment évaluer les besoins de nos clients, comment déterminer s’ils présentent un risque de récidive, et pourquoi. Nous appliquons également cette même technologie aux cas de personnes disparues. »
L’un des cas de disparition les plus connus de la dernière décennie au Canada s’est produit dans le Village, à Toronto. Entre 2010 et 2017, huit hommes de la communauté gaie sont disparus. On a éventuellement déterminé qu’ils avaient été assassinés par un tueur en série, qui fut arrêté en 2018. La façon dont les services de police de Toronto ont effectué l’enquête préliminaire sur ces personnes disparues a fait l’objet de sévères critiques, menant à plusieurs enquêtes et examens. L’examen externe indépendant a été mené par la juge Gloria Epstein. On a conclu que les services de police avaient échoué et que la communauté gaie de Toronto en avait souffert. Mais la Dre Stockdale a bon espoir qu’un changement significatif en résultera.
« Je suis optimiste et je pense que nous verrons de plus en plus, dans l’avenir, de partenariats universitaires avec tous les domaines de la justice pénale. Nous avons fait un travail sur les personnes disparues, à la suite des disparitions signalées dans le Village à Toronto. Dans son rapport, la juge Epstein recommande que les services de police (dans ce cas, ceux de Toronto) travaillent avec des établissements universitaires et des chercheurs, car, ainsi, ils disposent de personnes qui peuvent les aider à évaluer leurs programmes et leurs initiatives. Les gens ne peuvent y arriver seuls; c’est une question de ressources, mais c’est aussi une question de réflexion et d’attitudes cognitives. Plus nous travaillerons en équipes interdisciplinaires dans le domaine de la justice pénale, plus nous éviterons les préjugés, et nous pourrons peut-être vérifier certaines de nos hypothèses ou interventions. Et nous pourrons les adapter à l’avenir. »
La psychologie dans le domaine de la justice pénale évolue constamment, est en perpétuel changement et s’améliore sans cesse (quoique lentement). Selon la Dre Jung, la clé de voûte est la mobilisation des connaissances, à savoir le processus par lequel la recherche génère des données et des réponses, puis traduit ce travail en changements concrets et en meilleures pratiques.
« Nous avons besoin de beaucoup plus de mobilisation des connaissances pour progresser. Une tonne de recherche doit encore être réalisée, mais nous devons faire mieux pour mettre en œuvre les choses que nous savons déjà. Nous pouvons aider à répondre à certaines questions pratiques très pointues. Nous savons que les groupes à risque élevé devraient bénéficier de plus de supervision, mais où se situe la limite? Combien d’heures devrions-nous investir dans l’administration de traitements? Nous disséminons cette information, mais nous ne l’utilisons pas concrètement comme nous le pourrions. En fait, il faut environ 17 ans avant que toute donnée probante ne soit mise en œuvre. Je me souviens, lorsque j’ai entendu cette citation, m’être dit : “c’est déprimant”! »
Dix-sept ans, c’est en effet une statistique déprimante, et le changement peut certes sembler lent. Mais la Dre Stockdale affirme pourtant qu’elle voit ce changement dans plusieurs facettes de la justice pénale, y compris dans le travail qu’elle a elle-même accompli.
« Je regarde certains des rapports d’évaluation psychologique que j’ai rédigés il y a longtemps pour des individus ayant des démêlés avec la justice, et je réalise à quel point la pratique a changé. Au Canada, nous sommes reconnus sur la scène internationale pour notre conception d’outils et de technologies d’évaluation des risques. Il y a des années, l’évaluation était une question de jugement : est-ce que cette personne récidivera? Peut-être? Aujourd’hui, cette décision est beaucoup plus structurée et fondée sur des données probantes. Maintenant, nous examinons toute une série de facteurs et déterminons où nous pouvons intervenir ou offrir du soutien afin de diminuer le risque qu’une personne soit violente, commette des agressions sexuelles ou verse dans la criminalité en général. Nos programmes de traitement sont beaucoup plus pointus qu’ils ne l’étaient il y a des décennies, car nous nous concentrons sur ces dynamiques ou facteurs changeants.
Nous nous éloignons des étiquettes négatives et stigmatisantes, pour tendre vers un langage plus positif. Par exemple “individus ayant des démêlés avec la justice” plutôt que “délinquants” ou “détenus”. Nous nous éloignons également d’une vision centrée sur le négatif dans le traitement des personnes, et je crois que c’est particulièrement important pour les jeunes dans le système de justice pénale, où nous mettons l’accent sur les aspects positifs, comme la force et la résilience. »
L’un des autres aspects où l’on observe des changements en justice pénale concerne la justice sociale. Ici encore, c’est un processus très lent, le système judiciaire étant constitué de composantes si énormes qu’il devient un énorme navire à diriger. La Dre Jung dit que, longtemps, le travail des chercheurs était cloisonné, mais que cette situation évolue maintenant, les médias sociaux et les données numériques rendant la collaboration et le travail interdisciplinaire plus faciles et plus accessibles. Elle mentionne aussi qu’il reste un très très long chemin à parcourir avant que le système judiciaire canadien et ceux du monde entier n’atteignent l’équité à laquelle ils aspirent tous.
« Il y a quelques affaires judiciaires qui ont vraiment attiré l’attention sur quelque chose dont tout le monde connaissait déjà l’existence, mais que nous n’avions pas examiné autant que nous l’aurions dû. Il nous faut ce genre d’affaires pour nous rappeler qu’il s’agit d’une question d’une extrême importance. En matière d’équité, de diversité et d’inclusion, certains sous-groupes ont été étudiés, mais pas tous : nous avons investi bien peu d’efforts en ce qui concerne le genre, notamment. Je dirais que nous ne faisons qu’effleurer la surface du problème. »
La Dre Stockdale souligne que lorsqu’elle pense aux questions entourant les mouvements comme Moi aussi, Black Lives Matter et l’oppression des Autochtones, elle réfléchit au peu de formation qu’elle a reçue sur ces problématiques lorsqu’elle faisait ses études de doctorat en psychologie. En plus d’éduquer les équipes, on doit continuer à discuter de ces enjeux plus largement. Nous entrons dans une ère de prisons intelligentes et d’applis d’évaluations du risque. Ainsi, elle estime que nous pouvons peut-être utiliser la technologie de façon positive pour nous orienter sur cette route. Elle milite également en faveur d’un virage général de plus grande ampleur en matière de philosophie.
« Je pense qu’il faut favoriser la participation des groupes et des organisations communautaires, des groupes d’intérêts particuliers qui travaillent auprès de certaines de ces populations et de ces personnes. En tant que psychologues en justice pénale, nous aimons appliquer les connaissances scientifiques, mais nous reconnaissons aussi que ce n’est qu’un moyen de savoir. Et dans le système juridique, nous devons être ouverts et respectueux à l’égard des autres modes de savoir. Ce sera le défi de l’avenir et je crois que nous devons vraiment nous concentrer sur cet aspect. »
Même les séries policières qui suscitent l’intérêt envers la justice pénale commencent à s’orienter vers des thèmes liés à la justice sociale – du moins, elles s’y essaient. C’est souvent embarrassant, et parfois maladroit, mais la plupart de ces émissions sont déjà embarrassantes et maladroites. Nous savons maintenant que ce ne sont pas les émissions criminelles télévisées qui ont conduit la Dre Jung vers la psychologie. Alors qu’est-ce qui l’a motivée?
« J’avais choisi au départ la psychiatrie. J’ai suivi un cours pendant ma troisième année d’études de premier cycle à l’Université de la Colombie-Britannique avec John Yuille et Robert Hare. Le Dr Hare est le concepteur de la Hare’s Psychopathy Checklist, l’échelle d’évaluation de la psychopathie de Hare, et j’ai trouvé ça tellement intéressant et attirant que tout à coup, je me suis intéressée à un tout autre domaine. À partir de ce moment, j’ai commencé à faire du bénévolat dans des laboratoires et à m’intéresser à la fois aux témoignages des témoins oculaires et à la psychopathie. Je savais à cette époque que j’étais là pour de bon. Ce fut toute une aventure. Je n’aurais jamais cru passer des services de santé mentale médicolégaux à aujourd’hui, où je travaille avec des enquêteurs de police sur leur façon de gérer les délinquants dans la collectivité. »
Très bien, voici une autre référence à la culture pop. Le Dr Robert Hare a participé au documentaire canadien primé et réalisé en 2003, The Corporation, dans lequel il semblait conclure que si une entreprise était une personne, elle cocherait presque toutes les cases de l’échelle d’évaluation de la psychopathie de Hare. Toutefois, dans la parution ultérieure de son ouvrage Snakes in Suits : When Psychopaths Go to Work, Hare indique que ses commentaires ont été pris hors contexte par le réalisateur, et que dans les faits, une entreprise ne répondrait pas vraiment aux critères permettant de la désigner comme « psychopathe ».
Alors que le vaste thème de la justice pénale grandit et prend de la maturité, et qu’il en va de même pour la psychologie qui l’accompagne, la Dre Jung et la Dre Stockdale souhaitent toutes deux nous dire que les choses s’améliorent vraiment. Que même si quelque chose semble mauvais aujourd’hui, le fait de se souvenir de ce que cela aurait pu être il y a vingt ou trente ans montre que nous faisons des progrès.
Comme l’affirme la Dre Stockdale, « Nous sommes plus en sécurité que nous ne l’étions, à simplement marcher dans la rue. Dans les années 1980, on menait toutes sortes de campagnes visant à inciter les gens à se méfier des étrangers, des inconnus, etc. On imaginait être plus en danger face à un inconnu qui se cache quelque part, au coin de la rue. Évidemment, aujourd’hui, nous savons que nous sommes plus en danger face aux personnes que nous connaissons, et désormais, nous sommes tous conscients de cela. On peut ne pas aimer les balados de documentaires criminels ou grimacer devant des émissions de télévision du genre Les experts, mais je crois qu’on peut y voir une sorte de fonction de protection, car certaines des données probantes que nous avons apprises en justice pénale, dont il est question sur ces plateformes, ont en réalité amélioré notre sécurité. »
La Dre Jung grimace.

Dre Zarina Giannone
Dre Zarina Giannone, Psychologie du sport et de l’exercice
Tandis que les exploits des athlètes olympiques captent notre attention, nous mettons aujourd’hui l’accent, dans le cadre du Mois de la psychologie, sur les psychologues qui les aident à atteindre ces performances exceptionnelles. Toutefois, la psychologie du sport ne s’intéresse pas qu’aux athlètes de haut niveau. Nous avons parlé de ce domaine passionnant avec la Dre Zarina Giannone.
Psychologie du sport et de l’exercice
Brooke d’Hondt n’a que seize ans, et elle a déjà une équipe d’entraîneurs et d’experts qui l’aident à exceller en snowboard demi-lune. Brooke a terminé à la dixième place à l’épreuve de demi-lune en planche à neige pour le Canada aux Jeux olympiques de Beijing, et lorsque les Jeux seront terminés, elle retournera à l’école. Imaginez être dans son cours de gymnastique!
La psychologie du sport a en quelque sorte émergé des cours de gymnastique; l’éducation physique est née dans le monde de l’éducation et a évolué au fil du temps vers la psychologie du sport que nous connaissons aujourd’hui. Habituellement, les programmes d’études supérieures en psychologie du sport sont dispensés dans les écoles de kinésiologie des universités. Ils offrent des diplômes qui produisent des scientifiques spécialistes de la psychologie du sport.
Aujourd’hui, deux voies principales s’offrent aux personnes qui souhaitent exercer la psychologie du sport et deux types de titres de compétences existent en Amérique du Nord. L’un d’eux est le psychologue agréé, dont le champ d’activité est le plus vaste lorsqu’il a acquis la formation et l’expérience nécessaires pour se dire spécialisé en psychologie du sport et de l’exercice ou en psychologie de la performance. L’autre est un professionnel appelé « conseiller en performance mentale » (CPM). Les personnes qui détiennent ce titre sont titulaires de diplômes scientifiques et ont suivi une formation appliquée, mais leur champ d’activité est limité à l’application des connaissances psychologiques dans le contexte de la performance ou du sport.
La Dre Zarina Giannone a emprunté ces deux voies. Psychologue agréée spécialisée en psychologie du sport et de la performance, la Dre Giannone a fait sa formation de deuxième cycle en psychologie du counseling, mais a suivi une formation appliquée en psychologie du sport (le CPM).
« La psychologie du sport est l’un des domaines de la science du sport au sens large, explique-t-elle. Même mon propre travail en tant que psychologue du sport n’est qu’une petite part d’un plus grand gâteau, dans la mesure où il couvre l’application de la psychologie de la performance. Il consiste à prendre des données scientifiques et théoriques et à les appliquer à des situations réelles. »
La question de la santé mentale des athlètes n’a jamais été autant sous les projecteurs qu’aujourd’hui. Des athlètes de haut niveau parlent de leur santé mentale, se retirent de leur sport pour prendre soin de leur santé mentale et rendent publiques leurs difficultés. Naomi Osaka, Simone Biles, Calvin Ridley, Clara Hughes, Andy Robertson. La liste des athlètes qui ont commencé à parler publiquement de la santé mentale s’allonge de jour en jour. C’est une tendance qui enthousiasme la Dre Giannone.
« Même pendant mes sept années d’études supérieures, j’ai remarqué certains changements très intéressants. Au début des années 2000, le domaine se concentrait davantage sur les aptitudes mentales traditionnelles enseignées aux équipes, aux athlètes et aux entraîneurs. Imagerie mentale, régulation de l’éveil, contrôle de l’attention, ce genre de choses. Ce sont des compétences importantes qui, si elles sont bien maîtrisées par les athlètes, peuvent améliorer leurs performances. Il s’agit également de compétences transférables qui peuvent améliorer le bien-être général et le fonctionnement quotidien. Ces derniers temps, les psychologues et les CPM personnels sont de plus en plus recherchés. Cela s’explique, entre autres, par le fait que les athlètes se sentent plus à l’aise pour divulguer leurs problèmes de santé mentale. La stigmatisation associée à ces problèmes a diminué. Cela signifie que le rôle des psychologues dans les clubs et les organismes sportifs est plus prisé qu’avant. »
Les Colts d’Indianapolis, par exemple, ont lancé une initiative appelée Kicking The Stigma et le porte-parole de la campagne est le défenseur vedette Darius Leonard, qui parle ouvertement de ses crises d’angoisse et de sa dépression. Mais pour chaque équipe qui s’attaque aux problèmes de santé mentale et tente de lutter contre la stigmatisation qui leur est associée, il semble y avoir un autre groupe qui tarde à faire de même. La Ligue canadienne de hockey a récemment publié un rapport dévastateur sur l’existence d’un « code du silence » qui a permis à l’inconduite à l’extérieur de la patinoire de devenir une « norme culturelle ».
« Je connais certaines organisations et certaines équipes qui prennent la santé mentale très au sérieux, et il y a des psychologues du sport qui sont impliqués dans la résolution de problèmes dans une perspective de justice sociale, poursuit la Dre Giannone. Par exemple, ceux qui travaillent avec des cas d’abus ou d’inconduite sexuels. Ces psychologues ont contribué à la création de changements systémiques dans certaines organisations. On observe de plus en plus de politiques de santé mentale, ou de politiques de diversité et d’inclusion être mises en œuvre dans les organisations. J’espère que les gens en ressentiront les effets, et que ce ne sera qu’une question de temps avant que toutes les grandes organisations sportives emboîtent le pas. »
Pour la première fois depuis longtemps, les joueurs de la LNH ne sont pas présents aux Jeux olympiques. Cela signifie que les équipes de hockey qui s’affrontent se répartissent en deux catégories : soit un groupe de joueurs qui jouent ensemble dans un contexte ou un autre depuis longtemps, soit une équipe composée des meilleurs joueurs disponibles qui ont peu d’expérience de jeu entre eux. Comment créer une dynamique de groupe et développer la confiance de l’équipe? Selon la Dre Giannone, ces questions sont de plus en plus du ressort des psychologues du sport et des CPM.
« Les psychologues du sport ne se contentent plus d’offrir des formations classiques sur les aptitudes mentales et de simples évaluations des compétences mentales. Aujourd’hui, mon travail se concentre sur l’optimisation des performances, mais il concerne également d’autres difficultés propres au sport, notamment la dynamique de groupe entre les membres de l’équipe, le leadership des entraîneurs et la gestion de divers problèmes de santé mentale rencontrés par les athlètes, comme l’épuisement professionnel, la dépression, l’anxiété ou les troubles de l’alimentation. À bien des égards, le rôle du psychologue du sport a été réinventé et consiste désormais à répondre à la fois aux besoins psychologiques et aux exigences de la performance inhérentes au sport. »
La Dre Giannone travaille principalement en pratique privée au Vancouver Psychology Centre, où elle reçoit des clients en psychologie générale et d’autres personnes qu’elle aide en sa qualité de psychologue spécialisée en psychologie du sport et de la performance. Dans cet espace, elle voit un large éventail d’athlètes et d’artistes – des jeunes jusqu’aux professionnels. À l’occasion, elle accepte un contrat avec une équipe, pour laquelle elle met en œuvre un programme de développement des aptitudes mentales ou fournit d’autres services de groupe. Elle travaille également avec le Canadian Centre for Mental Health in Sport (CCMHS), où elle offre des services de santé mentale aux athlètes et aux artistes.
« Depuis 2013, le financement fédéral de ces services a vraiment augmenté, et ce, assez rapidement. Il existe aujourd’hui quelques services financés par le gouvernement fédéral destinés aux sportifs de niveau national. Par exemple, il y a le programme Plan de match, qui offre une vaste gamme de services aux athlètes brevetés de haut niveau au Canada. Mon rôle au CCMHS s’adresse à tous les sportifs, entraîneurs et administrateurs, quel que soit leur niveau, et permet à certaines personnes d’accéder à du financement à cet effet. Les autres pays sont un peu en retard dans ce domaine, ce qui fait du Canada un chef de file dans la sphère de la santé mentale des sportifs. »
Comme c’est le cas de tous les événements majeurs des deux dernières années, la COVID est une question centrale des Jeux olympiques de 2022. Elle a perturbé l’entraînement, entravé la consolidation des équipes et fait perdre à de nombreux athlètes la chance de concourir sur la scène mondiale. La COVID a même coûté à certains athlètes la chance de concourir après leur arrivée aux Jeux, lorsqu’un test positif a mis fin prématurément à leur parcours olympique. La Dre Giannone a vu tous les hauts et les bas créés par la pandémie chez les athlètes de tous les niveaux.
« Au début, les sports étaient sur pause. Les tournois importants ont été reportés. À ce moment-là, il fallait vraiment modifier et faire évoluer les services psychologiques vers un mode de prestation en ligne. Nous avons fait des choses en équipe avec plus de 25 personnes sur Zoom! Au cours de la dernière année, de nombreux athlètes ont repris le sport, et il se présente des défis nouveaux auxquels nous n’avons jamais été confrontés auparavant. Le contenu du travail a changé – imaginez un jeune athlète qui n’a participé à aucune compétition au secondaire depuis deux ans. Il était en secondaire 2, et il est maintenant en secondaire 4. Ce que cela représente pour ces jeunes sur le plan du développement et du perfectionnement des compétences propres au sport est intéressant.
Mes recherches portent principalement sur le développement de l’identité dans le sport. Ce qui arrive lorsqu’une personne se blesse ou prend sa retraite, et la perte d’identité qui en découle. La COVID est à l’origine d’un grand nombre de menaces pour l’identité, qu’il s’agisse d’enfants ou d’athlètes olympiques. Ces personnes qui tirent du sport une telle estime de soi et une telle valeur sont involontairement contraintes de le mettre de côté pendant un certain temps. Cela peut être très déstabilisant pour les gens.
Je dirais, à l’inverse, que la COVID a offert aux athlètes une occasion inédite de pratiquer leur sport d’une manière nouvelle et différente. Prenons l’exemple d’un sportif qui n’avait jamais le temps de regarder des vidéos de lui-même. Désormais, il est capable d’apprendre des choses différentes sur lui-même. Il est peut-être capable de faire un peu plus de musculation. J’ai été frappée par la résilience et la créativité dont ont fait preuve les gens durant cette période.
Ce qui m’a vraiment frappée au début de la pandémie, c’est le passage de l’entraînement aux compétences physiques et mentales à la création de nouvelles conceptions de la culture d’équipe. Je me souviens d’être intervenue dans des équipes et d’avoir aidé à faciliter la réalisation des objectifs, et à cultiver les valeurs de l’équipe et les relations entre ses membres. Cela ne veut pas dire que je ne le ferais pas pendant une saison régulière, mais la pandémie a vraiment mis cela en évidence car il n’y avait pas grand-chose d’autre à faire quand la situation était si incertaine. »
La santé mentale des athlètes est un domaine en expansion rapide. Le rôle des psychologues dans la résolution de certains problèmes sociaux et systémiques tels que les comportements inappropriés des athlètes, la violence dans le sport, les abus et le harcèlement, l’inclusion et la diversité culturelle, devient de plus en plus important. Les psychologues participent à la création de mesures de soutien, mais aussi à la promotion de changements systémiques au sein des systèmes et des organisations, et tout cela se répercute sur les athlètes. Mais leur influence et leur implication ne se limitent plus aux vestiaires.
Comme l’évoque la Dre Giannone, « les professionnels de la psychologie du sport sont désormais sortis du cadre traditionnel du sport et de l’exercice. Ils s’occupent des problèmes liés à la performance dans d’autres domaines. Il n’est pas rare de voir des psychologues du sport travailler avec des militaires, des artistes de la scène, des premiers intervenants ou des dirigeants d’entreprise de haut niveau. Presque tout le monde se retrouvant dans des situations très stressantes. Je m’attends à voir davantage de psychologues possédant ces compétences spécialisées se frayer un chemin dans divers milieux. »
Les Jeux olympiques, qui se déroulent en ce moment même, présentent une gamme de situations stressantes pour les athlètes, sous le regard du public, tous les jours, toute la journée. Nous pouvons nous réjouir de la performance improbable de l’équipe canadienne en poursuite par équipes de patinage de vitesse, mais aussi compatir à la douleur de l’équipe japonaise, dont la chute de l’une de ses membres a donné la médaille d’or au Canada. Nos yeux, les yeux du monde, ajoutent une pression inédite pour ces sportifs. Cette situation peut être difficile, et un psychologue peut aider l’athlète à y faire face. Que vous soyez Jennifer Jones, qui participe à ses deuxièmes Jeux olympiques à l’âge de 47 ans ou une planchiste de 16 ans, qui s’apprête à retourner à ses cours de géographie.
 Dr Kofi-Len Belfon
Dr Kofi-Len BelfonFévrier, c’est le Mois de l’histoire des Noirs, et la SCP met en vedette, tout au long du mois, des psychologues noirs contemporains. Le Dr Kofi-Len Belfon est un psychologue clinicien et travaille avec les enfants, les adolescents et les familles. Il porte de nombreux chapeaux, comme celui de directeur clinique adjoint de Kinark Child and Family Services.
« Pensons-nous réellement à concevoir les programmes d’une manière anti-oppressive? Est-ce que nous envisageons le contenu? »
Le Dr Kofi Belfon est un psychologue clinicien et travaille avec les enfants, les adolescents et les familles. Il est le directeur clinique adjoint de Kinark Child and Family Services, a un cabinet privé appelé Belfon Psychological Services, est membre du conseil d’administration d’Esprits Sains Enfants Sains (anciennement la Fondation de psychologie du Canada) et siège au comité sur l’équité, la diversité et l’inclusion (EDI) de l’Ordre des psychologues de l’Ontario. Orateur pondéré, il réfléchit attentivement avant de répondre aux questions que je lui pose. Le thème de la « réflexion » revient assez souvent pendant notre conversation.
Né à Sainte-Lucie, le Dr Belfon a immigré au Canada lorsqu’il avait à peu près cinq ans. Sa famille a déménagé dans les Caraïbes lorsqu’il avait environ 15 ans, et il est resté chez des amis de la famille pour terminer ses études secondaires au Canada. Ses parents accordaient beaucoup d’importance à l’instruction et l’ont encouragé à aller à l’université. Son frère est médecin et il a d’abord étudié à l’Université McMaster pour faire ses études de premier cycle en vue de suivre les traces de son frère et de devenir médecin. Mais très vite, il découvre que non seulement il réussit très bien dans ses cours de psychologie, mais qu’il les aime vraiment. Une nouvelle voie professionnelle s’ouvrait.
Après son baccalauréat, le Dr Belfon a travaillé dans une usine de peinture. Pendant ce temps, il a passé son test GRE (Graduate Records Examination – un test général normalisé visant à mesurer les capacités scolaires des diplômés) et il a fait des demandes d’admission auprès de programmes d’études supérieures en psychologie. Ce qu’il n’a pas fait, et qui a peut-être joué un rôle déterminant, c’est passer le test GRE évaluant les aptitudes en psychologie. Toutes les écoles d’études supérieures ont refusé sa demande, sauf une.
« Le seul endroit où j’ai été accepté est l’Université de Guelph. Le Dr Michael Grand a été un superviseur vraiment formidable qui m’a soutenu et encouragé. Mais j’ai toujours eu le syndrome de l’imposteur, doutant constamment de moi. “Je n’ai été accepté nulle part ailleurs, pourquoi ai-je été accepté ici, est-ce qu’ils essaient tout simplement de remplir un quota? Est-ce que j’ai été admis parce que je suis un Noir et un homme, et qu’ils veulent accroître la diversité au sein de leur programme?” Je manquais de confiance et mes doutes sur moi-même ont perduré longtemps. Nous n’étions qu’une petite cohorte, de cinq ou six personnes à peine, et j’étais le seul à ne pas avoir de bourse. J’ai fait des demandes de bourse chaque année et aucune n’a été acceptée, ce qui a alimenté le syndrome de l’imposteur et le sentiment que je n’étais pas à ma place.
Le bon côté des choses c’est, entre autres choses, que cela m’a obligé à travailler parce que je n’avais pas beaucoup d’argent! J’ai travaillé énormément sur le terrain. J’ai travaillé au conseil scolaire du district de Toronto pendant toutes mes études de doctorat et j’ai beaucoup d’expérience dans le domaine de l’éducation. J’ai travaillé dans un cabinet privé, j’ai travaillé au Syl Apps Youth Centre et j’ai acquis beaucoup d’expérience clinique intéressante. J’étais toujours très satisfait de mon travail de recherche. L’une des choses que j’aimais chez le Dr Grand, c’est qu’il ne m’empêchait pas de faire ce que je voulais.
Mes recherches portaient sur la violence communautaire chronique dans la région de Scarborough, puis, dans le cadre de mon doctorat, je me suis intéressé aux besoins en santé mentale des enfants en placement et en détention. À cette époque, au moins 50 % des enfants avec lesquels je travaillais étaient des PANDC. Une partie de ces recherches s’explique par le fait qu’à l’université, j’avais un ami proche qui est mort des suites de la violence armée. C’est ce qui m’a poussé à entamer ces recherches, et aujourd’hui encore, j’aimerais avoir plus de temps pour faire de la recherche et d’autres choses de ce genre, parce que cela signifie énormément pour moi. »
Avec tous les postes qu’occupe le Dr Belfon et les multiples chapeaux qu’il porte, il lui reste très peu de temps pour la recherche – ou pour quoi que ce soit d’autre d’ailleurs. Surtout aujourd’hui, car, d’après lui, la pandémie a considérablement augmenté la charge de travail. Les listes d’attente ne cessent de s’allonger et de plus en plus d’enfants, de jeunes et de familles demandent de l’aide pour des problèmes de santé mentale. Selon lui, cette augmentation de la demande est bien antérieure à la pandémie. Il dit avoir constaté, au cours des cinq dernières années, une augmentation du nombre de jeunes demandant de l’aide pour des problèmes de dépression, d’anxiété et de santé mentale. Il est difficile de dire si cela est dû au fait que les jeunes sont plus nombreux à souffrir ou au fait que les efforts déployés pour déstigmatiser ces maladies les incitent à demander de l’aide.
Les personnes qui s’adressent au Dr Belfon sont souvent des familles noires qui veulent voir un psychologue qui leur ressemble et qui a un vécu semblable au leur. Souvent, elles sont prêtes à attendre très longtemps, plus de huit mois parfois, pour consulter un psychologue noir. Pour lui, ce n’est pas l’idéal – c’est très long lorsque vous avez des problèmes graves, et il n’y a aucune garantie que vous rencontrerez un professionnel. Comme le dit le Dr Belfon, « nous confondons sans cesse race et culture ».
La rareté des psychologues noirs demeure une difficulté dans les communautés de couleur et se ressent fortement dans le sud de l’Ontario. À un moment donné, Belfon Psychological Services employait 60 % des psychologues noirs de la région – ils étaient trois. Voilà une autre raison pour laquelle la question de l’équité, de la diversité et de l’inclusion est si importante dans le domaine de la psychologie.
Le Dr Belfon apporte la dimension de l’EDI à tous ses projets, en s’efforçant de rendre les programmes plus inclusifs à Esprits Sains Enfants Sains, à l’organisme Kinark et dans son cabinet privé. Selon lui, il est bon de faire des efforts pour utiliser un langage plus inclusif, et de choisir des images et des exemples qui mettent en scène un groupe de personnes plus diversifié. Tout cela est utile pour faciliter l’accès et inciter davantage de personnes à demander des services et de l’aide. Mais ces mesures restent « superficielles ». Une fois que les gens ont franchi la porte, la programmation elle-même répond-elle à leurs besoins? Le programme auquel ils accèdent est-il aussi inclusif que le message qui les a amenés ici en premier lieu?
« Je ne connais pas nécessairement les réponses à ces questions. La psychologie commence à peine à penser de cette manière. Mais nous devons évaluer ces choses tout en pensant à la diversité et à la façon dont les différentes familles peuvent envisager ces choses différemment. Par exemple, un programme de formation parentale où nous parlons des pratiques parentales et de ce que nous considérons, en Amérique du Nord, comme des pratiques saines. Cela peut être totalement différent pour une famille dont les parents n’ont pas grandi dans la société nord-américaine et qui n’ont peut-être pas les mêmes valeurs. »
C’est à ce moment que le Dr Belfon revient au thème de la « réflexion » – ce qui compte le plus dans les efforts d’équité, de diversité et d’inclusion, c’est qu’ils soient au premier plan lorsqu’un programme est conçu, un comité est créé ou une politique est mise en œuvre. Si nous commençons tous à regarder ces questions sous l’angle de l’EDI et que nous partons de là, il est plus probable que le résultat final soit réellement inclusif et ne soit pas une simple façade.
« Nous réfléchissons systématiquement dans les organismes, à toutes les choses qui sont tournées vers l’intérieur. Les structures de direction, les pratiques d’embauche, les politiques et les procédures, en réfléchissant à la façon dont nous nous traitons les uns les autres. Peut-être avons-nous changé certaines formulations et expressions et amélioré des choses élémentaires, comme éliminer le langage binaire lié au genre sur nos formulaires. Une fois que nous aurons établi un cadre pour ce genre de choses – et nous avons entamé une partie de ce travail à Kinark –, la prochaine étape consistera à aborder la pratique clinique réelle, et à y réfléchir plus attentivement. Cela prendra du temps, et peut-être que rien ne changera! Peut-être que nous examinons un programme et décidons que le contenu est conforme à ce qu’il doit être. Mais y avons-nous réfléchi? Nous sommes-nous demandé si le contenu était pertinent ou non, au lieu de supposer que tous ces concepts sont neutres sur le plan culturel? Selon moi, c’est très important. »
Le comité de l’EDI du Collège des psychologues de l’Ontario ne travaille pas en vase clos. Il s’agit plutôt d’un groupe de personnes dont le rôle est d’influencer tous les autres groupes qui peuvent bénéficier de leur contribution. La Dre Donna Ferguson est la présidente du comité et le Dr Belfon travaille avec elle et les autres pour intégrer l’EDI à la culture globale du Collège.
« Nous avons étudié les expériences de nos membres par rapport à l’EDI et au Collège, en commençant par distribuer des questionnaires aux membres et recueillir des données auprès d’eux. Nous avons fait quelques formations sur l’EDI avec les autres comités, comme le comité de discipline, le comité de l’assurance de la qualité, mon propre comité, qui est celui des relations avec la clientèle. Nous disposons donc d’un langage avec lequel nous pouvons envisager l’EDI dès le départ. Ce que nous avons demandé, c’est qu’après cette formation, les membres de ces comités soient invités à réfléchir à la manière dont la thématique de l’EDI pourrait être liée à leur travail. »
Le Dr Belfon, la Dre Ferguson et le reste du comité de l’EDI se rendent dans chacun des autres comités, un à un, pour discuter du lien entre l’équité, la diversité et l’inclusion, et leur travail.
« Par exemple, si le comité d’inscription est responsable des examens oraux, y a-t-il des éléments des examens oraux auxquels nous devrions réfléchir et que nous devrions repenser à la lumière de l’anti-oppression ou de l’inclusion? »
Réfléchir. C’est le thème central de tout ce que fait le Dr Belfon, et c’est la clé pour faire évoluer les organisations, les entreprises, les groupes, et même la psychologie elle-même, dans une direction plus inclusive. C’est bien d’agir, mais avant d’avoir agi, avez-vous réfléchi? Avez-vous envisagé les choses sous l’angle de l’inclusion? Et comment vous assurez-vous que vos programmes sont inclusifs, plutôt que de simplement en avoir l’air?
Cela mérite réflexion.

Dr Amir Sepehry

Dre Diana Velikonja
Dr Amir Sepehry and Dre Diana Velikonja, Psychopharmacologie
Au carrefour de la psychologie et de la médecine se situent la psychopharmacologie. Les psychopharmacologues sont des psychologues qui peuvent prescrire des médicaments comme le font les psychiatres, mais qui possèdent une formation de psychologue sur les interventions basées sur le comportement et la thérapie. Le Dr Amir Sepehry et la Dre Diana Velikonja nous en parlent davantage.
Au Canada, il faut habituellement environ 10 ans pour devenir psychologue. Il s’agit de l’un des domaines d’études les plus longs et les plus intensifs puisqu’on exige généralement un doctorat en psychologie professionnelle ou un doctorat en psychologie clinique. Or, ces programmes sont assez limités, et il faut plus de temps pour terminer un programme de doctorat en psychologie que la plupart des autres programmes. Imaginez franchir toutes ces étapes, puis décider que finalement, vous voulez poursuivre vos études plus longtemps. D’où vient votre extrême passion, qui vous donnera envie de POURSUIVRE vos études lorsque vous avez enfin terminé?
Pourtant, c’est la décision qu’ont prise les gens qui ont emprunté la voie de la psychopharmacologie. La Dre Diana Velikonja a une formation en neuropsychologie. Elle est psychologue clinicienne et détient une maîtrise en psychopharmacologie clinique qui lui permet d’offrir des consultations impliquant des médicaments psychotropes. Elle a travaillé auprès de personnes ayant subi des traumatismes crâniens, a été présidente de l’Ontario Psychological Association, et elle a mené des initiatives militant en faveur de l’élargissement de la portée de la pratique des psychologues ontariens pour y inclure la prescription de médicaments psychotropes. Elle décrit la psychopharmacologie de la manière suivante :
« Pour traiter plusieurs problèmes émotionnels et cognitifs, on utilise certains types de médicaments qui sont appelés « médicaments psychotropes ». Ils sont principalement utilisés pour traiter des troubles tels que l’anxiété, la dépression, les hallucinations. Par ailleurs, ils aident à gérer les symptômes des troubles de santé mentale ou de dépendance. La psychopharmacologie consiste en fait à prescrire des médicaments, parallèlement à d’autres traitements fondés sur des données probantes. La raison pour laquelle les psychologues sont impliqués dans ce domaine est qu’ils sont formés aux interventions basées sur le comportement et la thérapie, et ceux d’entre eux qui ont demandé une certification supplémentaire en matière de prescription de médicaments psychotropes sont capables d’intégrer les deux – le comportement et les médicaments – afin d’orienter les patients vers les meilleures stratégies pour gérer les symptômes qu’ils éprouvent. »
La prescription de médicaments pour traiter la maladie mentale est depuis longtemps, du moins au Canada, l’apanage de la psychiatrie. Les psychopharmacologues représentent les quelques rares psychologues qui possèdent le savoir requis quand il s’agit de ces médicaments. Le Dr Amir Ali Sepehry est le président de la Section de psychopharmacologie de la SCP. Il détient un doctorat en neurosciences, une formation postdoctorale en neurologie, une maîtrise en psychiatrie scientifique axée sur la médication, et d’autres formations sur les lésions médullaires et en psychologie du counselling. Le Dr Sepehry enseigne actuellement à l’université Adler de Vancouver, collabore avec l’université de la Colombie-Britannique et travaille avec des neuropsychologues médico-légaux sur des cas de nature juridique et médicale. Il affirme que la discipline de la psychopharmacologie est à la fois très ancienne et très nouvelle.
« Elle remonte aux temps anciens où les gens de diverses spécialités utilisaient des substances psychoactives, des herbes et ainsi de suite pour traiter les maladies mentales. Cependant, on constate une incroyable accélération depuis cinq ans, parce qu’il s’est produit beaucoup de choses. C’est en partie dû à l’actuelle crise du SARS-COVID-19. Quelques développements mineurs surviennent pendant que plusieurs d’entre nous tentent de repositionner les médicaments. »
La réaction immunitaire antivirale normale d’une personne exige l’activation des voies inflammatoires du système immunitaire. Les cytokines sont produites dans le contexte de la réaction immunitaire. Une réaction immunitaire incontrôlée et excessive est connue sous le nom de cascade de cytokines ou tempête de cytokines. Ceci peut causer des dommages aux tissus, ce qu’on a observé dans plusieurs cas de COVID-19 graves et survient en raison d’une surabondance de cytokines pro-inflammatoires. Le Dr Sepehry souligne que c’est l’un des angles sous lequel les psychopharmacologues examinent le repositionnement des médicaments existants.
« Les antidépresseurs ont montré des propriétés anti-inflammatoires. Ils pourraient donc être utilisés pour contrer les cascades de cytokines qui sont produites par la COVID. Nous en sommes encore au stade où nous devons déterminer les effets à long terme de la COVID sur le cerveau et le comportement, sur les changements sur le plan de la personnalité, sur la maladie mentale et sur l’éventuel rétablissement. Nous avons besoin de l’engagement d’un plus grand nombre de psychologues. Nous savons qu’il y a des taux croissants de maladie mentale, particulièrement chez les personnes âgées qui ont contracté la COVID. Ainsi, l’apport de la psychopharmacologie est crucial. »
Selon la Dre Velikonja, il existe d’autres manières d’étudier les médicaments, en particulier dans le contexte de la COVID, au fur et à mesure que nous comprenons ses effets à court et à long terme.
« Les médicaments pourraient être repositionnés pour traiter certaines choses comme la fatigue, ce que les gens appellent le brouillard mental, qui, avec d’autres symptômes, est présent dans ce que l’on désigne comme la COVID longue. Lorsque les gens manquent d’énergie ou de motivation physique pour faire des choses, il y a probablement lieu de cibler ce domaine. »
Au cours des deux dernières années, on a observé une mobilisation sans précédent de l’expertise scientifique mondiale. Les experts de presque toutes les disciplines scientifiques se sont réunis pour aborder chaque aspect de la pandémie, et le travail interdisciplinaire et transdisciplinaire atteint des sommets inégalés. Les psychopharmacologues ont l’habitude du travail interdisciplinaire et ils apportent une vaste étendue d’expertise à cette arène scientifique. La Dre Velikonja considère que leur engagement dans ce gigantesque effort est essentiel.
« Je crois que cela est primordial à de nombreux égards, au sens où tout le monde parle de la prochaine vague, ce qui est en réalité la vague de la santé mentale. Nous connaissons les nombreux défis du domaine de la psychiatrie, notamment sur le plan du nombre de praticiens disponibles. Je crois que les psychologues sont bien placés pour jouer ce rôle, pour travailler de concert avec la psychiatrie afin d’examiner la question de la prescription de médicaments et l’intégration de stratégies comportementales. Nous aurons besoin que tous mettent la main à la pâte pendant que se déploie la vague de problèmes de santé mentale. »
Cette vague est en mouvance actuellement, et nous constatons la montée des situations de violence familiale, ainsi que l’augmentation des taux de dépression, d’anxiété, de traumatismes et de problèmes de toxicomanie. Personne ne sait à quoi ressemblera cette vague dans quelques mois ou quelques années. Mais quand elle déferlera, nous devrons tous vraiment mettre la main à la pâte. Et nous pouvons nous sentir un peu rassurés en sachant que certaines de ces mains appartiendront à des personnes qui ont passé des années à devenir des experts dans leur domaine respectif, des scientifiques pour qui apprendre une seule chose n’est pas suffisant, qui veulent en apprendre toujours plus. Vous savez, les passionnés…

Dr Kerry Mothersill

Dre Kelsey Collimore

Dre Stephanie
Greenham
Dr Kerry Mothersill, Dre Kelsey Collimore, et Dre Stephanie Greenham, Psychologues en milieux hospitaliers et en centres de santé
Plusieurs psychologues travaillent dans le système public de soins de santé, certains dans les hôpitaux et d’autres, dans les centres de santé comme membres d’équipes interdisciplinaires traitant une grande diversité de patients. Les Drs Kelsey Collimore, Stephanie Greenham et Kerry Mothersill nous proposent certaines réflexions sur leur travail.
Psychologues en milieux hospitaliers et en centres de santé
Brooke d’Hondt n’a que seize ans, et elle a déjà une équipe d’entraîneurs et d’experts qui l’aident à exceller en snowboard demi-lune. Brooke a terminé à la dixième place à l’épreuve de demi-lune en planche à neige pour le Canada aux Jeux olympiques de Beijing, et lorsque les Jeux seront terminés, elle retournera à l’école. Imaginez être dans son cours de gymnastique!
La psychologie du sport a en quelque sorte émergé des cours de gymnastique; l’éducation physique est née dans le monde de l’éducation et a évolué au fil du temps vers la psychologie du sport que nous connaissons aujourd’hui. Habituellement, les programmes d’études supérieures en psychologie du sport sont dispensés dans les écoles de kinésiologie des universités. Ils offrent des diplômes qui produisent des scientifiques spécialistes de la psychologie du sport.
Aujourd’hui, deux voies principales s’offrent aux personnes qui souhaitent exercer la psychologie du sport et deux types de titres de compétences existent en Amérique du Nord. L’un d’eux est le psychologue agréé, dont le champ d’activité est le plus vaste lorsqu’il a acquis la formation et l’expérience nécessaires pour se dire spécialisé en psychologie du sport et de l’exercice ou en psychologie de la performance. L’autre est un professionnel appelé « conseiller en performance mentale » (CPM). Les personnes qui détiennent ce titre sont titulaires de diplômes scientifiques et ont suivi une formation appliquée, mais leur champ d’activité est limité à l’application des connaissances psychologiques dans le contexte de la performance ou du sport.
La Dre Zarina Giannone a emprunté ces deux voies. Psychologue agréée spécialisée en psychologie du sport et de la performance, la Dre Giannone a fait sa formation de deuxième cycle en psychologie du counseling, mais a suivi une formation appliquée en psychologie du sport (le CPM).
« La psychologie du sport est l’un des domaines de la science du sport au sens large, explique-t-elle. Même mon propre travail en tant que psychologue du sport n’est qu’une petite part d’un plus grand gâteau, dans la mesure où il couvre l’application de la psychologie de la performance. Il consiste à prendre des données scientifiques et théoriques et à les appliquer à des situations réelles. »
La question de la santé mentale des athlètes n’a jamais été autant sous les projecteurs qu’aujourd’hui. Des athlètes de haut niveau parlent de leur santé mentale, se retirent de leur sport pour prendre soin de leur santé mentale et rendent publiques leurs difficultés. Naomi Osaka, Simone Biles, Calvin Ridley, Clara Hughes, Andy Robertson. La liste des athlètes qui ont commencé à parler publiquement de la santé mentale s’allonge de jour en jour. C’est une tendance qui enthousiasme la Dre Giannone.
« Même pendant mes sept années d’études supérieures, j’ai remarqué certains changements très intéressants. Au début des années 2000, le domaine se concentrait davantage sur les aptitudes mentales traditionnelles enseignées aux équipes, aux athlètes et aux entraîneurs. Imagerie mentale, régulation de l’éveil, contrôle de l’attention, ce genre de choses. Ce sont des compétences importantes qui, si elles sont bien maîtrisées par les athlètes, peuvent améliorer leurs performances. Il s’agit également de compétences transférables qui peuvent améliorer le bien-être général et le fonctionnement quotidien. Ces derniers temps, les psychologues et les CPM personnels sont de plus en plus recherchés. Cela s’explique, entre autres, par le fait que les athlètes se sentent plus à l’aise pour divulguer leurs problèmes de santé mentale. La stigmatisation associée à ces problèmes a diminué. Cela signifie que le rôle des psychologues dans les clubs et les organismes sportifs est plus prisé qu’avant. »
Les Colts d’Indianapolis, par exemple, ont lancé une initiative appelée Kicking The Stigma et le porte-parole de la campagne est le défenseur vedette Darius Leonard, qui parle ouvertement de ses crises d’angoisse et de sa dépression. Mais pour chaque équipe qui s’attaque aux problèmes de santé mentale et tente de lutter contre la stigmatisation qui leur est associée, il semble y avoir un autre groupe qui tarde à faire de même. La Ligue canadienne de hockey a récemment publié un rapport dévastateur sur l’existence d’un « code du silence » qui a permis à l’inconduite à l’extérieur de la patinoire de devenir une « norme culturelle ».
« Je connais certaines organisations et certaines équipes qui prennent la santé mentale très au sérieux, et il y a des psychologues du sport qui sont impliqués dans la résolution de problèmes dans une perspective de justice sociale, poursuit la Dre Giannone. Par exemple, ceux qui travaillent avec des cas d’abus ou d’inconduite sexuels. Ces psychologues ont contribué à la création de changements systémiques dans certaines organisations. On observe de plus en plus de politiques de santé mentale, ou de politiques de diversité et d’inclusion être mises en œuvre dans les organisations. J’espère que les gens en ressentiront les effets, et que ce ne sera qu’une question de temps avant que toutes les grandes organisations sportives emboîtent le pas. »
Pour la première fois depuis longtemps, les joueurs de la LNH ne sont pas présents aux Jeux olympiques. Cela signifie que les équipes de hockey qui s’affrontent se répartissent en deux catégories : soit un groupe de joueurs qui jouent ensemble dans un contexte ou un autre depuis longtemps, soit une équipe composée des meilleurs joueurs disponibles qui ont peu d’expérience de jeu entre eux. Comment créer une dynamique de groupe et développer la confiance de l’équipe? Selon la Dre Giannone, ces questions sont de plus en plus du ressort des psychologues du sport et des CPM.
« Les psychologues du sport ne se contentent plus d’offrir des formations classiques sur les aptitudes mentales et de simples évaluations des compétences mentales. Aujourd’hui, mon travail se concentre sur l’optimisation des performances, mais il concerne également d’autres difficultés propres au sport, notamment la dynamique de groupe entre les membres de l’équipe, le leadership des entraîneurs et la gestion de divers problèmes de santé mentale rencontrés par les athlètes, comme l’épuisement professionnel, la dépression, l’anxiété ou les troubles de l’alimentation. À bien des égards, le rôle du psychologue du sport a été réinventé et consiste désormais à répondre à la fois aux besoins psychologiques et aux exigences de la performance inhérentes au sport. »
La Dre Giannone travaille principalement en pratique privée au Vancouver Psychology Centre, où elle reçoit des clients en psychologie générale et d’autres personnes qu’elle aide en sa qualité de psychologue spécialisée en psychologie du sport et de la performance. Dans cet espace, elle voit un large éventail d’athlètes et d’artistes – des jeunes jusqu’aux professionnels. À l’occasion, elle accepte un contrat avec une équipe, pour laquelle elle met en œuvre un programme de développement des aptitudes mentales ou fournit d’autres services de groupe. Elle travaille également avec le Canadian Centre for Mental Health in Sport (CCMHS), où elle offre des services de santé mentale aux athlètes et aux artistes.
« Depuis 2013, le financement fédéral de ces services a vraiment augmenté, et ce, assez rapidement. Il existe aujourd’hui quelques services financés par le gouvernement fédéral destinés aux sportifs de niveau national. Par exemple, il y a le programme Plan de match, qui offre une vaste gamme de services aux athlètes brevetés de haut niveau au Canada. Mon rôle au CCMHS s’adresse à tous les sportifs, entraîneurs et administrateurs, quel que soit leur niveau, et permet à certaines personnes d’accéder à du financement à cet effet. Les autres pays sont un peu en retard dans ce domaine, ce qui fait du Canada un chef de file dans la sphère de la santé mentale des sportifs. »
Comme c’est le cas de tous les événements majeurs des deux dernières années, la COVID est une question centrale des Jeux olympiques de 2022. Elle a perturbé l’entraînement, entravé la consolidation des équipes et fait perdre à de nombreux athlètes la chance de concourir sur la scène mondiale. La COVID a même coûté à certains athlètes la chance de concourir après leur arrivée aux Jeux, lorsqu’un test positif a mis fin prématurément à leur parcours olympique. La Dre Giannone a vu tous les hauts et les bas créés par la pandémie chez les athlètes de tous les niveaux.
« Au début, les sports étaient sur pause. Les tournois importants ont été reportés. À ce moment-là, il fallait vraiment modifier et faire évoluer les services psychologiques vers un mode de prestation en ligne. Nous avons fait des choses en équipe avec plus de 25 personnes sur Zoom! Au cours de la dernière année, de nombreux athlètes ont repris le sport, et il se présente des défis nouveaux auxquels nous n’avons jamais été confrontés auparavant. Le contenu du travail a changé – imaginez un jeune athlète qui n’a participé à aucune compétition au secondaire depuis deux ans. Il était en secondaire 2, et il est maintenant en secondaire 4. Ce que cela représente pour ces jeunes sur le plan du développement et du perfectionnement des compétences propres au sport est intéressant.
Mes recherches portent principalement sur le développement de l’identité dans le sport. Ce qui arrive lorsqu’une personne se blesse ou prend sa retraite, et la perte d’identité qui en découle. La COVID est à l’origine d’un grand nombre de menaces pour l’identité, qu’il s’agisse d’enfants ou d’athlètes olympiques. Ces personnes qui tirent du sport une telle estime de soi et une telle valeur sont involontairement contraintes de le mettre de côté pendant un certain temps. Cela peut être très déstabilisant pour les gens.
Je dirais, à l’inverse, que la COVID a offert aux athlètes une occasion inédite de pratiquer leur sport d’une manière nouvelle et différente. Prenons l’exemple d’un sportif qui n’avait jamais le temps de regarder des vidéos de lui-même. Désormais, il est capable d’apprendre des choses différentes sur lui-même. Il est peut-être capable de faire un peu plus de musculation. J’ai été frappée par la résilience et la créativité dont ont fait preuve les gens durant cette période.
Ce qui m’a vraiment frappée au début de la pandémie, c’est le passage de l’entraînement aux compétences physiques et mentales à la création de nouvelles conceptions de la culture d’équipe. Je me souviens d’être intervenue dans des équipes et d’avoir aidé à faciliter la réalisation des objectifs, et à cultiver les valeurs de l’équipe et les relations entre ses membres. Cela ne veut pas dire que je ne le ferais pas pendant une saison régulière, mais la pandémie a vraiment mis cela en évidence car il n’y avait pas grand-chose d’autre à faire quand la situation était si incertaine. »
La santé mentale des athlètes est un domaine en expansion rapide. Le rôle des psychologues dans la résolution de certains problèmes sociaux et systémiques tels que les comportements inappropriés des athlètes, la violence dans le sport, les abus et le harcèlement, l’inclusion et la diversité culturelle, devient de plus en plus important. Les psychologues participent à la création de mesures de soutien, mais aussi à la promotion de changements systémiques au sein des systèmes et des organisations, et tout cela se répercute sur les athlètes. Mais leur influence et leur implication ne se limitent plus aux vestiaires.
Comme l’évoque la Dre Giannone, « les professionnels de la psychologie du sport sont désormais sortis du cadre traditionnel du sport et de l’exercice. Ils s’occupent des problèmes liés à la performance dans d’autres domaines. Il n’est pas rare de voir des psychologues du sport travailler avec des militaires, des artistes de la scène, des premiers intervenants ou des dirigeants d’entreprise de haut niveau. Presque tout le monde se retrouvant dans des situations très stressantes. Je m’attends à voir davantage de psychologues possédant ces compétences spécialisées se frayer un chemin dans divers milieux. »
Les Jeux olympiques, qui se déroulent en ce moment même, présentent une gamme de situations stressantes pour les athlètes, sous le regard du public, tous les jours, toute la journée. Nous pouvons nous réjouir de la performance improbable de l’équipe canadienne en poursuite par équipes de patinage de vitesse, mais aussi compatir à la douleur de l’équipe japonaise, dont la chute de l’une de ses membres a donné la médaille d’or au Canada. Nos yeux, les yeux du monde, ajoutent une pression inédite pour ces sportifs. Cette situation peut être difficile, et un psychologue peut aider l’athlète à y faire face. Que vous soyez Jennifer Jones, qui participe à ses deuxièmes Jeux olympiques à l’âge de 47 ans ou une planchiste de 16 ans, qui s’apprête à retourner à ses cours de géographie.

Dr Jude Mary Cénat

Dre Helen Ofosu

Anita Shaw
Dr Jude Mary Cénat, Dre Helen Ofosu, Anita Shaw, Kafui Sawyer, Dre Erin Beettam, et Dre Monnica Williams, Section de Personnes Noires en Psychologie

Kafui Sawyer

Dre Erin Beettam

Dre Monnica Williams
L’une des deux nouvelles sections de la SCP est la Section de la psychologie des Noirs; elle vise à accroître la présence des professionnels de la psychologie noirs et à accroître l’accès aux services de santé mentale pour la communauté noire.
Section de Personnes Noires en Psychologie
« Quel domaine peut être plus antiraciste que la psychologie? Nous sommes là pour soutenir les êtres humains, le développement de la personne et le bien-être des individus! Il n’y a pas de domaine qui puisse aborder les questions raciales aussi bien que la psychologie. »
Jude Mary Cénat, Ph. D., se passionne pour la lutte contre le racisme en psychologie et invite ses collègues du secteur de la santé mentale à se joindre au mouvement. Le Dr Cénat est professeur agrégé à l’École de psychologie de l’Université d’Ottawa et le directeur du Laboratoire de Recherche Vulnérabilité, Trauma, Résilience et Culture (V-TRaC).
Au Canada, les populations racisées vivent des traumatismes et des problèmes de santé mentale qui leur sont propres. Les Canadiens noirs ne font pas exception. En plus des choses qui touchent tout le monde – la pandémie, le stress au travail, les problèmes familiaux –, ils doivent faire face au racisme sociétal, ainsi qu’à l’hostilité et aux microagressions au travail, qui font partie de la vie quotidienne dans notre pays.
« Nous ne pouvons continuer à perpétuer et à encourager la discrimination raciale. Nous ne pouvons continuer à nous contenter d’être une société “sans préjugés raciaux”. Les personnes qui connaissent de hauts niveaux de discrimination raciale sont trente-six fois plus susceptibles de présenter des symptômes graves de dépression. »
La volonté de s’assurer que la psychologie joue le rôle de chef de file qu’elle peut et doit jouer dans la résolution des problèmes raciaux est l’un des principes qui ont amené cinq membres et affiliées de la SCP à devenir la force motrice de la création d’une nouvelle section, la Section de la psychologie des Noirs. Kafui Sawyer, Anita Shaw, la Dre Helen Ofosu, la Dre Monnica Williams et la Dre Erin Beettam ont donné à la section la mission de soutenir et de servir les praticiens, les éducateurs, les étudiants et les scientifiques du domaine de la psychologie qui s’identifient comme Noirs et qui s’intéressent aux questions de nature psychologique qui ont une incidence sur la population noire. Chacune d’entre elles a vu l’impact de la discrimination raciale, certaines personnellement, au cours de sa carrière.
La Dre Helen Ofosu est psychologue du travail et des organisations, coach pour cadres et conseillère en ressources humaines à Ottawa. Elle travaille avec des organisations, y compris des ministères, pour améliorer la culture organisationnelle et l’inclusion. Dans les deux dernières années, depuis le début de la pandémie, elle a remarqué que beaucoup d’employés racisés décident de chercher du travail dans des organisations plus inclusives, car ils se rendent compte qu’en travaillant à domicile, ils ne sont plus soumis aux outrages quotidiens qu’ils subissent dans un lieu de travail physique. « Ce genre de choses se produit depuis des années, mais maintenant, les gens ne sont plus dans leur environnement habituel, et ils ont la tranquillité d’esprit que procure le fait de pouvoir travailler sans se soucier des microagressions ou craindre de se faire regarder de travers ou d’être exclus des déjeuners, des pauses-café et des conversations. Lorsque tout cela disparaît, les gens se sentent beaucoup plus détendus car ils peuvent se concentrer sur leur travail.
Je crois que le véritable déclencheur a eu lieu à l’été 2021, au moment où de nombreuses organisations planifiaient le retour au travail de leurs employés dans leurs locaux. Ce n’est que lorsque les gens ont commencé à réaliser “Oh mon Dieu, je vais peut-être devoir retourner au bureau” qu’ils se sont mis à se dire “Un instant! Je ne pense pas être capable de retourner au bureau. Je ne veux pas retourner au bureau! Je ne veux pas retourner à ce que les choses étaient avant.” »
Pendant tout ce temps de réflexion, beaucoup de gens ont jugé qu’il était opportun pour eux de changer d’emploi et de trouver un lieu de travail où il y a plus de représentation, plus d’inclusion, plus de diversité, en somme, un milieu où il y a une meilleure culture organisationnelle. D’après ce que j’ai vu, les gens réfléchissent à plein de choses pendant la pandémie. Ils tentent donc de trouver un emploi où ils peuvent être eux-mêmes et se concentrer sur leur travail au lieu de chercher continuellement à se protéger contre toutes ces agressions psychologiques. »
Anita Shaw est étudiante au doctorat à l’Université de Northern British Columbia.
« Pendant que je fais mon doctorat, je réfléchis vraiment à la décolonisation, raconte-t-elle. Non seulement la décolonisation de ma propre pensée, mais aussi la façon dont la psychologie a contribué à la colonisation et comment elle pourrait contribuer à la décolonisation. J’ai travaillé avec un mentor qui est un chercheur autochtone, et nous avons élaboré un modèle de programme de cours visant à décoloniser la psychologie. »
Kafui Sawyer est une psychothérapeute, une consultante en traumatologie pour Santé Canada et la directrice clinique du Joy Health and Research Centre. Elle aide les familles à traverser des expériences traumatisantes, aide les employés du gouvernement qui ont vécu certaines expériences et situations difficiles (comme le racisme) dans leur milieu de travail, et bien plus encore. Souvent, les clients demandent de travailler avec elle, car elle est Noire et a un vécu commun avec eux. Pour elle, ce qui est le plus gratifiant, c’est de travailler sur des cas complexes comme les troubles de la personnalité, et de voir ses clients passer d’une personnalité pathologique à une personnalité plus saine.
Comme le mentionne Mme Sawyer, ce qu’espèrent les fondatrices de la section, c’est « créer un espace où des gens qui ont des valeurs et des croyances similaires peuvent faire bouger les choses. Nous espérons que la section rassemblera des personnes animées du même esprit afin de prendre notre place au sein de la SCP. » Pour les fondatrices, la section offre l’occasion de créer un espace où les gens peuvent mettre en commun leurs intérêts et leurs expériences de manière à « se donner les moyens de devenir meilleurs ».
De plus, la Section de la psychologie des Noirs est un espace important pour les alliés des membres, des étudiants et des affiliés noirs. La Dre Erin Beettam s’identifie comme une psychologue clinicienne pour enfants et adolescents. Bien qu’elle ait reçu une formation en psychologie scolaire, elle travaille principalement dans les hôpitaux, en pédopsychiatrie et dans le système public de santé mentale. Erin se spécialise dans le traitement des adolescents et des jeunes adultes qui souffrent d’anxiété, de dépression, de troubles de la personnalité en émergence et de troubles de l’alimentation. Elle travaille actuellement dans une commission scolaire et exerce en pratique privée. Elle mentionne qu’elle est de plus en plus consciente de « l’absence de services accessibles et efficaces pour les personnes de couleur, pour les communautés noires, dans les milieux de travail et dans les milieux d’enseignement ». Cette prise de conscience l’a amenée à examiner ce qu’elle « peut donner et faire pour apporter son soutien dans ce paysage en mutation ».
La Dre Monnica Williams est chercheuse à l’Université d’Ottawa et milite depuis longtemps pour l’inclusion dans la recherche. Pendant trop longtemps, les personnes de couleur ont été exclues des recherches de toutes sortes, notamment dans divers domaines de la psychologie.
« Une grande partie de la recherche qui se fait exclut d’emblée la diversité, et non seulement elle perpétue le problème, mais elle en est aussi le symptôme. Le fait que nous n’ayons pas assez de chercheurs de couleur pour faire des recherches pour les personnes de couleur est une partie du problème.
Je fais beaucoup de recherches pour mettre en lumière ces questions – comment les traitements doivent être adaptés aux personnes de couleur, comment les thérapeutes qui sont actuellement en formation peuvent en apprendre davantage sur la manière de traiter les gens dans une optique plus inclusive. Tout le monde doit comprendre les meilleures pratiques lorsqu’il s’agit de travailler avec les questions raciales, ethniques et interculturelles. »
Le collègue de la Dre Williams à l’Université d’Ottawa, le Dr Cénat, fait également la promotion de ces meilleures pratiques en matière de race, d’ethnicité et d’interculturalisme. Ses collègues et lui ont créé un cours appelé « Comment fournir des soins de santé mentale antiracistes », qui donne droit à des crédits de formation continue approuvés par la SCP. Le Dr Cénat espère que tous les professionnels de la santé mentale et les Canadiens en général s’engageront dans la lutte contre le racisme.
« Comme l’a dit Ikram Kendi, il n’y a pas de “racistes” et de “non-racistes”. Il y a des “racistes” et des “antiracistes”. Si vous êtes simplement “non raciste”, vous ne posez pas de geste qui puisse contrer le racisme. Et ce n’est qu’en agissant contre le racisme que nous créerons une société antiraciste. »
La Section de la psychologie des Noirs, dont la création a été approuvée par le conseil d’administration de la SCP en novembre 2021, recrute désormais des membres. Une fois que les membres seront réunis, la section proposera son mandat au conseil d’administration de la SCP aux fins d’approbation, et procédera ensuite à l’élection de son comité exécutif; toutes ces démarches devraient être achevées en 2022. L’objectif de la section sera de travailler avec d’autres intervenants pour accroître la présence de professionnels noirs en psychologie et faciliter l’accès de la communauté noire aux services de santé mentale, de mieux-être et de consultation, ainsi qu’aux services organisationnels, en mettant l’accent sur les membres de cette communauté qui ont de la difficulté à avoir accès aux soins de santé mentale appropriés et à d’autres services psychologiques (p. ex., formation, leadership, interventions organisationnelles, recherche fondamentale et appliquée, etc.). La section pourra éventuellement devenir un espace communautaire pour les membres, les affiliés et les étudiants affiliés de la SCP qui s’intéressent à ces questions et, en particulier pour les étudiants, les éducateurs, les chercheurs et les psychologues noirs. Pour en savoir plus sur la façon de se joindre à la section, rendez-vous à l’adresse https://cpa.ca/fr/sections/black-psychology/.
 Dre Monnica Williams
Dre Monnica WilliamsFévrier, c’est le Mois de l’histoire des Noirs, et la SCP met en vedette des psychologues noirs contemporains tout au long du mois. La Dre Monnica Williams est chercheuse à l’Université d’Ottawa et se consacre à rendre la recherche plus ouverte aux personnes de couleur. En particulier, aujourd’hui, la recherche sur la médecine psychédélique.
La Dre Monnica Williams est thérapeute, auteure et chercheuse à l’Université d’Ottawa (entre autres choses, la liste de ses titres de compétences étant très longue). Elle a une longue expérience du militantisme, de l’activisme et de la défense de la justice sociale et s’est spécialisée dans la problématique des disparités raciales dans le domaine de la santé, de la recherche et ailleurs. Experte des troubles anxieux, elle est actuellement l’une des très rares personnes à faire de la recherche sur l’inclusion des personnes de couleur dans la médecine psychédélique.
« Une grande partie de mes recherches a été consacrée aux traumatismes, particulièrement aux traumatismes vécus par les personnes racisées, qui sont liés au racisme, et à la façon d’aider le mieux possible les personnes qui en souffrent. Lorsque j’ai appris, il y a six ou sept ans, que des recherches étaient menées sur l’utilisation de la MDMA pour le traitement du SSPT, j’ai été très intéressée. Premièrement, est-ce que ça fonctionne? Si l’on regarde les essais cliniques et les recherches qui ont été menées, il semble que ce soit très efficace. Et deuxièmement, est-ce que cela fonctionnera chez les gens de couleur? Il était évident que si la recherche était prometteuse, elle n’était pas inclusive.
Le fait de voir des millions et des millions de dollars investis dans cette nouvelle approche thérapeutique, qui, à mon avis, va vraiment changer la donne pour la santé mentale, et de constater en même temps que les personnes de couleur n’en font pas partie, m’a inquiétée – et m’a mise un peu en colère, en fait. C’est bon pour les Blancs, alors pourquoi n’en profitons-nous pas?
J’ai donc entrepris de faire des recherches à ce sujet afin de pouvoir quantifier le degré d’exclusion que nous subissons. J’espérais aussi que cela puisse servir d’appel à l’action – pour sensibiliser les gens au fait que nous devons être inclus et que notre opinion doit être entendue, et que les approches thérapeutiques doivent être adaptées à nos communautés. Il ne s’agit pas seulement de ce que l’on pourrait considérer comme un client blanc typique de la classe moyenne, mais de toute une variété de personnes qui pourraient bénéficier de ces traitements.
Il est également important de souligner que non seulement un grand nombre de ces médicaments psychédéliques ont été volés aux cultures autochtones, mais que certaines méthodes ont également été volées aux cultures autochtones. Nous devons donc être conscients de cela lorsque nous abordons ces recherches. »
La Dre Williams est depuis longtemps une défenseur de l’inclusion dans la recherche. Depuis trop longtemps, les personnes de couleur sont exclues des recherches de toutes sortes, notamment dans divers domaines de la psychologie.
« Une grande partie de la recherche qui se fait exclut d’emblée la diversité, et non seulement elle perpétue le problème, mais elle en est aussi le symptôme. Le fait que nous n’ayons pas assez de chercheurs de couleur pour faire des recherches pour les personnes de couleur est une partie du problème. Certes, il y a beaucoup de Blancs qui font des recherches sur ces populations, mais nous devons aussi être inclus. Comme le dit le dicton, « Rien pour nous sans nous ». Le milieu de la recherche doit nous représenter et nous devons en faire partie.
Une des choses importantes que je préconise est une plus grande inclusion : ouvrir les portes de nos établissements d’enseignement à des thérapeutes de couleur et souligner la nécessité d’y être inclus. Je fais également beaucoup de recherches pour mettre en lumière ces questions – comment les traitements doivent être adaptés aux personnes de couleur, comment les thérapeutes qui sont actuellement en formation peuvent en apprendre davantage sur la manière de traiter les gens dans une optique plus inclusive. Même les rares thérapeutes de couleur qui réussissent sont formés pour traiter les Blancs. Par conséquent, tout le monde doit comprendre les meilleures pratiques lorsqu’il s’agit de travailler avec les questions raciales, ethniques et interculturelles. »
La Dre Williams explique que, pendant ses études et par la suite, elle n’a pas pu trouver de mentor noir dans son établissement d’enseignement, et c’est pourquoi il est très important pour elle de servir de mentor à autant d’étudiants que possible qui se trouvent dans la même situation qu’elle lorsqu’elle était aux études.
« Je fais beaucoup de mentorat auprès des étudiants de couleur, parce que je n’ai pas pu bénéficier de ce genre de mentorat. Lorsque j’étais une jeune psychologue, au début de ma carrière, la personne qui était censée me servir de mentor était en fait assez violente. Je suis donc allée ailleurs et j’ai trouvé mes propres mentors à la Delaware Valley Association of Black Psychologists. J’ai travaillé avec quelqu’un là-bas, et c’était bien. Le travail que je faisais et ce qu’il faisait ne correspondaient pas exactement, mais j’étais vraiment heureuse que des Noirs me soutiennent, m’encouragent et croient en moi. C’était très différent de mon environnement actuel, et cela a beaucoup compté. »
Malheureusement, encore aujourd’hui, les établissements d’enseignement n’offrent pas tous un environnement inclusif et accueillant pour les étudiants ou les professionnels noirs. C’est pourquoi Monnica a choisi d’aller ailleurs lorsqu’elle était une jeune psychologue, et c’est pourquoi les personnes de couleur cherchent souvent à aller ailleurs aujourd’hui. La création de ces espaces inclusifs fait partie de la mission qu’elle s’est donnée, et c’est un objectif dont le reste du Canada – dans les établissements d’enseignement et ailleurs – devrait se rapprocher.

Dr Vinay Bharadia

Dre Kristina Gicas
Dr Vinay Bharadia et Dre Kristina Gicas, Neuropsychologie clinique
Notre cerveau et notre corps entretiennent une relation, parfois harmonieuse, parfois conflictuelle. C’est le domaine de la neuropsychologie clinique. Nous avons parlé au Dr Vinay Bharadia et à la Dre Kristina Gicas pour en savoir plus.
Le mot « neuropsychologie » est difficile à prononcer. Il ressemble à un mot que l’on utilise pour avoir l’air intelligent. Comme « nomenclature » ou « cumulatif ». Comme il faut beaucoup de temps pour le dire, les neuropsychologues ont trouvé un moyen astucieux de raccourcir ce terme – ils disent plutôt « neuropsy ». Le fait d’omettre les deux dernières syllabes a sans aucun doute permis, au fil des décennies, d’économiser un nombre incalculable d’heures de conversation dans les départements universitaires de partout au Canada.
Ajoutez le mot « clinique » et vous voilà dans un tout nouveau monde, à la nomenclature encore plus complexe. Et ce monde, la Dre Kristina Gicas, présidente de la Section de neuropsychologie clinique de la SCP, est heureuse de le faire découvrir. La Dre Gicas est neuropsychologue clinicienne et professeure adjointe à l’Université York, où elle forme des étudiants en neuropsychologie clinique. Elle enseigne, fait de la recherche et exerce aussi des activités cliniques à Toronto.
« La neuropsychologie clinique est l’étude de la relation entre le cerveau et le comportement, dit-elle. Nous examinons la structure et le fonctionnement du cerveau, et nous étudions comment ces éléments sont reliés aux capacités de réflexion. Cela comprend l’attention, la mémoire, le langage, les habiletés visuelles, la vitesse de traitement et même le fonctionnement émotionnel. »
Les neuropsychologues sont des spécialistes de l’étude de ces relations entre le cerveau et le comportement, et de l’utilisation de ces informations à diverses fins. La première chose qu’ils font est de diagnostiquer certaines choses comme les blessures ou les maladies qui touchent le cerveau (commotion cérébrale, accident vasculaire cérébral, tumeurs, démence). Ils cherchent également à comprendre le développement normal de la personne et son vieillissement. Un autre domaine de spécialisation des neuropsychologues est la conception et la mise en œuvre d’interventions visant à améliorer le fonctionnement quotidien des individus.
La SCP désigne cette section sous le nom de « neuropsychologie clinique », car tous les neuropsychologues reçoivent d’abord une formation de psychologue clinicien. Le volet « neuropsychologie » est une spécialisation, que les praticiens acquièrent en suivant des cours supplémentaires, par exemple, des cours de doctorat en neuroanatomie (un autre mot difficile à prononcer – seulement, celui-ci est difficile à contracter). Ils apprennent ce que sont les outils d’évaluation et les tests cognitifs, ce qu’ils signifient et comment ils sont utilisés. La plupart des psychologues peuvent faire passer ces tests, mais ce sont les neuropsychologues qui peuvent les relier au fonctionnement du cerveau – la relation entre cerveau et comportement dont il est question ci-dessus.
Vous avez peut-être remarqué que l’un de vos parents commence à perdre la mémoire et à être moins attentif aux tâches qu’avant. Vous pourriez l’amener chez le médecin, qui pourrait alors lui faire passer un test, comme le MoCA Test (Montreal Cognitive Assessment). Il s’agit d’une évaluation préliminaire qui peut aider à déterminer dans quelle mesure une intervention est nécessaire. Si votre parent atteint un certain seuil, il pourrait être dirigé vers un neuropsychologue clinicien, comme le Dr Vinay Bharadia.
Le Dr Bharadia partage son temps entre un cabinet privé, les Cliniques TELUS Santé, où il occupe le poste de responsable de la neuropsychologie, et l’Université de Calgary, où il forme des psychologues au niveau du doctorat et de la maîtrise. Il travaille principalement avec des personnes souffrant de lésions cérébrales, de démence, de la maladie de Parkinson, de la sclérose en plaques et d’autres pathologies neurologiques qui affectent la fonction cognitive.
« Si vous êtes dirigé vers nous, nous effectuons des tests plus poussés de la mémoire, de l’attention et d’autres capacités cognitives, après que votre médecin généraliste a effectué un test de dépistage, comme le MoCA Test, explique-t-il. Nous recherchons également des signes de dépression et d’anxiété, car ils peuvent également affecter les capacités cognitives. Nous établissons ensuite un lien entre les tests que nous effectuons et l’hippocampe ou le thalamus – des parties du cerveau que nous savons liées à la mémoire – ou d’autres zones et réseaux neuronaux. Nous examinons vos antécédents médicaux, les résultats de vos tests d’IRM et de tomodensitogramme, etc., et nous tentons de poser un diagnostic ou de déterminer le traitement à prodiguer. »
Une grande partie des recherches effectuées par les spécialistes des sciences cognitives, comme Jonathan Wilbiks, de la Section cerveau et science cognitive (voir l’article précédent du Mois de la psychologie), influencent le travail des neuropsychologues cliniciens. Les spécialistes des sciences cognitives produisent des recherches et des données, et il revient ensuite aux neuropsychologues cliniciens d’appliquer ces connaissances dans un cadre clinique pour améliorer la vie de leurs patients. Et ces patients sont très différents selon leur état, leurs symptômes et leur âge.
Le Dr Bharadia poursuit : « Si vous avez 25 ans et présentez des symptômes de dépression, vous ne verrez probablement pas un neuropsychologue. Vous serez plus susceptible de consulter un psychologue clinicien ou un thérapeute, et peut-être un omnipraticien pour la prise de médicaments. Mais si vous avez 55 ans et êtes atteint de dépression, il est à espérer que l’omnipraticien se demande si cela pourrait être autre chose. Qu’est-ce qui ressemble à une dépression dans la cinquantaine? Si l’on tient compte de certains éléments de vos antécédents médicaux et des informations que pourrait révéler une IRM, il pourrait s’agir d’un symptôme de démence frontotemporale, qui ressemble parfois à une dépression dans certains groupes d’âge. À ce moment-là, il serait bon que vous passiez un test avec un neuropsychologue afin d’affiner le diagnostic. »
Cela signifie que les neuropsychologues travaillent beaucoup en équipe, avec les omnipraticiens, les psychiatres, les neurologues qui effectuent des IRM et de nombreux autres professionnels du monde des sciences du cerveau, dont les compétences se chevauchent. Si la personne de 55 ans présentant des symptômes de dépression rencontre cette équipe, celle-ci pourrait déterminer que la cause est neurologique, et dans ce cas, elle suggérera un traitement. Si, toutefois, on détermine que la cause est psychologique, un neuropsychologue pourra travailler avec la personne pour la soigner (car, ne l’oublions pas, les neuropsychologues sont d’abord des psychologues cliniciens).
La neuropsychologie est un domaine officiel qui existe depuis 70 ans. Les travaux précurseurs de la Dre Brenda Milner, à l’Université McGill, réalisés dans les années 1950 avec le patient H.M., ont révolutionné notre compréhension de la mémoire. Ce remarquable travail a été réalisé aux côtés du Dr Wilder Penfield, neurochirurgien. La Dre Milner EXERCE ENCORE à McGill à l’âge de 102 ans. D’autres pionniers ont mis sur pied un programme de neuropsychologie à l’Université de Victoria, où la Dre Gicas a fait son baccalauréat. C’est ce qui l’a conduite sur cette voie (ainsi que sa fascination pour le cerveau et sa passion pour la science en général).
« Je me souviens d’avoir lu un livre d’Oliver Sacks, intitulé L’Homme qui prenait sa femme pour un chapeau (1985), mentionne-t-elle. Ce livre présentait une série de cas neurologiques et je suis tout de suite devenue férue de neuropsychologie. »
Dans un épisode de Parcs et loisirs, Ben ne comprend pas la relation entre Jerry (Jim O'Heir) et sa femme Gayle (Christie Brinkley), visiblement plus belle, et suppose que c’est le résultat d’un trouble neurologique (« l’un des troubles évoqués par Oliver Sacks – elle pense peut-être que Jerry est un chapeau sympa? »). Ce n’est peut-être pas le meilleur exemple de neuropsychologie dans la culture populaire, dans la mesure où il est tout à fait faux – mais ce n’est pas une étude aussi simple à réaliser! À moins que vous ne puissiez contourner l’effet cumulatif de toute cette nomenclature difficile.

Dre Karen Blair

Dr. Rhea Ashley
Hoskin

Bre O’Handley
Dre Karen Blair, Dre Rhea Ashley Hoskin, et Bre O’Handley Orientation sexuelle et identité sexuelle
Le champ de l’orientation sexuelle et de l’identité de genre a grandement évolué au cours des dernières années, de l’obtention du mariage entre personnes de même sexe, en passant par l’abolition des thérapies de conversion. Nous avons discuté de ces progrès avec la Dre Karen Blair, la Dre Rhea Ashley Hoskin et Bre O’Handley. Nous avons aussi abordé une expression que vous n’avez peut-être jamais entendue auparavant, la « féminophobie ».
Orientation sexuelle et identité sexuelle
« Je n’aime plus la bière. »
Un message publicitaire à la télé nous présente un homme qui avoue à l’un de ses amis, en murmurant honteusement, qu’il n’aime plus le goût de la bière. S’installe alors une entente implicite entre nous, les téléspectateurs, et les hommes de la publicité : le fait qu’il n’aime plus la bière atteint son sentiment de masculinité. Que de boire une bière avec les « gars » fait partie de son identité mâle qu’il est honteux de perdre. Et que le fait de ne pas aimer la bière le rend ‘féminin’, et donc moins digne de mérite que les autres.
La Dre Rhea Ashley Hoskin est titulaire de la bourse postdoctorale AMTD Waterloo Global Talent de l’Université de Waterloo, où elle est affectée au département de sociologie et d’études juridiques et à celui des études sur la sexualité, la famille et le mariage. Elle est secrétaire-trésorière de la Section de l’orientation sexuelle et l’identité sexuelle de la SCP. En général, son travail est axé sur la diversité sexuelle et de genre, plus particulièrement sur le traitement sociétal de la féminité et la « féminophobie ».
« La féminophobie évoque la manière dont la société déprécie et régule la féminité et tout le monde peut en être la cible. Elle peut viser un homme cisgenre qui commande une salade, ou qui est vu comme efféminé, parce que la féminité est souvent perçue comme une rétrogradation sociale. Nous observons également la féminophobie qui cible les femmes du domaine scientifique pouvant être vues comme trop ‘féminines’ et être traitées comme si elles étaient incompétentes parce qu’elles sont trop maquillées ou parce qu’elles n’ont pas l’air de scientifiques. »
Dans la publicité, l’ami du protagoniste traite son aveu de ne plus aimer la bière avec un haussement d’épaules et ne semble pas croire que celui-ci soit pour autant un homme diminué. Et puis, évidemment, il lui offre autre chose qu’une bière, un alcool fort, que nous les téléspectateurs supposons être une substitution adéquate et aussi masculine aux yeux de la société.
La féminophobie touche à la fois les gais et les hétérosexuels, les hommes et les femmes, et même les personnes qui s’identifient comme non-binaires. Nous vivons tous, la plupart du temps inconsciemment, les tiraillements entourant la définition de notre personnage public en fonction de ce qui est vu comme féminin. Chacun de nous est, d’une façon ou d’une autre, touché par cette situation, que ce soit les hommes qui commandent une bière régulière au lieu d’une bière légère, par crainte d’être vus comme trop ‘féminins’, ou les femmes qui portent moins de maquillage pour paraître plus intelligentes ou ‘professionnelles’.
La Dre Karen Blair est professeure adjointe de psychologie à l’Université Trent. Elle est la présidente de la Section de l’orientation sexuelle et l’identité sexuelle de la SCP depuis 2014. Ce qui est bien avec la féminophobie, c’est qu’une fois qu’elle a fait tilt, on commence à la voir partout. On commence à remarquer toutes les façons dont nous dévalorisons la féminité. Chez les hommes, nous avons un éventail assez étroit de la « féminité acceptable », et la plupart du temps, nous préférons qu’ils n’en aient aucune. Dans les vestiaires d’une équipe de football, l’entraîneur pourrait, pour invectiver les joueurs de son équipe, dire qu’ils jouent comme « des filles ». C’est dit pour injurier, et les joueurs comprennent le message, et que l’entraîneur est insatisfait. Si un homme a une démarche trop ‘féminine’, parle de manière efféminée, ou parle avec ses mains, il perd des points pour ces raisons. Dans notre société, nous utilisons la féminité comme une arme ou une insulte. »
L’occupation se déployant à Ottawa depuis quelques semaines a donné lieu à une recrudescence des attaques envers le premier ministre, à la fois parmi les insurgés et dans les médias sociaux. La Dre Blair et la Dre Hoskin surveillent ce genre de choses. À quoi ressemblent les attaques dirigées envers les personnalités publiques et les politiciens, et pourquoi la féminophobie en fait-elle si souvent partie?
« Quand les gens veulent attaquer Justin Trudeau, ils posent certains gestes : d’abord, ils ont tendance à l’appeler par son prénom. Quand nous étions irrités par Stephen Harper, nous l’appelions quand même Harper. Mais quand nous sommes irrités par Trudeau, nous employons son prénom, et certains l’appellent même Justine. Pourquoi serait-ce une insulte que d’appeler quelqu’un par un prénom féminin? Pourquoi est-ce insultant de féminiser une autre personne? La réponse est la misogynie et la féminophobie. Ce ne sont pas que les politiciens comme le premier ministre qui en sont la cible; nous faisons cela à tous les niveaux. Quand les gens veulent se moquer de Poutine ou de Trump, l’un des mèmes les plus communs sur Internet est d’ajouter du fard à leurs visages pour leur donner l’allure d’une femme trop maquillée. Peu importe ce que l’on pense de Trudeau, Trump ou Poutine, ils se font tous écraser par la même attaque contre la ‘féminité’. On l’emploie pour affirmer qu’ils sont inférieurs, stupides, idiots, frivoles, ou excessifs. Toutes ces idées peuvent être transmises simplement en les rendant féminines. Ce qui nous donne à penser : que disons-nous vraiment des gens qui sont féminins? C’est un peu comme quand les gens avaient l’habitude de dire “oh, c’est tellement gai”, alors qu’ils voulaient en fait qualifier une chose de stupide ou insignifiante. »
‘Nous’ (la société) avons fait beaucoup de chemin au cours des dernières décennies. Lorsque la Section de l’orientation sexuelle et l’identité sexuelle a été lancée au début des années 2000, la question la plus urgente était le mariage entre personnes de même sexe. L’expansion des droits civils au Canada pour les couples de même sexe était une préoccupation majeure chez plusieurs psychologues. Pendant cette période, un énoncé de politique de la SCP affirmait notre soutien à l’idée selon laquelle les couples de même sexe avaient le droit de se marier. Cela semble un peu étrange aujourd’hui, le fait que nous soutenions évidemment cette idée, mais la Dre Blair affirme qu’il s’agissait d’un énoncé assez novateur et stimulant à l’époque.
« Au début des années 2000, la recherche démontrait que les relations entre personnes de même sexe étaient semblables aux relations entre personnes de sexes différents en ce qu’elles étaient bénéfiques pour les gens, et saines, et que l’amour, c’est l’amour. C’est sur ces éléments que s’attardaient les chercheurs. Ils essayaient d’aider les responsables des politiques à comprendre que si on exclut les gens d’une institution comme celle du mariage, cela modifie les relations qu’ils entretiennent avec leur famille, leurs amis et leurs collègues. Prenons l’exemple anodin des célébrations du temps des Fêtes dans une entreprise où les invitations incluent les conjoints. En 1999, il était loin d’être évident, pour un couple de même sexe, que le conjoint allait être inclus, et souvent, il était assez clair qu’il ne le serait pas. »
À cette époque, plusieurs estimaient qu’ils ne pouvaient pas parler de leur conjoint au travail, pas plus qu’avoir sa photo sur leur bureau. Les psychologues travaillant dans ce contexte ont été en mesure de souligner qu’au fil de temps, ces situations avaient des répercussions néfastes sur la santé mentale et le bien-être des personnes concernées. La Dre Blair poursuit ainsi : « Plusieurs recherches révélaient que les familles des personnes LGBTQ ne ‘comprenaient pas’. Et qu’elles ne comprenaient vraiment qu’au moment où elles assistaient au mariage. Les cérémonies de mariage comportent plusieurs conventions sociales qui nous indiquent quand il faut se lever, quand il faut porter un toast, quand il faut applaudir, et ainsi de suite. En intégrant les relations de même sexe à un rituel social que les gens comprenaient, on a instauré un environnement où les familles et les amis pouvaient comprendre la relation, ce qui à son tour a suscité un plus vaste soutien des cercles intimes de plusieurs individus LGBTQ, et par ricochet, une amélioration du bien-être mental au sein de toute la communauté. »
La santé mentale en a pris un coup pendant la pandémie, et ce, pour plusieurs raisons. Bre O’Handley est étudiante à la maîtrise en psychologie à l’Université de Trent et la Dre Blair est sa superviseure. Elle travaille à une thèse qui étudie le bien-être des personnes LGBTQ pendant la pandémie et la manière dont les mécanismes de soutien peuvent jouer un rôle dans cette situation.
« J’examine les trajectoires du bien-être chez les personnes LGBTQ pendant la COVID. De nombreuses études effectuées partout dans le monde ont révélé que les individus LGBTQ se portent plutôt mal pendant la pandémie. Leur santé mentale a été très affectée, ils rapportent des taux plus élevés de dépression, d’anxiété et de stress que les autres. Tout le monde vit la COVID et l’isolement social, mais il existe des facteurs supplémentaires qui pourraient avoir des répercussions chez les individus LGBTQ. Il se peut qu’ils vivent dans un milieu qui ne les soutient pas, particulièrement s’ils sont plus jeunes. Ils sont séparés des communautés solidaires, comme si vous aviez un groupe d’amis à l’école qui vous soutiennent et vous acceptent, mais que vous n’alliez plus à l’école. La pandémie diminue l’accès aux centres de ressources LGBTQ. Pendant longtemps, les personnes trans n’ont pas eu accès à leur traitement hormonal substitutif (THS) et aux chirurgies d’affirmation de genre, puisque ces services ont été jugés non essentiels au début de la pandémie, et que les problèmes liés à la chaîne d’approvisionnement ont créé des délais dans la livraison d’importants médicaments et hormones. »
Dans plusieurs pays, on a même adopté des politiques de lutte contre la COVID discriminatoires. Au Pérou, on a mis en place un règlement qui obligeait les hommes à ne quitter la maison qu’à certains jours précis et les femmes, les autres jours. Par conséquent, les individus trans et ceux qui ne s’identifiaient comme homme ni comme femme faisaient face à des situations intenables. Ils sont plusieurs à avoir été harcelés et à subir des crimes haineux alors qu’ils étaient à l’extérieur de la maison. La recherche de Bre n’aborde pas la discrimination comme telle, mais davantage le soutien qui est nécessaire à ceux qui sont la cible de cette discrimination.
« Comment favoriser la résilience dans ces circonstances, et comment les personnes LGBTQ s’en sortent-elles pendant cette pandémie? Si je me sens proche de la communauté LGBTQ, alors ça devrait atténuer certains des problèmes qui touchent la santé mentale. Mais comment établir une distinction entre cet aspect et le soutien social plus général? Est-ce que le simple fait de compter sur le soutien des gens et des membres de la famille qui vous entourent est suffisant, ou avez-vous plutôt besoin de contacts sociaux avec les membres de votre groupe de pairs pour maintenir véritablement votre résilience? La situation actuelle, avec l’avènement de la COVID, nous donne l’occasion de démêler tout cela. »
Le travail n’est jamais terminé et de nouveaux défis émergent constamment. Le mariage entre personnes du même sexe est inscrit à la législation canadienne depuis seize ans. Depuis une décennie, l’adoption par les couples de même sexe est légale dans l’ensemble des provinces et territoires du Canada. La thérapie de conversion est maintenant prohibée et plusieurs membres de la Section de l’orientation sexuelle et l’identité sexuelle se sont activement engagés dans les discussions avec les responsables des politiques pour que cela se produise. Aujourd’hui, l’identité de genre rejoint la lutte pour les droits à l’égalité des couples homosexuels et lesbiens. Comme le mentionne la Dre Blair, « on peut en savoir beaucoup sur l’orientation sexuelle et les minorités sexuelles et ne rien savoir sur l’identité de genre et les minorités de genre, et vice-versa. Les deux dimensions se sont rejointes dans une même section de la SCP, alors que l’identité de genre était moins courante et que l’intérêt était probablement plus centré sur l’orientation sexuelle à ce moment-là. Avec le temps, le genre est devenu une question tout aussi importante que l’orientation sexuelle au sein de la section. »
Tous autant que nous sommes dans la société canadienne en apprenons un peu plus sur l’orientation sexuelle et l’identité de genre, à l’instar des scientifiques qui acquièrent des connaissances sur le sujet et nous renseignent en cette matière. La Dre Hoskin cadre cela sous l’angle de la féminophobie.
« Notre capacité de détecter la féminophobie provient de l’étude de la diversité sexuelle et de genre. La féminophobie est éclairée par notre habileté à établir des distinctions entre l’identité de genre et le sexe assigné à la naissance, et l’expression de genre. Lorsque nous pouvons voir ces choses comme différentes, nous pouvons voir comment l’expression du genre entre en jeu et comment elle est régulée par la société. »
Nous faisons tous partie de cette société, et la manière dont nous régulons nos attitudes à l’égard des membres de la population LGBTQ+ joue un rôle primordial dans le maintien et l’amélioration de leur santé mentale. Il peut s’agir d’utiliser les bons pronoms pour s’adresser à quelqu’un, d’embrasser sa fille lesbienne, ou quelque chose d’aussi simple que de dire avec assurance « Je n’aime plus la bière. »

Dre Shahnaz Winer
Dre Shahnaz Winer, Carrières et professions en psychologie
L’une des deux nouvelles sections de la SCP, la Section des carrières et des professions en psychologie, est un endroit où réseauter et collaborer, destiné aux personnes qui ont un diplôme en psychologie, mais qui travaillent dans d’autres sphères que le milieu universitaire ou la pratique clinique.
Carrières et professions en psychologie
En juin 2014, l’État islamique/DAESH envahit le territoire kurde du nord de l’Irak, capturant successivement Samarra, Mosul et Tikrit. La Dre Shahnaz Winer est une jeune célibataire qui enseigne la psychologie dans une université du Moyen-Orient de la région, endroit où elle est née et que sa famille l’incite à quitter. Elle choisit donc de monter dans l’avion qui la ramènera au Canada, alors que le Kurdistan est frappé de bouleversements et de violents affrontements.
La Dre Winer se remémore affectueusement la période où elle enseignait en Irak, soulignant qu’il s’agissait des meilleurs moments de sa carrière. Elle est évidemment attristée que ce chapitre ait dû prendre fin, et surtout de la manière dont il s’est terminé. Mais cette morosité est de courte durée. Elle occupe une série d’emplois voués à une sphère qui l’a motivée pendant toute sa carrière : la mise en application de la science et du savoir en psychologie pour rehausser le quotidien de… eh bien… tout le monde! Après plusieurs emplois à l’intérieur et à l’extérieur du milieu universitaire, elle démarre sa propre entreprise. Et c’est en tant que propriétaire de cette entreprise qu’elle s’adresse l’an dernier aux étudiants, lors du salon de l’emploi de la SCP.
Les salons de l’emploi de la SCP, tenus depuis quelques années, comptent parmi les activités les plus attendues, attirant une importante participation. Au cours de ces évènements, les étudiants ont l’occasion de se familiariser avec divers postes et parcours professionnels destinés aux diplômés en psychologie, et ce, à l’extérieur de la prestation de services de santé et des milieux universitaires. Qui plus est, ils sont en mesure de rencontrer des personnes qui occupent ces postes et d’explorer toute la gamme de possibilités d’emploi qui s’offrent aux diplômés en psychologie.
Des gens comme Sophie Kenny, qui travaille en technologie des mouvements oculaires chez VPixx Technologies. Ou encore Anne-Marie Côté, de TakingITGlobal, qui coordonne des excursions virtuelles pour les étudiants habitant les communautés autochtones des régions nordiques et éloignées. Ou bien notre collègue, la directrice générale associée de la SCP, Lisa Votta-Bleeker, dont le travail à la SCP est certainement distinct des milieux universitaires ou de la pratique clinique.
Ces activités permettent aux étudiants, aux professionnels et à d’autres personnes intéressées de réseauter dans un milieu conçu pour élargir les options offertes aux diplômés en psychologie et à tous ceux qui sont attirés par un parcours professionnel moins traditionnel. Mais que se passerait-il si ces gens qui partagent une vision commune pouvaient profiter d’un réseau pendant toute l’année, plutôt que seulement quelques fois lors d’activités ponctuelles? Voilà l’idée derrière la création de la toute nouvelle Section des carrières et des professions en psychologie de la SCP.
La Dre Winer s’est alliée à la Dre Votta-Bleeker pour lancer cette section. La Dre Winer détient un doctorat en neuroscience cognitive de l’Université de Waterloo. Elle est l’une de ces personnes ayant choisi un parcours non traditionnel. L’entreprise qu’elle a créée, Vibrant Minds, est une plateforme éducative en ligne où la Dre Winer amalgame les principes de la psychologie à d’autres sujets d’intérêt. Elle crée des produits numériques qui aident les gens à planifier, à fixer et à atteindre leurs objectifs de carrière et de vie.
« Le fait que je puisse toucher un auditoire international d’étudiants par ce moyen est l’un des aspects que j’apprécie le plus. Je peux entrer en contact avec plein de gens différents, et les aider à appliquer ce que la psychologie nous enseigne et ce que la recherche universitaire a découvert. »
La Dre Winer a bien fait un séjour dans un rôle traditionnel en milieu universitaire, en tant que professeure. Elle souligne que pendant cette période, elle a constaté que les étudiants convergeaient davantage vers un type particulier de cours.
« Les parties des cours qui soulevaient l’enthousiasme des étudiants étaient celles où ils pouvaient mettre en application ce qu’ils apprenaient dans leur propre vie. Par exemple, si nous explorions la mémoire, une session entière était consacrée à l’application du savoir pour qu’ils puissent étudier plus efficacement et se souvenir plus aisément des matières liées aux examens. Alors, c’est ce genre d’application qui m’a réellement stimulée et j’estimais que cet aspect était largement absent au sein de la psychologie traditionnelle et de toutes les autres professions et disciplines. Jeter un pont entre le volet universitaire et rejoindre les gens pour transmettre cette information. »
Lorsque la Section des carrières et des professions en psychologie commencera à recruter ses membres, la plupart d'entre eux seront des personnes qui comblent ce fossé; des personnes qui appliquent la science et le savoir en psychologie à toutes les industries imaginables à travers le Canada; des personnes qui rendent le transport aérien plus sûr, les milieux de travail plus inclusifs et créent des édifices à haut rendement qui minimisent l’empreinte écologique. Ce nouvel espace de collaboration rassemblera ces personnes, dans toute leur diversité.
« Cette section s’est réellement inspirée du besoin de fournir un lieu à ceux d’entre nous qui, comme moi, avons des antécédents en psychologie, sans avoir suivi une voie traditionnelle. Je suis devenue membre de la SCP quand j’étais étudiante. Mais quand j’ai quitté le milieu universitaire, j’ai aussi quitté la SCP parce que j’estimais qu’il n’y avait plus rien pour moi. Et je me sentais en fait très seule! C’était merveilleux de pouvoir compter sur ce genre de communauté, ce soutien et les ressources qu’offre la SCP. Alors, quand on a communiqué avec moi, avec l’idée de créer une nouvelle section, destinée particulièrement aux personnes intéressées aux champs d’activité extérieurs aux domaines typiques de la psychologie, mon intérêt s’est immédiatement éveillé! »
La Section des carrières et des professions en psychologie est actuellement à l’étape où elle a été approuvée. La prochaine tâche consiste à recruter les membres fondateurs. Avec 90 nouveaux membres dès les premières semaines de recrutement, la section connaît un départ dynamique. La Dre Winer a une idée de ce que pourraient être ces premiers membres. Elle songe à une alliance diversifiée composée de professionnels établis, en début de carrière et évidemment, d’étudiants.
« Nous voulons créer un espace accueillant pour les étudiants qui explorent leurs possibilités de carrière. Ce groupe compte beaucoup pour moi parce que je sens que j’ai été très privilégiée. Quand j’effectuais mes études de doctorat, pendant la première année, toute l’information qui me parvenait, tous les ateliers et tous les séminaires et salons de l’emploi, toutes ces activités étaient axées sur les étapes à franchir pour intégrer le milieu universitaire ou encore la pratique clinique. À ce moment-là, je ne savais pas ce que je voulais faire, mais je souhaitais connaître les autres options qui m’étaient offertes.
Ma superviseure, la Dre Myra Fernandes, croyait vraiment que nous devions explorer toutes les options mises à notre disposition. Alors, dans le cadre de notre propre laboratoire, elle a créé une série de séminaires où elle invitait différents conférenciers. Par exemple, une personne ayant fait des études en psychologie qui travaillait pour l’entreprise pharmaceutique Eli Lilly est venue nous entretenir de son parcours et de son travail. Le fait d’être exposée à ces débouchés m’a inspirée et m’a transmis beaucoup plus de connaissances. Cependant, mes camarades des études supérieures ne profitaient pas de ces occasions ou de ces renseignements supplémentaires. »
Certaines des autres personnes qui ont manifesté un intérêt pour la section sont des professionnels qui souhaitent échanger entre eux, des personnes qui sont disposées à offrir du mentorat aux étudiants et des personnes qui ont choisi la voie universitaire ou clinique, mais qui ont aussi d’autres intérêts. Plusieurs font ce que de nombreux diplômés en psychologie font, comme de la recherche. Mais ils l’effectuent dans un cadre hospitalier, gouvernemental, dans le secteur privé ou encore dans de jeunes entreprises, plutôt que dans une université. Par conséquent, ils ne se sentent pas très branchés au traditionnel volet universitaire.
Comme l’évoque la Dre Winer, « bon nombre de personnes se situent dans l’entre-deux, et c’est ce qui est si formidable de ce vaste spectre. Nous accueillons toute personne, d’où elle provienne, qui souhaite se joindre à nous et entrer en contact avec ce groupe de gens qui ont une large gamme d’intérêts. »
La Dre Winer s’estime chanceuse et elle est reconnaissante d’avoir vécu ces expériences lors de ses études et d’avoir par conséquent choisi une trajectoire non traditionnelle. En plus d’être doyenne des sciences sociales, d’occuper un éventail de postes d’enseignante et de mener sa propre entreprise, elle a aussi travaillé comme conceptrice et éducatrice de programmes d’enseignement, directrice d’une école de programmation pour les jeunes, et comme animatrice et coordonnatrice du Programme mémoire et vieillissement pour un groupe de centres d’hébergement pour personnes âgées de l‘Ontario.
Ce sont ces expériences que Dre Winer souhaite partager avec les autres membres de la nouvelle section – des personnes ayant des visions communes qui ont choisi différentes trajectoires de carrière et des étudiants qui tireraient grandement profit d’être exposés à des débouchés différents qu’ils n’auraient peut-être pas découverts autrement. L’idée derrière tout cela est de concevoir un grand et long salon des carrières, qui évolue et se développe sans cesse; un salon qui crée un lieu pour les diplômés en psychologie qui pourraient autrement avoir l’impression d’être sur une île; un salon qui fonctionne, collabore et agit en réseau, non seulement 48 heures à la fois, mais 365 jours par année.

Dr Marvin McDonald

Dre Tanya Mudry

Dre Jessica Van Vliet

Dr Houyuan (Hy) Luo

Dre Janet Miller
Dr Marvin McDonald, Dre Tanya Mudry, Dre Janet Miller, Dr Houyuan (Hy) Luo, et Dre Jessica Van Vliet, Psychologie du counseling
La psychologie du counseling a de nombreuses facettes et est exercée par de nombreux praticiens différents. Nous avons parlé avec cinq d’entre eux de leur travail et de la manière dont il influence la vie quotidienne des gens.
Syd Barrett a fondé Pink Floyd en 1964, et a été la force motrice de l’album phare du groupe, The Piper at the Gates of Dawn, paru en 1967. Il n’a participé qu’à un seul autre album, A Sauceful of Secrets, avant que des problèmes de drogue et de santé mentale ne conduisent à son départ du groupe. Il s’est ensuite retiré de la vie publique, gardant obsessionnellement sa vie secrète pendant 35 ans, jusqu’à sa mort en 2006.
En insistant pour qu’il y ait cinq membres sur scène en tout temps, la Section de la psychologie du counseling pourrait bien être la Pink Floyd des disciplines de la psychologie. Étant donné qu’il s’agit d’une discipline collaborative et inclusive, je n’étais pas surpris, lorsque j’ai demandé à rencontrer la Section de la psychologie du counseling de la SCP, qu’un groupe de cinq personnes se présente sur Zoom.
Le Dr Marvin McDonald est professeur à l’Université Trinity Western, en Colombie-Britannique. Il est le Syd Barrett du groupe (en ce sens qu’il est là depuis le début), l’ancien président qui a contribué à faire de cette section ce qu’elle est aujourd’hui. Le Dr McDonald a un peu plus d’expérience que les autres et a bien sûr vu l’évolution de la discipline.
« Lorsque j’ai fait mes études de doctorat aux États-Unis dans les années 1980, le cours d’éthique était un cours optionnel! souligne-t-il. Ce n’était pas un cours obligatoire; j’évoque ce fait simplement pour vous donner un exemple très concret de la façon dont ont changé les choses. Le point positif de la transition qui s’est opérée au fil des ans est que les normes professionnelles ont suivi les preuves empiriques. Lorsque j’ai commencé mon cours sur la psychopathologie de l’enfant, les données des enquêtes communautaires sur les besoins en santé mentale n’avaient pas encore été regroupées. La question des différences entre les sexes en ce qui concerne les besoins en santé mentale était toujours débattue dans la documentation. Ce n’est qu’à la fin des années 1980 et au début des années 1990 que les données ont montré clairement que les femmes sont plus nombreuses que les hommes à demander de l’aide, et que les hommes présentent des taux plus élevés de consommation de drogue et de toxicomanie. C’est ce type de connaissances qui a fait progresser la psychologie du counseling au cours des dernières décennies et qui a une incidence considérable sur la pratique, et pas seulement sur la recherche. »
La Dre Tanya Mudry, professeure de psychologie à l’Université de Calgary et psychologue du counseling qui a quelques clients en pratique privée, est la nouvelle présidente de la section. Elle est la David Gilmour du groupe, dans la mesure où elle a remplacé le Dr McDonald – et dans le sens où elle fait avancer le groupe avec un but précis.
Pour elle, la psychologie du counseling est « un groupe assez diversifié. Nous avons tendance à travailler dans la collectivité avec les familles, les enfants et les couples. Nous travaillons souvent avec des personnes qui sont confrontées aux transitions de la vie – cela peut être des problèmes familiaux ou conjugaux – et avec des personnes qui ont des problèmes de santé mentale ou des troubles liés à l’usage de substances psychoactives. Nous avons tendance à adopter une perspective diversifiée – de nombreux psychologues privilégient une méthode particulière de thérapie, tandis que les psychologues du counseling sont plus polyvalents. Certains s’intéressent au passé et à l’enfance. Certains s’intéressent au contexte social de l’individu ou à ce qui se passe à l’intérieur du cerveau, et d’autres encore se concentrent sur les questions de justice sociale et la défense des intérêts. »
La Dre Janet Miller est la Richard Wright de l’appel Zoom (Wright était le claviériste de Pink Floyd, connu pour sa maîtrise de divers instruments et pour les rythmes et mélodies jazz syncopés qu’il apportait à la musique). La Dre Miller travaille à l’Université Mount Royal de Calgary, mais elle n’est pas professeure. Elle est conseillère d’orientation et exerce également en pratique privée à Calgary. Elle apporte un style jazz improvisé à la conversation, lorsqu’on lui demande comment la psychologie du counseling peut affecter la vie quotidienne d’une personne qui ne suit pas, elle-même, une thérapie.
« Lorsque vous arrivez à la caisse à l’épicerie, l’employé vient tout juste de sortir d’une séance de counseling, où il apprend à gérer son anxiété sociale pour pouvoir travailler avec le public et être à l’aise avec les interactions publiques. En thérapie, il aura appris à prendre conscience de son corps, à se centrer et à mettre son anxiété de côté pendant un certain temps afin de pouvoir entrer véritablement en contact avec les gens. Il a peut-être utilisé les mécanismes d’adaptation qu’il a appris, et lorsque vous êtes arrivé à la caisse pour payer votre épicerie, l’interaction entre vous deux s’est déroulée sans heurts. Votre séance de magasinage à l’épicerie a été agréable, l’employé a passé une belle journée au travail et est rentré à la maison avec de l’énergie à consacrer à sa charmante famille. »
Le percussionniste du groupe, Nick Mason, est le seul membre de Pink Floyd à figurer sur ses cinq albums. Il est devenu l’emblème du « son Pink Floyd » et a écrit certaines des plus grandes chansons du groupe. Le Nick Mason de notre quintette est le Dr Houyuan (Hy) Luo, qui incarne tout à fait la définition classique du psychologue du counseling. Il exerce en pratique privée à Toronto et est le président désigné de la Section de la psychologie du counseling. Le Dr Luo affirme que, bien que la pandémie ait rendu la prestation de services de counseling plus difficile à certains égards, plusieurs de ses clients accueillent favorablement les nouvelles méthodes de prestation.
« J’ai commencé à offrir des services de counseling complètement virtuels en mars 2020. Je travaille au centre-ville de Toronto, dans les gratte-ciel, et les bureaux ont été pendant de nombreux mois désertés par les travailleurs. Les services de counseling en ligne étaient alors plus pratiques et plus faciles pour beaucoup de gens. Avec la vaccination, les gens reviennent lentement au bureau et nous nous attendons à recommencer graduellement à offrir des services en personne en plus des services virtuels. »
Le Dr Luo souhaite élargir le domaine de la psychologie du counseling pour y inclure davantage de personnes de couleur, car il y a une véritable pénurie de psychologues capables de partager leur vécu avec leurs clients, qui peuvent provenir de milieux différents.
« Toronto, où je travaille, est une ville très diversifiée. Les clients qui veulent travailler avec un psychologue qui a la même origine ethnique qu’eux ont de la difficulté à en trouver un, même à Toronto. Nous devons vraiment aider les étudiants PANDC du premier cycle dès qu’ils entrent à l’université, pour veiller à ce qu’ils soient soutenus tout au long de leur parcours. »
La Dre Jessica Van Vliet, la Roger Waters du groupe, est également très impliquée dans les changements sociaux et la défense de la justice sociale. Roger Waters, le bassiste et l’auteur-compositeur principal de Pink Floyd, est le membre qui a fait évoluer le groupe dans une direction plus ouvertement sociale (pensez à The Wall). La Dre Van Vliet, professeure à l’Université de l’Alberta en psychologie du counseling, affirme que le plus grand changement récent observé dans le domaine de la psychologie du counseling concerne la justice sociale.
« La justice sociale a toujours été importante en psychologie du counseling, mais elle l’est aujourd’hui plus que jamais. Elle est désormais à l’avant-garde de tout ce que nous faisons. Nous avons toujours mis l’accent sur la diversité, mais aujourd’hui plus que jamais, je pense que notre discipline joue un rôle de premier plan dans le domaine du travail interculturel et avec des personnes, des questions et des méthodologies différentes. Je pense également que le leadership et la défense des intérêts sont de plus en plus valorisés et mis en avant dans notre domaine. »
Pour l’instant, le plus grand problème de la psychologie du counseling – et de pratiquement toutes les autres industries, professions et disciplines de la psychologie du monde entier – est la COVID. Elle a fait augmenter le besoin de thérapeutes capables d’aider les personnes confrontées à l’épuisement professionnel, à la dépression, au désespoir et à tous les autres problèmes de santé mentale qui sont apparus dans la foulée de la pandémie. Nous avons enregistré notre appel Zoom en octobre 2021, et les pensées de la Dre Mudry exprimées à cette époque semblent prémonitoires.
« L’un des domaines où les psychologues du counseling vont jouer un rôle déterminant est celui de la reconstruction après la COVID. J’ai récemment participé à des travaux sur l’épuisement professionnel parmi les travailleurs des soins intensifs, et je crois que les besoins seront énormes. En Alberta, en particulier, et partout au Canada, nos professionnels de la santé sont exténués. Aussi les familles et les personnes qui ont de la difficulté à travailler de la maison, le manque d’interactions sociales, nos enfants ont de la difficulté à s’adapter au va-et-vient de la maison à l’école. Dans les prochaines années, les psychologues du counseling seront très occupés. »
En quoi la psychologie du counseling aidera-t-elle particulièrement à traiter l’épuisement professionnel et tous les autres problèmes qui sont apparus? La Dre Van Vliet répond ainsi à la question :
« Une partie de ce que nous faisons est de modifier le discours que les gens entretiennent dans leur esprit. Nous aidons à transformer ce discours en le faisant passer de “Qu’est-ce qui ne va pas chez moi?” à “Qu’est-ce qui va bien chez moi?” L’accent mis sur les forces, l’aspect positif de la psychologie du counseling, constitue une énorme richesse dans notre domaine. Je pense que cela a largement contribué à la manière dont les gens se perçoivent eux-mêmes, perçoivent les autres et perçoivent le monde. »
Très peu de gens, voire personne, ne savent ce que Syd Barrett a fait pendant les 35 dernières années de sa vie. À la fin des années 1970, Roger Waters l’a aperçu dans le grand magasin Harrods de Londres. Barrett a vu Waters, a laissé tomber ses sacs et est sorti du magasin en courant. C’était la dernière fois qu’un membre de Pink Floyd voyait son fondateur. Nous savons qu’il est devenu un jardinier passionné et qu’il s’est consacré à la peinture, mais c’est à peu près tout. Nous espérons qu’il s’en est bien sorti pendant les dernières années de sa vie et qu’il a pu surmonter certains de ses problèmes avec un professionnel qui aura pu l’aider à améliorer son sort. Un professionnel, comme un psychologue du counseling peut-être?

Dre Jenna Boyd

Dr. Rachel Langevin
Dre Jenna Boyd et Dre Rachel Langevin, Section du stress traumatique
Traumatic Stress shows itself in more than just PTSD, and can be caused by more than just major single events. Dr. Jenna Boyd and Dr. Rachel Langevin are working to help those affected by trauma, and working to learn more about traumatic stress as they do.
“In the 80s and early 90s, there was nothing known about the victims of child sexual abuse. Now, there are volumes of research on the subject.”
Dr. Rachel Langevin is an assistant professor of counselling psychology at McGill University, as well as a clinical psychologist who does a bit of private practice. She is currently the Chair-Elect of the CPA’s Traumatic Stress Section. She says her PhD advisor was one of the pioneers in researching the sexual abuse of children in Quebec and Canada. At the time she decided to work on this, it was a reality that many people didn’t even recognize existed. The first step had to be acknowledging, socially, that the sexual abuse of children DID exist, and that often it happened within families. It may seem difficult to imagine now, but it took a very long time for this kind of abuse to be recognized as real in the public at large.
“In the early 80s, some researchers in the States, like David Finkelhor, started trying to really understand child sexual abuse and the specific impact it had related to other traumatic experiences. One of the first to start working on it here in Quebec was Martine Hébert, who was my PhD advisor. Her advisor had been a specialist looking at perpetrators of sexual abuse, but not victims – and Dr. Hébert was the only one looking at that side. She did her research with a lot of autonomy, because no one else had that expertise!”
Today, child sexual abuse is one of the most-studied types of child maltreatment. Research into traumatic stress has come a long way in a short time. Dr. Jenna Boyd is a psychologist at an anxiety treatment and research clinic at St. Joseph’s Healthcare Hamilton, and an assistant professor in the department of psychiatry and behavioural neuroscience at McMaster University. She is the current Chair of the CPA’s Traumatic Stress Section, and specializes in the treatment of Post-Traumatic Stress Disorder (PTSD).
“Cognitive Behavioural Therapy (CBT) is my main area of practice. A little more than 20 to 30 years ago, the main therapies that we’re using now were just emerging. From the perspective of treating PTSD, there was almost a thought that we couldn’t really treat it, but we could kind of help people cope with it. Today, we do have some really effective treatments.
Potentially traumatic experiences are pretty common. Over the course of their lives, most of us will be exposed to a traumatic event. It could be the death of someone close to us, a serious injury, sexual or intimate partner violence, or a frightening near-death experience. For some of us, it’s part of our jobs – a first responder or someone in the military could be exposed to a traumatic event more than once in a day. ‘Traumatic stress’ is what comes about as a reaction to that trauma.
It’s quite normal to have a stress-based reaction to a traumatic event or series of events. Most people who are exposed to one will have some kind of stress-response as a result. Many people will recover over time through a process of natural recovery, but others may go on to develop PTSD. This is where the symptoms related to the trauma persist over a longer period of time. Dr. Langevin says those symptoms can be multiple, complex, and varied.
“We encounter many different symptoms in this line of work. Re-experiencing symptoms, like nightmares, intrusive memories. Someone might be doing something and suddenly an image pops into their head causing distress. Every time they’re exposed to something that might resemble the trauma they endured, or something that makes them think about it, they will have a stress reaction, and anxiety will rise up. That might lead them to the second category of symptoms, which is avoidance. People start avoiding things that remind them of the trauma because it’s too stressful and uncomfortable.
The third big category of symptoms is a change in cognition, mood, and self-image. This includes things like self-blame, taking an overly large share of responsibility over what happened, feeling disconnected from others, or feeling no emotion whatsoever. And finally, there are arousal and reactivity symptoms. This is a more physiological response, and includes things like always being on your guard and looking over your shoulder, being very easily startled, difficulty sleeping, irritability, and possibly self-harm behaviours.”
When a clinical psychologist specializing in trauma sees someone who presents with a cluster of these symptoms, that persists for a month or longer after the traumatic event, and those symptoms are affecting that person’s life, that’s when they start talking about something like PTSD. At that point, it is no longer a normal reaction, and it requires attention. As Dr. Boyd says, there are now many ways that attention can be delivered.
“We now have Cognitive Processing Therapy, Prolonged Exposure Therapy, Eye Movement Desensitization and Reprocessing (EMDR) to name just a few. These treatments have had a lot of research supports behind them over the past 20 or 25 years. We now know they’re really effective for many people, and we have tools where we can say ‘let’s try this and see if we can get you to a place where you’re functioning better’. Many people can return to some of the things in their lives that have been taken away from them.”
Treatments are always improving, clinical psychologists are always innovating, and researchers are continually expanding our understanding of trauma, stress, and the interaction of the two. Dr. Langevin’s current research is looking into the intergenerational continuity of family violence, including child maltreatment and intimate partner violence.
“We know that a parent who was maltreated in their childhood is at increased risk of having a child that will also experience trauma and maltreatment – whether or not it’s at their own hands. Sometimes the mistreated parent becomes a perpetrator of abuse, and other times that doesn’t happen but the child still ends up being mistreated by someone else in the environment. There’s this continuity that we see in the data and in clinical practice, but the mechanisms that are responsible for this – the protective factors, the risk factors that are involved – are still trying to be understood. What makes one parent end up in a cycle where there is repetition of their own maltreatment history with their child, versus parents who are able to break those cycles? We’re looking to help parents who have been in this situation end the cycle, and foster resilience and positive adaptation in their children and themselves.”
Dr. Langevin is quick to point out that treating traumatic stress, and the problems that come along with it, go far beyond PTSD. She says,
“Everything can be associated with trauma, including behaviour problems, emotion regulation, depression, anxiety, bullying, difficulties with attachment and relationship. There are a host of different areas where we can see the consequences of traumatic events. PTSD is just one part of it, there’s a lot more. And we’ve come a long way in learning about it!”
 Dr Jude Mary Cénat
Dr Jude Mary CénatFévrier, c’est le Mois de l’histoire des Noirs, et la SCP met en vedette des psychologues noirs contemporains tout au long du mois. Jude Mary Cénat, Ph. D., est le directeur du Laboratoire de Recherche Vulnérabilité, Trauma, Résilience et Culture (V-TRaC) de l’Université d’Ottawa et le directeur du Centre Interdisciplinaire pour la santé des Noir.e.s.
« Quel domaine peut être plus antiraciste que la psychologie? Nous sommes là pour soutenir les êtres humains, le développement de la personne et le bien-être des individus! Il n’y a pas de domaine qui puisse aborder les questions raciales aussi bien que la psychologie. »
Jude Mary Cénat, Ph. D., se passionne pour la lutte contre le racisme en psychologie et invite ses collègues du secteur de la santé mentale à se joindre au mouvement. Le Dr Cénat est professeur agrégé à l’École de psychologie de l’Université d’Ottawa et directeur du Laboratoire de Recherche Vulnérabilité, Trauma, Résilience et Culture (V-TRaC) de la même université. Il est en outre le directeur du Centre Interdisciplinaire pour la santé des Noir.e.s.
Le laboratoire V-TRaC a trois axes. Le premier s’intéresse aux aspects familiaux, sociaux et culturels des traumatismes et de la résilience. Le deuxième axe est consacré à la santé mentale mondiale. Le laboratoire mène un projet sur différents pays d’Afrique visant à documenter les problèmes de santé mentale liés aux maladies infectieuses, comme le virus Ebola et la COVID-19. Cet axe s’intéresse également à la violence fondée sur le sexe et la santé mentale dans les Caraïbes. Le troisième axe porte sur les disparités raciales en matière de santé et de services sociaux.
« Nous menons des projets sur la santé mentale des Noirs, et nous avons réalisé la première enquête sur la santé mentale des Noirs au Canada, dans le cadre d’un projet important financé par l’Agence de la santé publique du Canada visant à documenter la santé mentale des Noirs et à créer et mettre en œuvre des programmes liés à cette question. Nous nous penchons sur la surreprésentation des enfants noirs dans les organismes de protection de la jeunesse pour essayer de comprendre tous les facteurs qui sont à l’origine de cette situation et proposer des solutions. » En décembre 2021, le laboratoire V-TRaC a dévoilé 13 recommandations visant à réduire la surreprésentation des enfants noirs dans le système de protection de la jeunesse.
L’implication des services de protection de la jeunesse dans la vie de l’enfant est le principal facteur permettant de prédire si un jeune se retrouvera sans abri et si d’autres problèmes, comme la pauvreté et une faible scolarisation, apparaîtront plus tard. La surreprésentation des jeunes noirs dans ce système fait qu’ils subissent ces effets plus souvent que les autres groupes, ce qui entraîne un cycle perpétuel.
« Le premier facteur est que les professionnels des organismes de protection de la jeunesse ne sont pas formés pour prendre en compte les aspects culturels des familles noires. Nous réunissons beaucoup de groupes de discussion avec les intervenants, et l’une des choses qu’ils soulignent est qu’ils ne sont pas assez formés pour aborder les questions culturelles. Nous avons mené une étude qui a montré que, en 2020, plus de 48 % des programmes de travail social offerts dans les universités et les collèges de l’Ontario ne comptaient pas de cours obligatoire sur la culture. Il existe aussi des facteurs systémiques, comme la pauvreté dans les communautés noires, et la discrimination raciale que beaucoup d’enfants et de jeunes noirs ont vécue dans le système de protection de la jeunesse.
Mais ce n’est pas seulement le système de protection de la jeunesse comme tel qui est en cause, c’est aussi la société en général. Dans les écoles, par exemple, les enseignants sont plus susceptibles d’appeler les services de protection de la jeunesse en cas de problème avec un enfant noir qu’avec un enfant blanc. La société canadienne est une société “sans préjugés raciaux”; nous disons : “Je ne vois pas la couleur de votre peau, je vois vos problèmes et j’essaie de les régler”. Lorsqu’un enfant a des problèmes à l’école, on peut appeler ses parents pour le régler. Mais souvent, s’il s’agit d’un enfant blanc, l’enseignant aborde le problème directement avec les parents, alors qu’il risque d’appeler la protection de la jeunesse directement s’il s’agit d’un enfant noir. »
L’idée d’une société “sans préjugés raciaux” équivaut à celle d’une société “non raciste”. C’est un moyen passif d’aborder la race, où le fait de ne pas rire d’une blague raciste ou de ne pas se faire complice d’un recrutement discriminatoire est suffisant. Mais cela ne va pas assez loin pour corriger les inégalités raciales existantes. Le Dr Cénat espère que nous pourrons dépasser les notions de “non-racisme” et d’“absence de préjugés raciaux” pour devenir une société véritablement antiraciste au Canada.
« Comme l’a dit Ikram Kendi, il n’y a pas de “racistes” et de “non-racistes”. Il y a des “racistes” et des “antiracistes”. Parce que si vous êtes simplement “non raciste”, vous vous autorisez à observer des personnes se montrer racistes et vous vous rassurez en vous disant que vous n’êtes pas l’une d’elles. Vous ne posez pas de geste qui puisse contrer le racisme. Et ce n’est qu’en agissant contre le racisme que nous créerons une société antiraciste. »
C’est dans cet esprit que le Dr Cénat et son équipe ont créé le cours Comment fournir des soins de santé mentale antiracistes, qui donne droit à des crédits de formation continue approuvés par la SCP. Si les professionnels de la santé mentale, les universitaires des établissements d’enseignement supérieur et les dirigeants de tout le pays adoptent les principes de l’antiracisme, nous pourrons véritablement commencer à nous approcher d’un Canada inclusif où tout le monde se sent le bienvenu, où la discrimination et le profilage ne sont pas tolérés, où nous sommes tous sur un pied d’égalité et où nous avons tous les mêmes chances.
Le Dr Cénat a publié un article dans The Lancet dans lequel il explique que les soins de santé mentale antiracistes sont des soins proactifs, dans le sens où ils abordent les questions raciales sans attendre que les clients ou les patients les soulèvent. Les soins antiracistes vont au-delà des soins interculturels. Ils intègrent à la fois des aspects culturels et des éléments qui permettent de tenir compte des dommages causés par la discrimination raciale, le profilage racial et les microagressions raciales. C’est une façon de créer des espaces dans une société exempte de racisme.
« Le problème de la notion de société “sans préjugés raciaux” est le suivant. Prenons l’exemple d’un homme noir qui se présente dans votre bureau; vous vous dites : “Je ne vois pas la couleur de sa peau, je l’évalue et je lui offre des soins sans voir la couleur de sa peau.” Mais le fait est qu’il se peut que la couleur de sa peau fasse partie de son problème. Cet homme noir est peut-être déprimé, et l’un des facteurs qui expliquent sa dépression est la discrimination raciale qu’il vit au travail. Ou parce que ses enfants sont victimes de discrimination et qu’il n’a pas assez de pouvoir pour défendre ses enfants, ce qui lui rappelle qu’enfant, il a subi la même discrimination de la part des autres enfants et des enseignants. Lorsque vous vous dites que vous ne voyez pas la couleur de sa peau, vous ne traitez pas son problème, car la couleur de sa peau fait partie intégrante de son problème. »
Il ne s’agit pas seulement d’une situation hypothétique à laquelle un professionnel de la santé mentale pourrait être confronté, mais d’une situation étayée par des données. L’équipe du Dr Cénat a publié un article qui montre que les Canadiens noirs âgés de 15 à 40 ans qui connaissent de hauts niveaux de discrimination raciale sont trente-six fois plus susceptibles de présenter des symptômes graves de dépression que ceux qui connaissent des niveaux inférieurs de discrimination.
« Si vous recevez un membre de la communauté noire présentant des symptômes dépressifs, vous devez l’interroger sur la discrimination raciale et les traumatismes qu’il a subis ou qu’il subit. C’est ce que notre cours Comment fournir des soins de santé mentale antiracistes apprend aux cliniciens : ils sont amenés à s’interroger sur eux-mêmes pour se connaître davantage et pour prendre conscience de leurs propres préjugés, puis à évaluer les problèmes raciaux et les traumatismes dans leurs activités cliniques. Enfin, ils apprennent comment fournir des soins antiracistes aux enfants, aux adolescents et aux familles. »
Du 26 au 28 octobre de cette année, le Dr Cénat et son équipe tiendront la première conférence consacrée exclusivement à la santé mentale des Noirs, qui s’intitule « Black Mental Health in Canada: Overcoming Obstacles, Bridging the Gap ». Comme le dit le Dr Cénat, aucune profession ne dispose de meilleurs outils pour lutter contre le racisme que la psychologie. Et il est déterminé à mettre autant d’outils qu’il le peut dans cette boîte à outils.

Dr Andrew Hyounsoo Kim

Dr Nassim Tabri
Dr Andrew Hyounsoo Kim et Dr Nassim Tabri, Psychologie de la dépendance
La psychologie de la toxicomanie couvre de nombreux domaines, de la consommation de substances psychoactives jusqu’aux jeux vidéo. Le Mois de la psychologie met en vedette aujourd’hui le Dr Andrew Hyounsoo Kim et le Dr Nassim Tabri, qui parlent du travail qu’ils font dans le domaine des dépendances et de la lutte contre la stigmatisation qui entoure le sujet.
« Je n’ai jamais eu de client qui, à la question “Qu’est-ce qui vous amène ici?”, me réponde “Je voulais devenir accro, alors me voilà.” Ça ne m’est jamais arrivé. »
Andrew Hyounsoo Kim est professeur adjoint au département de psychologie de l’Université Ryerson et président de la Section de la psychologie des toxicomanies de la SCP. Psychologue clinicien (exercice autonome provisoire), le Dr Kim a fait sa résidence au Programme de traitement de la toxicomanie et des troubles concomitants du Royal. Il souligne que personne ne commence à consommer de la drogue ou de l’alcool ou à adopter un comportement donné avec une intensité telle que son fonctionnement en sera perturbé.
Presque tout le monde a déjà consommé de l’alcool et de la drogue. Rares sont les Canadiens qui n’ont jamais parié ni joué à un jeu vidéo en ligne. Certaines personnes finissent par s’adonner à ces activités de manière excessive ou à se livrer à ce genre de comportements plus souvent et plus longtemps que d’autres. Mais très peu de personnes développent une dépendance. Nous faisons tous le choix d’essayer certaines choses et nous pouvons choisir de continuer à les faire dans une certaine mesure – mais personne ne choisit de devenir dépendant.
La toxicomanie est l’un des problèmes de santé mentale les plus stigmatisés. Dans le but de remédier à cette situation et de susciter une plus grande compréhension de la part du public, un réel changement s’est opéré au cours de la dernière décennie pour abandonner le langage stigmatisant qui lui est associé. Les chercheurs et les cliniciens de ce domaine n’utilisent plus les mots « addiction » ou « abus », mais plutôt le terme « usage de substances psychoactives ».
« Nous n’utilisons plus le mot “drogué”, dit le Dr Kim. Nous disons plutôt “une personne qui souffre d’une dépendance”. Nous n’utilisons pas le mot “héroïnomane ou junkie”, et même l’expression “être clean” ne fait plus partie de notre vocabulaire car ces mots ont plutôt une connotation négative. »
En eux-mêmes, les mots « addiction, dépendance ou toxicomanie » sont largement utilisés – et mal utilisés – dans la société en général. Nous avons tendance à les utiliser pour décrire toute activité à laquelle les gens s’adonnent pendant une longue période de temps.
« Pensez à toutes les publicités qui disent par exemple : “Cette émission de télévision est vraiment addictive” ou “Je suis accro à ce jeu”. Les gens utilisent abondamment ces termes sans vraiment savoir ce qu’ils signifient. La dépendance a une signification très précise qui est beaucoup plus nuancée qu’une simple activité à laquelle une personne s’adonne pendant de longues périodes. Elle englobe non seulement le biologique (le cerveau), mais aussi le comportement, les émotions, les pensées et les conséquences qui en découlent. »
Outre le mauvais usage du mot, il subsiste de nombreuses idées fausses sur la dépendance elle-même, à savoir qu’il s’agit d’un échec moral ou d’un choix personnel, et que devenir dépendant est le signe d’un manque de caractère.
« Au tout début, lorsque vous commencez à vous livrer à un comportement de dépendance, c’est vous qui décidez de le faire, poursuit le Dr Kim. Mais avec le temps, le problème devient beaucoup plus complexe qu’un simple manque de volonté. Des changements se produisent dans le cerveau et dans le contexte émotionnel et psychosocial de la personne, et l’on passe d’un choix à une compulsion, c’est-à-dire que la personne s’y adonne même si cela ne lui procure plus de plaisir. S’il suffisait, pour arrêter, de se dire “arrête de consommer”, les psychologues cliniciens qui se spécialisent en toxicomanie ne travailleraient pas. Les dépendances, c’est beaucoup plus complexe que le simple fait d’arrêter. »
Le Dr Nassim Tabri est professeur adjoint de psychologie à l’Université Carleton. Ses recherches portent sur la toxicomanie et la santé mentale, en particulier les facteurs transdiagnostiques qui sont présents dans une gamme de comportements problématiques, comme le jeu et les troubles de l’alimentation.
« Pour comprendre ce qu’est une dépendance et comment une personne peut développer éventuellement une dépendance, il faut voir les choses de la manière suivante. Vous buvez de l’alcool pour la première fois, pour essayer, ou vous prenez un jeu vidéo et commencez à jouer. Cela ne signifie pas nécessairement que, parce que vous faites une chose qui a un fort potentiel addictif, vous développerez une dépendance. La dépendance s’installera si vous répétez le comportement même si vous n’en retirez plus de plaisir. Alors, vous devez répéter le comportement pour mieux fonctionner, et non plus pour le plaisir, et le fait de ne pas consommer ou vous adonner au comportement en question vous rend malheureux. »
La psychologie de la toxicomanie est une vaste discipline qui touche à pratiquement tous les aspects de nos vies connectées. Les publicités, les jeux, les téléphones, etc. sont conçus selon les principes de la science de la toxicomanie. Mais il existe un seuil défini de comportements qui constituent une dépendance. Ce n’est pas un seuil précis, car il peut être un peu différent chez chaque personne qui souffre de dépendance, mais le degré auquel l’activité, la consommation de la substance ou le comportement affectent la vie de cette personne est très élevé.
« La “dépendance” est un terme qui doit être réservé à une pathologie grave, souligne le Dr Tabri. Les publicités ou les jeux d’argent nous incitent, d’une certaine manière, à adopter un certain comportement. Le fait qu’une personne développe ou non une dépendance dépend en fait de son profil de risque (facteurs de risque biopsychosociaux). Le fait de se livrer modérément à ces activités, même si l’on est influencé, ne mérite pas le terme de “dépendance” ».
Je n’ai pas touché à mon téléphone depuis environ deux heures. Je le prends et je fais défiler les notifications – CBS Sports veut m’informer que les Broncos de Denver ont embauché le coordonnateur offensif de Green Bay, Nathaniel Hackett, comme nouvel entraîneur. L’appli Flipp voudrait que je voie les nouvelles aubaines disponibles cette semaine chez Loblaws. Mon petit jeu mobile veut que je sache qu’il m’a accordé des vies supplémentaires, Pharmaprix est très inquiète que je rate ma chance d’obtenir 10 000 points Optimum en dépensant 40 $ à son magasin et Twitter m’a envoyé huit notifications à propos de huit nouveaux abonnés que j’ai attirés aujourd’hui.
Bien que ces notifications ne concernent pas nécessairement le travail des psychologues spécialisés en toxicomanie, elles sont toutes influencées par la psychologie de la toxicomanie. Toutes sont conçues pour provoquer une réponse de ma part, pour me faire interagir avec l’appli, la boutique d’applis ou le contenu de manière à maximiser le temps que je passe sur mon téléphone et, par extension, à minimiser le temps que je passe à faire d’autres choses, vraisemblablement plus productives, mais moins intéressantes sur le moment. Bien que ces choses soient créées et étayées par la psychologie de la toxicomanie, le fait qu’elles m’influencent ne signifie pas que je suis « dépendant »; il y a un certain seuil à partir duquel on peut utiliser ce terme et si je ne me prive pas de sommeil, ne saute pas les repas et ne quitte pas le travail quatre heures plus tôt pour jouer à Words With Friends, je n’ai probablement pas dépassé ce seuil.
« Certains principes utilisés augmentent la probabilité de comportements addictifs sur les téléphones intelligents, ajoute le Dr Kim. Il s’agit de choses qui augmentent le temps passé sur l’appareil. Pour rendre l’appli plus attrayante, envoyer des notifications. Par exemple, avec les jeux vidéo en particulier, les tableaux des meneurs ou des messages comme “Voici une offre spéciale aujourd’hui – pour seulement 1,99 $, vous pouvez obtenir des vies supplémentaires”. Le jeu est un autre exemple : des connaissances et des principes psychologiques ont été utilisés pour développer les machines à sous, de sorte que les gens restent plus longtemps devant la machine. »
Bien que les principes psychologiques de la dépendance puissent être, et ont été utilisés pour engendrer des comportements addictifs qui entraînent parfois une dépendance, les psychologues qui se spécialisent dans ce domaine ont tendance à travailler sous l’angle opposé. Ils se concentrent sur la prévention et le traitement. Ils ont créé les Directives de consommation d’alcool à faible risque, les Lignes directrices sur les habitudes de jeu à moindre risque et les Recommandations pour l’usage du cannabis à moindre risque, les théories derrière le certificat Smart Serve Ontario et des initiatives de réduction des méfaits comme les sites d’injection supervisée. C’est là que les connaissances en psychologie sont directement appliquées pour réduire les méfaits que peuvent causer certaines de ces substances ou certains de ces comportements.
« La psychologie est l’étude scientifique de l’esprit et des comportements humains, ajoute le Dr Kim. En ce sens, la psychologie de la toxicomanie utilise des méthodes psychologiques scientifiquement fondées pour mieux comprendre pourquoi certaines personnes consomment des substances psychoactives jusqu’à en devenir dépendantes, et d’autres, non. La psychologie essaie aussi de mieux comprendre les effets des substances et d’autres comportements addictifs sur le cerveau, et, ce que je trouve le plus intéressant, les façons de mettre au point des interventions, des traitements et des mesures de prévention de manière à réduire les préjudices et la souffrance subis par les personnes qui vivent ou ont vécu avec une dépendance. »
Lorsque nous entendons le mot « dépendance », nous avons tendance à l’associer à des substances plutôt qu’à des comportements. La cigarette, l’alcool, la crise des opiacés nous viennent à l’esprit lorsqu’il est question de dépendance, mais ces comportements addictifs sont-ils similaires, par exemple, à ceux associés aux jeux d’argent ou aux jeux vidéo? Selon le Dr Tabri, ce n’est pas nécessairement le cas.
« Une des choses sur lesquelles nous nous concentrons est le cerveau. Je donne un cours complet sur le système dopaminergique de la récompense. Il me semble que le grand public comprend que les comportements addictifs ont une influence similaire sur le cerveau car ils détournent le système dopaminergique de la récompense. Cela signifie que la personne qui a développé une dépendance ne s’adonne plus aux activités qui ont du sens pour elle et qui la font se sentir bien, mais qu’elle fait la seule et unique chose qui la fait se sentir vraiment bien, au détriment de toutes les autres choses qui composent sa vie.
Mais toutes les dépendances sont-elles identiques dans le cerveau? Pas nécessairement. À une certaine époque, la théorie la plus répandue était que tout est dû à la dopamine, qui est à la base de tout. Cela a commencé par des recherches sur les rats dans les années 1950, et l’histoire s’est imposée parce qu’elle était attrayante. L’idée que la dopamine peut expliquer toutes sortes de comportements addictifs s’est développée. Mais quand on regarde les publications, on constate que la dopamine est très utile pour expliquer les comportements liés à l’alcool, par exemple, ou à la nicotine dans une certaine mesure. Mais elle ne l’est pas tellement, lorsqu’il s’agit de la dépendance au cannabis, par exemple. La dopamine n’explique pas tout, et les choses sont plus nuancées et complexes. Elle joue probablement un rôle, mais elle n’est pas la clé de tout dans le cerveau. »
La science de la toxicomanie et la psychologie qui la sous-tend évoluent constamment à mesure que nous apprenons des choses nouvelles et que nous abordons celles-ci d’une manière différente. Tout comme nous avons modifié la terminologie utilisée relative à la santé mentale, à la consommation de substances et aux personnes qui souffrent de dépendance, nous avons mis en place de nombreux programmes, campagnes et initiatives pour réduire les risques et la stigmatisation. À travers tout cela, plusieurs choses restent vraies, la plus importante étant que « personne ne choisit la toxicomanie ».

Juanita Mureika

Dawn Hanson
Juanita Mureika et Dawn Hanson, Psychologues et la retraite
Même après la retraite, de nombreux psychologues poursuivent leurs activités professionnelles. Le Mois de la psychologie met en vedette aujourd’hui Juanita Mureika et Dawn Hanson, qui nous parlent de leur travail dans ce domaine.
Beaucoup de psychologues se lancent dans la profession dans un but de défense des intérêts – ceux de leurs clients, de l’avancement de la recherche en psychologie, de la mobilisation des connaissances et de la déstigmatisation entourant la santé mentale. Que la défense des intérêts soit une ambition explicite ou implicite, c’est un élan universel chez les personnes qui consacrent leur vie à aider les autres.
Cette motivation à être au service des autres ne prend pas fin une fois la carrière terminée. Prendre sa retraite après avoir exercé la profession de psychologue ne signifie pas nécessairement cesser de militer pour les grandes causes. En fait, la fin de la vie active pourrait donner plus de temps pour relever ce genre de défis, voire découvrir de nouvelles causes à défendre.
C’est le cas de Juanita Mureika et de Dawn Hanson, coprésidentes de la Section des psychologues et la retraite de la SCP. Juanita a pris sa retraite en 2011 après avoir exercé comme psychologue scolaire, mais elle demeure active dans l’arène politique du Nouveau-Brunswick. Elle a passé une grande partie de l’année 2021 à faire pression contre le projet de loi-35, dans le cadre duquel le gouvernement du Nouveau-Brunswick a l’intention de retirer les évaluations des élèves des mains des psychologues scolaires et de permettre aux enseignants d’effectuer ces évaluations à la place.
Dawn a pris récemment sa retraite de la présidence de la Manitoba Association of School Psychologists, mais elle reste active et impliquée dans le projet de loi-64 qui vient d’être proposé. Le projet de loi ferait disparaître tous les conseils scolaires, afin de centraliser l’administration scolaire à Winnipeg. « À la Manitoba Association of School Psychologists, nous sommes toujours à l’affût de tout ce qui pourrait avoir une incidence sur les services psychologiques au Manitoba, particulièrement en ce qui concerne les enfants d’âge scolaire et les familles, dit Dawn. Je ne peux pas imaginer – à la retraite ou non – ne pas être impliquée dans ces dossiers et ces questions brûlantes. Nous avons été très impliqués dans la création d’un nouvel ordre des psychologues au Manitoba. Nos psychologues scolaires ne faisaient pas encore partie de l’organisme de réglementation avant aujourd’hui. Ainsi, avec l’arrivée d’un nouvel ordre, nous travaillons pour que les psychologues scolaires puissent y être représentés, tâche que nous avons entreprise il y a plusieurs années. »
Pour Juanita, Dawn et la Section des psychologues et la retraite dans son ensemble, la représentation des intérêts ne cesse pas avec la retraite. Et la retraite elle-même ouvre en fait d’autres domaines où la défense des intérêts peut être très utile. Partout au Canada, les psychologues à la retraite sont très préoccupés par les règlements en vigueur dans leur province respective en ce qui concerne la durée de conservation des dossiers. Dans une province, les dossiers doivent être conservés en lieu sûr pendant 15 ans – mais si le client est un enfant d’âge scolaire, le dossier doit être conservé en lieu sûr pendant 15 ans après l’année où l’enfant atteint l’âge de la majorité. Selon Dawn, « il s’agit d’une tâche très lourde pour les psychologues qui doivent trouver un moyen de garder et de conserver ces dossiers en lieu sûr, parfois pendant des décennies! Juanita et moi avons exercé la plupart de nos activités dans le cadre scolaire, de sorte que, après avoir pris notre retraite, ce problème ne nous concernait plus. L’école doit garder ces dossiers en lieu sûr, conformément à ce qui est exigé par l’organisme de réglementation ou par la province. »
Ni Dawn ni Juanita ne sont concernées par ce problème, mais elles défendent néanmoins la cause. La Section des psychologues et la retraite a envoyé un sondage à tous les autres organismes de réglementation du Canada, y compris ceux des territoires, afin de déterminer quels étaient les problèmes en matière de confidentialité, de conservation des dossiers, de consentement éclairé, etc. Au moment d’écrire ces lignes, les réponses de ces groupes continuent de nous parvenir – lentement. Jusqu’à présent, la seule chose qui est claire, c’est que les règlements, les politiques et les pratiques régissant la conservation des dossiers varient énormément d’une province à l’autre.
Imaginez que vous fermez votre cabinet et que vous prenez votre retraite. En plus de détenir un grand nombre de fichiers électroniques, vous avez également des mètres et des mètres de dossiers papier que vous devez garder en sécurité pendant encore 15 ans. Il est probablement peu pratique et peu sûr, voire illégal, de garder tous ces documents dans votre sous-sol. Allez-vous payer pendant 15 ans un garde-meuble, à même votre revenu de retraite? Quelles sont vos options et comment pouvez-vous procéder? Et par qui seront assurés ces dossiers, selon l’endroit où ils sont stockés?
Dawn et Juanita sont sur l’affaire. Cela peut prendre un certain temps avant d’obtenir des réponses, car à chaque étape du processus, une nouvelle difficulté surgit. Comme le dit Juanita, « Une autre chose dont nous devons dorénavant tenir compte est le fait que de nombreuses provinces exigent un testament professionnel aux personnes qui projettent de prendre leur retraite. La conservation des dossiers deviendra donc le problème de quelqu’un d’autre si vous prenez votre retraite ou si vous mourez. Or ce ne sont pas toutes les provinces qui l’exigent. Il y a toujours quelque chose de nouveau. Mais pensez aux dossiers médicaux ou dentaires; ils sont conservés pendant très longtemps et il devrait en être de même des dossiers psychologiques. C’est simplement un peu trop lourd pour les gens qui se demandent « combien de temps cela va-t-il durer? »
Juanita, Dawn et les membres de la Section des psychologues et la retraite sont peut-être à la retraite, mais ils sont de plus en plus impliqués dans la représentation des intérêts. Au sein des conseils scolaires, des politiques provinciales et de la section elle-même, il existe de multiples possibilités d’influencer les systèmes afin de les améliorer. Juanita et Dawn vont continuer de faire avancer les questions importantes – pour les retraités, pour les psychologues scolaires et pour tous les autres.
 Dre Eleanor Gittens
Dre Eleanor GittensLa Dre Gittens est professeure au Georgian College et enseigne au programme universitaire de formation policière. Elle aide les étudiants à confronter leurs préjugés avant d’obtenir leur diplôme et devenir policiers, en les emmenant à la Barbade!
Le plat national de la Barbade est le poisson volant frit au coucou (une bouillie à base de farine de maïs et de gombos) agrémenté d’une sauce épicée. La cuisine barbadienne est aussi appelée cuisine Bajan, et les beignets de poisson et les gourmandises frites typiques de la Barbabe ont influencé la cuisine du monde entier. Comme c’est le cas de la nourriture, la Barbade elle-même a eu un impact culturel hors norme par rapport à sa petite taille. La Barbade a une population de moins de 300 000 habitants.
La ville de Barrie, en Ontario, fait, à elle seule, la moitié de la taille de la Barbade. Elle compte un peu plus de 150 000 habitants, et l’un d’eux est la Dre Eleanor Gittens. Native de la Barbade, la Dre Gittens est professeure au Georgian College et enseigne au programme universitaire de formation policière. Les principaux cours qu’elle donne actuellement portent sur les méthodes de recherche, la cybercriminalité, les problèmes de santé mentale dans les services policiers et les mouvements sociaux contemporains.
« Ce qui me passionne, c’est la recherche, dit-elle. J’aime faire des recherches avec les services de police, surtout lorsqu’ils ont une question ou une préoccupation, mais ne savent pas comment s’y prendre pour obtenir les preuves ou les données à partir de ce qu’ils ont déjà. Je peux les aider à y répondre. »
L’une de ces questions concernait les appels provenant d’établissements locaux de soins de longue durée de la ville d’Orillia. Le service de police de la PPO de la région a communiqué avec la Dre Gittens parce qu’il était préoccupé par le fait qu’il recevait de ces établissements trop d’appels de service qui ne nécessitaient pas la présence de la police. Étant donné que toute possibilité de recherche peut être intégrée à l’enseignement, la Dre Gittens et quelques-uns de ses étudiants ont créé une équipe de recherche chargée d’examiner la question. L’équipe a examiné tous les appels effectués pendant une certaine période pour déterminer ce que les preuves montraient.
Elle a découvert que la police provinciale de l’Ontario avait raison : de 60 % à 70 % des appels provenant d’établissements de soins de longue durée ne nécessitaient pas la présence de la police. Dans beaucoup de cas, les résidents appelaient le 9-1-1 directement de leur chambre pour une raison futile comme avoir égaré leur télécommande. La Dre Gittens et ses étudiants ont présenté leurs conclusions à la fois au service de police et aux établissements de soins de longue durée (et lors du congrès de la SCP de cette année-là).
Leurs recommandations ont conduit à des changements tant au service de police que dans les centres de soins eux-mêmes. Les organismes de soins de longue durée ont modifié la façon dont leurs résidents accèdent aux téléphones et les processus par lesquels le personnel communique avec les services d’urgence. La police a modifié ses politiques en ne se contentant pas de déterminer quand intervenir, mais en modifiant la manière dont elle répond aux appels de ces établissements afin de s’assurer que l’intervention est adaptée à la situation.
La plupart des étudiants qui suivent les cours de la Dre Gittens deviennent des policiers. Ces dernières années, l’accent a été mis sur les préjugés implicites dans le travail de la police et sur les conséquences de ces préjugés, en particulier pour les communautés de couleur.
« Souvent, les policiers se font une idée de l’identité des criminels et de l’endroit où se déroule l’activité criminelle en fonction de leurs propres préjugés et des sentiments qu’ils ont développés au fil du temps en travaillant sur le terrain, explique-t-elle. L’une des choses que nous essayons de faire lorsqu’il s’agit des droits de la personne et de la justice sociale est de briser certains de ces préjugés afin que les gens puissent commencer à voir les choses pour ce qu’elles sont plutôt que de les voir à travers le prisme de leurs préjugés. »
Alors, comment déconstruire certains de ces préjugés avant que ces étudiants obtiennent leur diplôme et deviennent des policiers un peu partout au Canada, au service de communautés très différentes ayant des besoins et des problèmes systémiques très différents? Même si, selon elle, il est impossible de se débarrasser entièrement des préjugés, la Dre Gittens s’est dit que le meilleur moyen de pousser les futurs policiers dans cette direction serait d’emmener ses étudiants – qui sont majoritairement blancs – à un endroit où ils constitueraient la minorité, loin de leur environnement social habituel. Les étudiants se trouvent à Orillia, une ville très peu diversifiée. La Dre Gittens est la seule professeure noire du Georgian College. Alors, où emmener ces étudiants?
À la Barbade. Elle les emmène à la Barbade.
« La Barbade est à 95 % noire. Les étudiants peuvent explorer la nourriture et la culture et visiter les postes de police et la prison. [Oui, il n’y a qu’une seule prison à la Barbade.] Nous avons déjà fait une visite de la Cour suprême, où les étudiants ont pu assister à une audience. Lors de ces voyages, ils ont l’occasion de voir certaines des subtilités du rôle de la culture dans le comportement des gens, la façon dont ils pensent et la façon dont ils sont perçus. Ce n’est qu’une expérience pour eux, mais je pense que c’est mieux que pas d’expérience du tout. »
Il est difficile de comprendre l’impact de la culture et de la tradition tant que l’on n’est pas en plein milieu d’une culture qui n’est pas la sienne. Bien sûr, les étudiants adorent l’expérience.
« Non seulement tous les étudiants aiment leur expérience, mais c’est aussi ce que recherchent les services de police de nos jours. Lorsque que je dois fournir des références pour un étudiant qui se destine au métier de policier, l’une des questions que posent les employeurs est : « que savez-vous de son point de vue sur la diversité? » Lorsqu’il s’agit d’un étudiant que j’ai emmené en voyage, je peux parler de la façon dont il s’est comporté pendant sa visite. Qu’est-ce qui le distingue des autres étudiants? Comment a-t-il accueilli, par exemple, la nourriture? Il y a des gens qui refusent de goûter à de nouveaux plats, simplement parce qu’ils ne les connaissent pas ou ne les comprennent pas! La peur est une émotion qui peut vraiment paralyser les gens. »
La Dre Gittens aime aider ses étudiants à améliorer leurs compétences culturelles dans sa vie professionnelle, et aime voyager dans sa vie personnelle. Malheureusement, les voyages avec ses étudiants et ses voyages personnels ont dû être mis en veilleuse durant la pandémie. Un jour, tout cela sera à nouveau possible. En attendant, la Dre Gittens se réjouit à l’idée d’amener d’autres étudiants à la Barbade pour qu’ils découvrent la culture, l’atmosphère et, bien sûr, la cuisine. Petit conseil pour quiconque y ira : « Goûtez au poisson! ».

Dr Jonathan Wilbiks
Dr Jonathan Wilbiks , Cerveau et sciences cognitive
Les chercheurs du domaine des sciences du cerveau et des sciences cognitives s’intéressent à la façon dont le cerveau fonctionne et à la façon dont il perçoit et trie les stimuli externes. La rubrique du Mois de la psychologie d’aujourd’hui se penche sur ce sujet, avec le Dr Jonathan Wilbiks, qui nous parle de son travail – et de Snoop Dogg et Angela Hewitt.
« With so much drama in the LBC
It's kinda hard bein’ Snoop D-O-double-G. »
Vous assistez au spectacle de la mi-temps du Super Bowl. Dr. Dre, Eminem, Mary J. Blige, Snoop Dogg et Kendrick Lamar sont sur scène, et vous vibrez au rythme de la musique. Sur le grand écran, vous pouvez voir Snoop faire du rap, et la musique frappe fort dans vos oreilles. La foule qui vous entoure hurle et applaudit. Vous êtes perdu dans le moment présent et vous ne vous demandez pas vraiment « comment savoir que tout cela est réel? Qu’est-ce qui me dit que c’est bien la voix de Snoop Dogg que j’entends? Comment puis-je être certain que le bruit de la foule autour de moi est fait par les autres supporters? » Vous n’avez pas à répondre à ces questions parce que votre cerveau rassemble les informations pour vous. Les lèvres de Snoop bougent sur le grand écran et semblent correspondre aux paroles que vous entendez. Le bruit de la foule vient de derrière, de devant et tout autour de vous, et votre cerveau fait le tri pour vous, de sorte que vous savez qu’il y a des milliers de personnes qui crient de milliers de façons, et vous n’avez pas besoin de prêter attention à une quelconque voix dans la foule.
La façon dont le cerveau exécute ces tâches est le domaine des sciences cognitives, qui est la spécialité de chercheurs comme le Dr Jonathan Wilbiks, professeur agrégé en psychologie à l’Université du Nouveau-Brunswick, Saint John. Le Dr Wilbiks est le président de la Section cerveau et science cognitive de la SCP et il étudie l’intégration audiovisuelle et le traitement multisensoriel – comment le cerveau reçoit diverses informations sensorielles et décide implicitement si ces choses proviennent de la même source. (Vos lèvres bougent et j’entends chanter – c’est probablement votre voix que j’entends.)
Dernièrement, certains des travaux du Dr Wilbiks ont porté sur la perception et les aptitudes musicales. Son équipe de chercheurs a constaté que les musiciens obtiennent de bien meilleurs résultats que les non-musiciens dans des tâches où le son et les images sont en concordance, c’est-à-dire que l’image correspond au son et se produit au même moment. Mais les musiciens sont moins performants que les non-musiciens lorsque le son et les images ne sont pas en concordance. Les personnes qui ont une formation en musique, plus que celles qui n’en ont pas, utilisent l’information auditive pour donner un sens à ce qu’elles voient.
Lorsque Angela Hewitt s’assoit devant son piano et place devant elle la partition des Variations Goldberg, tout est parfaitement logique. Chaque note qui figure sur la feuille représente une note qu’elle doit jouer au piano, et les deux choses concordent : elle a fait cela toute sa vie et c’est plus facile pour elle que pour… eh bien, tout le monde. Mais si, au lieu de la partition, on lui avait présenté une tablette cunéiforme représentant une notation musicale, il se peut qu’elle soit complètement perdue. En fait, quelqu’un qui ne sait pas du tout lire la musique pourrait être capable d’accomplir cette tâche mieux qu’elle. (Les plus anciennes notations musicales jamais découvertes datent d’environ 1 400 avant J.-C. et sont inscrites sur une tablette cunéiforme trouvée dans l’actuel Irak.)
Dans les années qui ont suivi la Seconde Guerre mondiale, le béhaviorisme était le courant le plus populaire en psychologie. Les chercheurs béhavioristes plaçaient un rat dans une boîte et l’exposaient à un stimulus, puis ils mesuraient les réactions du rat et la façon dont elles évoluent dans le temps avec une exposition répétée au même stimulus. Ils ne portaient pas vraiment attention à ce qui se passait réellement dans le cerveau. Selon le Dr Wilbiks, c’est parce que la science repose sur des faits observables, et qu’à l’époque, il n’y avait aucun moyen d’observer ce qui se passait dans le cerveau. Cela a commencé à changer à la fin des années 1960, lorsque le psychologue germano-américain Ulric Neisser a publié Cognitive Psychology, où il avançait que les processus mentaux d’un individu peuvent, en fait, être mesurés et analysés.
« Les chercheurs en sciences cognitives qui ont fait leur apparition dans les années 1960 ont dit “il se produit plein de choses dans le cerveau”, explique le Dr Wilbiks. Bien sûr, nous ne savons pas exactement ce qui s’y produit, mais il se produit quelque chose, et ce serait une erreur de ne pas en tenir compte. Ils ont donc essayé d’émettre des hypothèses sur ce qui se produit et de mesurer cela à l’aide d’observations secondaires. La tâche de temps de réaction en est un exemple simple. Je vous donne un bouton et vous demande d’appuyer dessus chaque fois qu’une lumière clignote sur l’écran devant vous. Les gens sont généralement assez rapides – leur temps de réaction est d’environ 200 millisecondes. Mais si je vous donne deux boutons et que je vous demande d’appuyer sur le bouton de gauche lorsque la lumière verte clignote et sur le bouton droit lorsque la lumière rouge clignote, il faudra plus de temps – peut-être 400 millisecondes. Nous ne pouvons pas voir ce qui se produit dans le cerveau, mais nous pouvons supposer que si la première tâche prend 200 millisecondes et la deuxième, 400 millisecondes, cela signifie très clairement que le traitement des informations dans le cerveau prend du temps. »
Avec le temps, bien sûr, les choses ont dépassé le stade de la lumière rouge et de la lumière verte lorsque les expériences sont devenues plus sophistiquées et que la technologie nous a permis de voir réellement ce qui se passe dans notre tête. Nous sommes capables de voir la tension électrique créée par les impulsions neurales dans le cerveau. Les appareils d’IRMf (imagerie par résonance magnétique fonctionnelle) permettent aux scientifiques d’observer et de mesurer les variations de l’oxygénation du sang qui indiquent des niveaux différents d’activité cérébrale. Nous pouvons désormais dire quelles zones du cerveau sont actives, quand elles le sont, et ensuite corréler cela avec les informations comportementales que nous recueillons.
Le domaine des sciences du cerveau et des sciences cognitives est vaste et a une incidence qui se manifeste dans notre vie quotidienne, et ce, de multiples façons. En ce moment, il se passe plein de choses autour de vous. Supposons que vous êtes assis sur une chaise. Il y a d’autres meubles dans la pièce, peut-être des décorations sur les murs. Il y a de la circulation à l’extérieur, le lave-vaisselle fonctionne peut-être en arrière-plan et quelqu’un regarde la télévision dans une autre pièce, tout cela pendant que vous lisez cet article. Il vous est impossible de prêter attention à tout en même temps, c’est pourquoi votre cerveau filtre tous ces stimuli externes avant même que vous ne les perceviez, pour éviter que vous ne soyez submergé.
Votre cerveau décide, pour vous, de ce qui est important. La circulation que vous entendez dehors? Vous pouvez l’ignorer parce qu’elle ne constitue pas une menace. Comme le dit le Dr Wilbiks, il est rare qu’une voiture percute une maison; ainsi, lorsque vous êtes assis dans votre maison, vous n’avez pas à faire attention au bruit des voitures. Mais lorsque vous marchez dans la rue, le bruit des voitures est très important pour vous – si vous entendez le bruit d’une voiture qui accélère au moment où vous vous engagez sur un passage pour piétons, vous devriez à l’évidence tourner la tête vers ce bruit pour voir ce qui se passe, car il existe maintenant une réelle possibilité de danger.
Le cerveau crée des raccourcis pour obtenir une efficacité maximale avec un minimum d’effort, et ce phénomène est appelé « économie cognitive ». Parce que nous utilisons de tels raccourcis, et que nous ne traitons que les informations les plus pertinentes et ne retenons que les indices les plus importants, nous sommes plus sensibles aux « incitations douces ». Ce sont de petites choses que les sciences cognitives ont créées pour nous inciter à nous comporter d’une certaine manière. Comme conduire plus prudemment. Le Dr Wilbiks en donne un exemple :
« Vous êtes sur la route au volant de votre voiture et vous savez que vous roulez dans une petite rue résidentielle. Vous savez que la limite de vitesse est de 40 km/h, vous conduisez donc plutôt lentement, et vous êtes attentif. Vous guettez s’il y a des enfants qui courent dans la rue, un chien en liberté, un ballon de basketball qui roule vers la route. Si vous roulez sur l’autoroute, vous portez attention à beaucoup d’autres choses, mais vous ne cherchez pas un ballon de basketball égaré. Nous pouvons utiliser la compréhension cognitive et les incitations douces dans une situation où, par exemple, les gens ont tendance à rouler trop vite dans une rue résidentielle. Nous pouvons faire des choses pour les faire ralentir. Vous verrez parfois de petits îlots, surmontés d’un arbre ou d’autre chose, qui rendent la route un peu plus étroite. Ces îlots ne gênent pas la circulation, mais le commun des mortels ne se sentirait pas à l’aise de passer dans cet espace étroit à une vitesse supérieure à 40 km/h. »
La seule chose sur laquelle mon cerveau se concentre, que je sois dans ma voiture ou en train de travailler sur mon ordinateur, c’est la musique. Partout où il y a de la musique, que ce soit en fond sonore ou dans le garage de mon voisin au bout de la rue, je ne peux pas l’ignorer. Le Dr Wilbiks dit que l’un des cours qu’il préfère donner est le cours de psychologie de la musique, car il englobe de nombreux aspects de la psychologie en général, et pas seulement des sciences cognitives.
« Je fais généralement peur aux étudiants lors des premiers cours, parce que nous commençons par la physique. La physique du son et des ondes sonores, et leur fonctionnement. Ensuite, nous abordons la façon dont les vibrations pénètrent dans l’oreille, comment elles se traduisent dans le cerveau et comment on les perçoit. Puis nous passons à la psychologie du développement – comment développer nos aptitudes musicales, le parallèle étroit entre développement musical et développement linguistique. Nous parlons de thérapie – il se fait des travaux très intéressants qui utilisent la musique (thérapie d’intonation mélodique) pour aider les personnes qui ont subi un accident vasculaire cérébral à retrouver certaines capacités linguistiques. »
Nous avons tous deux hémisphères dans notre cerveau, et il y a une zone dans l’hémisphère droit où nous traitons la musique. Il y a une région dans l’hémisphère gauche qui reproduit presque exactement la partie musicale, et c’est là que nous traitons le langage. Lorsque les personnes qui ont subi un accident vasculaire cérébral chantent les mots qu’elles essaient de prononcer, elles peuvent, avec le temps, entraîner l’autre hémisphère de leur cerveau pour qu’il traite à nouveau le langage. À la longue, elles pourraient retrouver jusqu’à 70 % à 80 % de leur capacité de parole. Les personnes atteintes de démence sont souvent capables de créer un lien avec la musique qu’elles ne peuvent pas établir avec le langage, car la musique peut déclencher des souvenirs qui seraient autrement inaccessibles.
Vous avez peut-être vu le mème qui circule et qui dit « my ability to remember song lyrics from the 80s far exceeds my ability to remember why I walked into the kitchen » (ma capacité à me souvenir des paroles de chansons des années 1980 dépasse de loin ma capacité à me rappeler pourquoi je suis en ce moment dans la cuisine) ». Cela pourrait bien être vrai, car la musique de notre jeunesse reste un puissant déclencheur de souvenirs. C’est pourquoi les groupes de soutien aux personnes atteintes de démence chantent souvent ensemble des chansons de leur jeunesse – des chansons des Beatles et des Beach Boys et des chansons folkloriques traditionnelles du pays où elles ont grandi. Dans quelques années, les choses seront peut-être un peu différentes – en 2054, ces groupes de soutien pourraient chanter « Gin et Juice » de Snoop Dogg. Les chansons de rap produiront-elles le même genre de souvenirs et amélioreront-elles les capacités linguistiques de la même façon? Seul le temps le dira, mais lorsque nous aurons la réponse à cette question, elle nous sera fournie par des psychologues spécialisés en psychologie cognitive et d’autres spécialistes du domaine.

Dre Gilla Shapiro
Dre Gilla Shapiro, Psychologie de la santé et médecine du comportement
La psychologie de la santé et la médecine comportementale couvrent beaucoup de domaines, qu’il s’agisse d’encourager les personnes atteintes de diabète à prendre leur insuline ou d’inciter les gens à adopter des habitudes alimentaires plus saines. Le Mois de la psychologie met en vedette aujourd’hui la Dre Gilla Shapiro, qui parle du travail qu’elle fait dans le domaine du cancer et de la vaccination.
Psychologie de la santé et médecine du comportement
« Nous savons que le taux de vaccination varie selon le vaccin. Même avant la COVID-19, certains vaccins, comme le vaccin ROR (vaccin contre la rougeole, les oreillons et la rubéole), étaient beaucoup plus administrés que le vaccin contre la grippe. Il existe également des différences entre les vaccins destinés aux enfants et aux adolescents. C’est le cas du vaccin contre le VPH [papillome humain], qui est administré dans les écoles aux adolescents. »
Les psychologues de la santé et les scientifiques du comportement possèdent une expertise qui s’étend à une grande variété de spécialités et de disciplines. Plusieurs d’entre eux sont également des psychologues cliniciens agréés, autorisés à fournir des services et des traitements psychologiques. Les cliniciens spécialisés en psychologie de la santé aident les gens à surmonter leurs problèmes médicaux, leurs maladies et leurs maladies chroniques. Les spécialistes du comportement étudient tout cela, surtout lorsqu’il s’agit de comportements de prévention et de comportements qui peuvent avoir une incidence sur l’évolution d’un diagnostic médical. Qu’est-ce qui aide une personne atteinte d’une maladie cardiaque à suivre un régime alimentaire strict? Qu’est-ce qui influence la constance avec laquelle un diabétique administre son insuline? Et – point très important ces derniers temps – quels facteurs influencent le consentement et la volonté d’une personne à se faire vacciner?
Imaginez que vous venez tout juste de recevoir un diagnostic de cancer. Des centaines de questions surgissent probablement dans votre esprit et encore plus de craintes vous assaillent soudainement. D’autres facteurs peuvent aussi ajouter à ce stress, comme la possibilité de devenir infertile, la perte de revenu possible ou la nécessité de faire garder les enfants pendant le traitement. Il se peut également que vous soyez désormais entouré de toute une série de nouveaux médecins et spécialistes que vous n’aviez jamais rencontrés auparavant – oncologues, infirmières en oncologie, intervenants-pivots, consultants en génétique. Cela fait beaucoup de choses à gérer, outre le fait d’avoir à accepter le diagnostic lui-même.
L’une des personnes qui pourrait vous aider à traverser cette période difficile est un psychologue, comme la Dre Gilla Shapiro, au Princess Margaret Cancer Centre de Toronto. La Dre Shapiro est une psychologue clinicienne spécialisée en psychologie de la santé et une psycho-oncologue (une spécialiste du cancer). Elle travaille avec des personnes qui ont reçu un diagnostic de cancer, avec celles qui suivent un traitement et avec les personnes qui reçoivent des soins de fin de vie.
« De nombreuses personnes éprouvent une détresse élevée [liée au cancer et à son traitement]. Il est donc très important de disposer d’une équipe de traitement spécialisée pour les soutenir, ainsi que leurs proches. »
Une partie de l’aide offerte prend la forme de thérapies de soutien, et une autre partie est liée à la prise de décision. Si une personne atteinte d’un cancer doit prendre la décision de commencer ou non un traitement de chimiothérapie, compte tenu des effets dévastateurs de ce traitement sur l’organisme et du pourcentage de chances qu’il a de fonctionner, le fait d’en parler peut beaucoup aider. La décision de participer ou non à un essai clinique peut être un choix très difficile à faire pour une personne atteinte d’un cancer. Un psychologue, comme la Dre Shapiro, appréhende cela de plusieurs façons :
« Les gens ont besoin de soutien de différentes manières et ont des inquiétudes différentes, qui peuvent être d’ordre social, pratique, psychologique ou émotionnel. Certains se demanderont comment aborder le cancer avec leurs enfants. D’autres auront besoin de soutien pour traiter leurs symptômes comme la douleur, l’insomnie, l’anxiété ou la dépression. Certains types de cancer sont associés à une prédisposition génétique. Ainsi, si un test génétique est effectué, certaines personnes se demanderont à qui elles devraient le dire, et comment le dire. »
Au Princess Margaret Centre, une équipe travaille à l’élaboration d’interventions fondées sur des données probantes pour réduire la détresse et améliorer les conditions de vie des patients atteints de cancer. Par exemple, une intervention appelée « thérapie CALM » (Managing Cancer And Living Meaningfully) est conçue pour aider les patients à s’adapter à la vie à un stade avancé du cancer. Elle s’inspire de théories en psychologie et en santé mentale – théorie relationnelle, théorie de l’attachement et théorie existentielle – l’objectif étant d’aborder une gamme de problèmes de manière individualisée. La prise en charge des symptômes, les changements dans la relation du patient avec lui-même et avec ses proches, le sens de la vie et la finalité de l’existence, les espoirs et les préoccupations relatifs à l’avenir sont autant de facteurs pris en compte dans la thérapie CALM et sont tous vécus différemment par chaque personne qui reçoit un diagnostic de cancer en phase terminale.
Si la Dre Shapiro a décidé de travailler au Princess Margaret Cancer Centre, c’est en partie parce son superviseur, le Dr Gary Rodin, et Sarah Hales, une collège de ce dernier, est la personne qui a élaboré la thérapie CALM. Le Dr Rodin et sa collègue, la Dre Madeline Li, ont également fait des travaux intéressants pour comprendre les facteurs qui influencent les individus lorsqu’ils ont à prendre des décisions difficiles en lien avec leur santé. L’aide médicale à mourir, ou AMM, apparue très récemment, est une décision importante dans le domaine de la cancérologie. La Dre Shapiro voulait apporter à ce travail la dimension de l’équité en santé et l’optique des politiques en matière de santé. Mais ce n’est pas là que la Dre Shapiro a commencé ses travaux en psycho-oncologie et en sciences du comportement; elle a commencé à travailler en psycho-oncologie dans le domaine de la prévention du cancer et de la vaccination. Elle s’intéressait notamment aux vaccins, comme le vaccin contre le VPH, et à la façon de prévenir les virus qui causent le cancer du col de l’utérus et d’autres cancers en aidant les personnes à faire des choix comportementaux, comme se faire vacciner.
Moins de deux ans avant que la COVID-19 ne soit qualifiée de pandémie par l’Organisation mondiale de la santé (OMS), la Dre Shapiro a fait son doctorat sur l’hésitation à l’égard du vaccin contre le virus du papillome humain (VPH) chez les parents canadiens. Avec ses collègues de l’Université McGill, elle a mis au point des échelles pour mesurer les attitudes à l’égard des vaccins et a mené des recherches pour comprendre les facteurs comportementaux et sociaux de la vaccination dans la population canadienne.
En 2019, elle a commencé à travailler avec l’OMS à l’élaboration d’outils de vaccination infantile systématique et à mesurer les facteurs comportementaux et sociaux de la vaccination à l’échelle mondiale. Lorsque la pandémie a frappé, ce travail a ensuite permis de comprendre l’acceptation des vaccins par les adultes et leur intention de se faire vacciner contre la COVID, lorsque le vaccin serait offert.
Pendant la pandémie de COVID-19, la Dre Shapiro faisait partie du groupe de travail sur les sciences du comportement et la lutte contre la COVID-19 de l’Ontario; de concert avec ses collègues du groupe de travail (dont plusieurs sont également des membres de la Section de psychologie de la santé et de médecine comportementale de la SCP), elle a publié en octobre un document intitulé « Behavioural Science-Informed Strategies for Increasing COVID-19 Vaccine Uptake in Children and Youth » [LIEN].
Tout en étudiant les facteurs comportementaux et sociaux qui ont une incidence sur l’acceptation des vaccins contre la COVID-19, elle a également commencé à s’intéresser à un effet domino de la pandémie, à savoir les vaccinations systématiques manquées ou retardées. La Dre Shapiro et ses collègues de l’OMS et d’autres pays viennent de terminer une étude sur l’omission des vaccins à administrer dans le cadre de la vaccination systématique des enfants dans 26 pays pendant la pandémie [LIEN - COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: An observational survey].
Imaginez que vous ayez reçu un diagnostic de cancer, que vous ayez été opérée et ayez subi une radiothérapie, et que vous soyez maintenant sortie de tout cela avec un bilan de santé (relativement) positif. Un psychologue clinicien de la santé vous a peut-être aidé tout au long du processus, mais maintenant une autre menace existentielle, hors de votre contrôle, apparaît : une pandémie mondiale. Étant immunodéprimée, votre santé dépend de la vaccination de votre entourage contre le virus. Ce n’est pas une situation facile, mais il est rassurant de savoir que des psychologues de la santé et des scientifiques du comportement comme la Dre Shapiro y sont attentifs.

Ann Marie Beals

Dre Natalie Kivell

Ramy Barhouhe
Ann Marie Beals, Dre Natalie Kivell, et Ramy Barhouhe, Psychologie communautaire
La psychologie communautaire concerne davantage l’aspect « communautaire » que l’aspect « psychologique » et est très impliquée dans les questions de justice sociale. Le Mois de la psychologie met en vedette aujourd’hui Ann Marie Beals, la Dre Natalie Kivell et Ramy Barhouhe, qui nous parlent de leur travail dans ce domaine.
« Les personnes impliquées dans la transformation sociale au sein de leur collectivité – organisateurs communautaires, responsables des mouvements populaires – s’appuient sur des théories aussi rigoureuses sur le fonctionnement du changement que celles que l’on trouve dans le monde universitaire. »
La Dre Natalie Kivell est professeure adjointe au programme de psychologie communautaire de l’Université Wilfrid Laurier. « Il y a très peu de programmes de psychologie communautaire dans les universités canadiennes, dit-elle, et les personnes qui travaillent dans le domaine tendent à être beaucoup plus impliquées dans le volet “communautaire” que dans le volet “psychologique” de leur travail. »
Ann Marie Beals est l’une de ces personnes. Ann Marie est une étudiante de deuxième cycle au programme de psychologie communautaire de l’Université Wilfrid Laurier. Elle est Micmaque – de descendance afro-néo-écossaise et micmaque – et elle s’intéresse à l’effacement des communautés métisses afro-autochtones, hier et aujourd’hui, à la vérité et la réconciliation et à l’actuelle marginalisation des nations autochtones et des communautés noires du Canada.
Ramy Barhouhe, un autre étudiant de Natalie, est originaire du Liban et vivait aux États-Unis avant de venir à l’Université Wilfrid Laurier pour étudier au programme de doctorat en psychologie communautaire. Dans le cadre de ses études, il s’intéresse au colonialisme et à la colonisation. Il cherche à savoir, d’une part, comment les structures coloniales ont façonné le développement de systèmes communautaires entiers en Amérique du Nord et en Asie du Sud-Ouest, et d’autre part, comment cela oriente la façon dont les gens perçoivent, ressentent et expérimentent le monde sur le plan du temps, de l’espace, de la moralité, du pouvoir, de l’éducation, de la santé, de la justice, de la politique, de l’économie et plus encore.
Ramy, Ann Marie et Natalie sont venus à la psychologie communautaire par des chemins très différents, mais ils ont tous des vues similaires dans la mesure où ils placent tous la « communauté » avant la « psychologie ». Ils sont tous les trois très investis dans le démantèlement des systèmes actuels et très conscients qu’ils travaillent eux-mêmes dans certains de ces systèmes. Ramy étudie les moyens d’opérer la décolonisation dans le milieu universitaire, lui-même un vestige structurel des pratiques coloniales. Ann Marie est membre de la SCP et est la trésorière de la Section de la psychologie communautaire de la SCP, deux institutions qui sont façonnées par l’héritage du colonialisme. Natalie est professeure de psychologie, un domaine d’étude qui a longtemps été complice non seulement du colonialisme, mais aussi de la marginalisation des populations minoritaires.
Selon Ramy, « le monde universitaire est tellement imbriqué dans le système capitaliste néolibéral qu’il est très difficile de l’en détacher. L’écart de pouvoir entre les personnes qui contrôlent le flux de connaissances et celles qui ne le contrôlent pas est trop grand. Prenons l’exemple d’un universitaire qui reçoit une subvention pour faire des recherches, qui fait appel ensuite à une communauté pour obtenir des informations de celle-ci. Mais il n’a pas à obtenir l’approbation de cette communauté par la suite en ce qui concerne la diffusion et la mobilisation des connaissances. Il obtient le mérite, la reconnaissance et le financement, mais la communauté elle-même n’en retire rien. Elle ne fait qu’appuyer et aider l’université. Il s’agit donc d’un problème lié à la structure du colonialisme au sein de l’université dont nous devons encore parler et que nous devons surmonter.
Nous en parlons beaucoup dans notre programme et nous reconnaissons que nous faisons également partie du problème. Si nous effectuons cette recherche, nous ne sommes pas pour autant dégagés de la structure et de l’impact qu’elle a sur la communauté; nous faisons toujours partie du problème. Nous essayons de trouver une façon de reconcevoir cela, et cela exige une certaine dose de respect et d’humilité envers la communauté dans laquelle nous travaillons. Il faut s’assurer qu’elle obtient sa juste part et le respect qui lui est dû, et même des fonds, qui lui serviront à répondre à ses besoins. C’est là que la transformation s’impose : comment utiliser les ressources qui font malheureusement partie d’un système corrompu pour en faire bénéficier ces communautés? Et comment utiliser leurs connaissances comme étant les leurs, et non comme étant les miennes, simplement parce que j’ai fait une enquête dans la collectivité. »
Ann Marie considère la situation actuelle, influencée par la pandémie de COVID-19, comme une fenêtre ouverte sur le travail qui doit être fait. « La pandémie a révélé à quel point les politiques et les pratiques d’austérité néolibérale ont affecté nos systèmes de soins de santé et comment les travailleurs précaires touchant le salaire minimum ou occupant des emplois peu rémunérés – principalement des femmes noires, des personnes racisées, des nouveaux arrivants et des Autochtones – sont touchés de manière disproportionnée par le manque de compassion, de soins et de filets de sécurité adéquats, qui ont été démantelés par les gouvernements néolibéraux.
À titre d’exemple, l’actuel gouvernement de l’Ontario, dans le contexte d’un régime capitaliste, a adopté une loi limitant les augmentations de salaire à 1 % pour les travailleurs du secteur public comme les travailleurs de la santé, car l’inflation dépasse les 4 % [4,1 % en août 2021]. Dans notre programme de psychologie communautaire, nous comptons des étudiants et des chercheurs universitaires issus et résidents de communautés directement touchées par les pratiques néolibérales et coloniales, comme celle-ci, qui continuent à creuser les écarts en matière de soins de santé et de stabilité économique. En même temps, les droits fondamentaux de la personne, comme le logement, l’éducation, l’eau potable et la qualité de vie ne sont pas seulement bafoués, ils sont délibérément ignorés. En tant qu’étudiante chercheuse, j’examine, avec d’autres psychologues communautaires critiques, l’intersection entre les structures de pouvoir, comme la suprématie blanche, le colonialisme, le néolibéralisme et le patriarcat, et les êtres humains et la Terre mère à partir d’une infinité d’identités interconnectées.
Nous examinons ces structures de pouvoir, au travers du contrôle des ressources situées sur les terres autochtones volées, du racisme anti-Noirs et des politiques colonisatrices. Et j’entends par là les personnes qui soutiennent et maintiennent ces structures de pouvoir. Parfois, nous parlons des structures de pouvoir de manière abstraite ou théorique, mais nous devons être conscients du fait que les gens soutiennent et maintiennent ces structures. Ils essaient de dicter notre mode de vie et oppriment systématiquement toute personne qui ne correspond pas à la conception de ce qu’est un “Canadien”, à savoir un homme blanc cisgenre hétérosexuel et non handicapé. Pour moi, cela revient toujours à démanteler les structures de pouvoir qui oppriment les gens dans ma communauté. »
Il existe plusieurs mots qu’Ann Marie, Ramy et Natalie utilisent assez souvent : intersection, démantèlement, néolibéral, colonialisme. Un autre mot qu’ils utilisent tous, peut-être encore plus souvent, est celui de « collaboration ». Ramy parle de collaboration avec les communautés, de sorte que le travail qui y est effectué ne vise pas à extraire, mais plutôt à améliorer les connaissances, la santé et la réussite de cette communauté. Ann Marie parle de collaboration, dans le sens où le mérite du travail accompli n’est pas seulement l’objectif final, mais est contraire au processus d’autodétermination des collectivités. Natalie parle de dizaines d’autres organismes communautaires, militants locaux et disciplines scientifiques avec lesquels elle travaille pour faire avancer les innombrables causes de la justice sociale. En fait, le tout premier mot qu’elle utilise pour décrire la psychologie communautaire est « interdisciplinaire ».
« La psychologie communautaire est une science sociale interdisciplinaire, axée sur les valeurs et sur l’action et engagée dans la communauté. Elle s’intéresse à la justice sociale à l’intersection de la justice raciale, climatique, migratoire, sexuelle, carcérale ainsi que la justice pour les personnes handicapées. Nous travaillons à l’intersection des questions complexes de justice sociale qui se touchent de manière interconnectée. La psychologie communautaire est guidée par un ensemble de théories. Nous abordons ces questions sociales complexes à partir de lieux de prévention, de la théorie écologique, de perspectives critiques et de perspectives de décolonisation. Nous cherchons à situer les relations entre les individus, les communautés et les sociétés. Lorsque nos communautés sont justes et équitables, les personnes qui les habitent sont en meilleure santé. La psychologie communautaire a donc comme objectif de trouver des moyens de reconstruire, reconcevoir et créer collectivement des systèmes scolaires, des systèmes de santé, des systèmes pénitentiaires équitables, etc. ».
Puisque la psychologie communautaire s’attaque à un aussi vaste éventail de systèmes et de structures, le travail des psychologues communautaires transcende de nombreuses frontières et touche à d’autres aspects de la psychologie – justice pénale, environnement, éducation, etc. Bien qu’ils soient peu nombreux, leur collaboration avec les disciplines, les sciences, les groupes communautaires et les organisations militantes leur permet d’avoir un impact considérable.

Dre Milica Miočević

Dr Rob Cribbie
Dre Milica Miočević et Dr Rob Cribbie, Méthodes quantitatives
Méthodes quantitatives est une science qui fonctionne avec presque toutes les branches de la psychologie. Tous les chercheurs utilisent des méthodes différentes pour analyser les données, mais tous les chercheurs analysent les données. Dans le cadre du Mois de la psychologie d’aujourd’hui, le Dr Milica Miočević et le Dr Rob Cribbie discutent du travail qu’ils font pour rendre la collecte et l’analyse des données plus faciles, plus cohérentes et plus précises.
Dans le vaste domaine de la psychologie, les méthodes quantitatives, c’est comme la radio étudiante indé de l’université. Celle qui faisait jouer U2 et R.E.M. dans les années 1980 avant que « Sunday Bloody Sunday » et « Man on the Moon » jouent partout. Celle qui a « découvert » les Red Hot Chili Peppers au début des années 1990 avant Blood Sugar Sex Magic et les Grammys. Ou qui, il n’y a pas longtemps, a révélé les Black Eyed Peas avant l’arrivée de Fergie et leur succès commercial.
Les méthodes quantitatives, c’est l’ado avec un piercing dans le nez et une chemise à carreaux qui s’intéressait à la modélisation par équation structurelle, aux statistiques bayésiennes ou à la modélisation linéaire hiérarchique avant que ce soit branché. Celui qui a passé des mois dans sa chambre, à éplucher le catalogue, à apprendre toutes les facettes de cette méthode statistique, avant de l’abandonner et de l’envoyer dans le monde pour qu’elle soit utilisée par les chercheurs en psychologie. La plupart de ces méthodes ont été étudiées en profondeur par un très petit groupe de psychologues spécialisés en méthodes quantitatives à une certaine époque, mais sont aujourd’hui largement utilisées à la grandeur de la discipline.
Elles sont également, d’une certaine façon, le Rick Rubin de la psychologie. Vous savez comment les Red Hot Chili Peppers ont connu le succès avec Blood Sugar Sex Magic? C’est grâce au producteur Rick Rubin. Reign, le chef-d’œuvre de Slayer, 21, d’Adèle, Licensed to Ill, qui a fait connaître les Beastie Boys? Rick Rubin. Et pour les chercheurs en psychologie qui font un travail poussé – que ce soit sur la dépression, la confiance en la vaccination ou l’ESPT chez les couples de militaires –, le producteur qui travaille en coulisses pour assurer la rigueur scientifique, ce sont les méthodes quantitatives. Les psychologues spécialisés en méthodes quantitatives aident ces chercheurs à élaborer leurs études afin de déterminer la meilleure façon de recueillir les données, de tenir compte des éventuels accrocs et de définir la taille de l’échantillon nécessaire pour détecter les effets pertinents.
Le Dr Rob Cribbie est le président de la Section des méthodes quantitatives de la SCP et un psychologue spécialisé en méthodes quantitatives au département de psychologie de l’Université York.
« Les méthodes quantitatives s’intéressent aux méthodes de recherche et à l’analyse de données. Les personnes qui travaillent dans le domaine des méthodes quantitatives font tout, qu’il s’agisse de conseils sur la taille des échantillons, les plans de recherche et l’analyse des données, ou de la recherche de méthodes nouvelles ou améliorées d’analyse de données. Nous étudions également les aspects psychométriques des outils que nous utilisons et leur efficacité. », dit-il.
À quoi ressemble ce genre de travail au quotidien? Que fait exactement un psychologue spécialisé en méthodes quantitatives? La Dre Milica Miočević est la secrétaire-trésorière de la Section des méthodes quantitatives de la SCP et une psychologue spécialisée en méthodes quantitatives au département de psychologie de l’Université McGill. Elle donne un exemple de son travail :
« J’ai récemment publié un article avec un coauteur spécialisé en biostatistique sur la puissance statistique avant la répartition. Nous essayions de trouver un moyen d’utiliser les données historiques d’une étude liée à une étude en cours, mais réalisée à l’aide d’un échantillon provenant d’une population légèrement différente. Nous cherchions des façons de quantifier les différences entre les participants à l’étude précédente et les participants à l’étude en cours, et nous avons évalué si l’utilisation de notre méthode avec les données de l’étude précédente pouvait améliorer les inférences de l’étude en cours. L’article que nous avons publié permettra aux chercheurs en psychologie de
s’appuyer sur des données historiques pour améliorer les inférences statistiques des nouvelles études de recherche sans exiger des tailles d’échantillon excessivement grandes ».
Le champ lui-même est, d’une certaine manière, assez nouveau. La Section des méthodes quantitatives de la SCP célèbre son dixième anniversaire cette année, et la discipline, bien que largement reconnue aujourd’hui, était bien moins connue il y a 10 ou 20 ans.
« Je me souviens quand je menais des entretiens d’embauche, autour de l’année 2000, la plupart des personnes interviewées me demandaient « Dans quel domaine de la psychologie êtes-vous? » Et je répondais « les méthodes quantitatives », et elles disaient « Non, je veux dire, est-ce la dépression, la psychologie clinique, la psychologie culturelle, qu’étudiez-vous au juste? » Et je disais « Eh bien… les méthodes quantitatives ». Elles ne voyaient pas cela comme une discipline. Il y a eu un véritable changement depuis. Il est maintenant totalement courant de dire ‘Je suis chercheur en psychologie quantitative’. Le domaine des méthodes quantitatives est si vaste aujourd’hui, et nous utilisons tellement d’outils qu’il nous faut vraiment des gens qui se spécialisent dans les différentes méthodes », explique le Dr Cribbie.
La croissance de ce domaine a entraîné une évolution des méthodes d’analyse et d’interprétation des données par les psychologues. L’avènement de logiciels comme R et d’autres logiciels ont ouvert un monde de possibilités qui étaient beaucoup plus laborieuses, voire inaccessibles, il y a 20 ou 25 ans. Et ce monde est en constante évolution. Lorsqu’une nouvelle méthode devient populaire et se répand dans le monde de la psychologie, les psychologues spécialistes des méthodes quantitatives sont déjà passés à autre chose.
« Nous passons par des périodes où nous voyons ce qui est intéressant et ce qui doit être développé davantage. Quand je faisais mes études supérieures, les méthodes bayésiennes commençaient à faire parler d’elles. Aujourd’hui, il semble que ce soit l’apprentissage automatique, et nous attendons de voir ce qui viendra ensuite. J’ai l’impression que d’année en année, nous ajoutons quelque chose de nouveau à la boîte à outils des méthodes quantitatives en psychologie. Parfois, les approches nouvelles proviennent des statistiques, et parfois, d’autres domaines, comme l’économie. J’ai observé beaucoup de changements en 10 ans! », ajoute la Dre Miočević.
Vous connaissez les excellentes chansons de Taylor Swift, Dido, Alicia Keys ou Imagine Dragons? Celles avec un rapper invité? Ce rapper invité, c’est Kendrick Lamar. Les méthodes quantitatives sont, d’une certaine manière, le Kendrick Lamar de la psychologie, même si elles n’auront probablement jamais la même reconnaissance en solo que celle qu’il a obtenue lorsqu’il a remporté le prix Pulitzer. Elles collaborent avec n’importe qui, dans n’importe quelle discipline, à n’importe quel moment, à tel point qu’au bout d’un moment, on remarque à peine leur présence. Chaque facette de la psychologie, chaque discipline, se nourrit des derniers outils d’analyse de données, des méthodes et pratiques de recherche les plus à jour et de la rigueur scientifique que fournissent les méthodes quantitatives.
Pour le Dr Cribbie, « les méthodes quantitatives englobent tous les domaines de la discipline. Ainsi, si vous survoliez chaque section de la SCP, vous découvririez que la Section des méthodes quantitatives joue un rôle dans chacune d’elles. C’est formidable que cette section permette aux personnes intéressées de discuter de méthodes nouvelles et différentes, et de la façon dont les gens les appliquent. »
C’est pour cette raison que le Mois de la psychologie de 2022 commence par la Section des méthodes quantitatives – c’est la seule section qui alimente toutes les autres sections. Le Dr Cribbie, la Dre Miočević et leurs collègues sont les enfants cool du quartier, qui se donnaient à fond dans cette méthode de recherche bien avant que vous n’en entendiez parler. Vous pouvez suivre la Section des méthodes quantitatives sur Twitter, avec le mot-clic @cpa_qm, sur son site Web https://canadianquantpsych.wordpress.com/ ou par l’entremise de son bulletin https://cpa.ca/fr/sections/quantitativemethods/newsletter/. Vous pourrez ainsi, vous aussi, être un enfant cool, qui sait tout avant tout le monde!

Dre Elena Antoniadis

Dr Steve Joordens
Dre Elena Antoniadis, Dre Elizabeth Bowering, et Dr Steve Joordens, Enseignement de la psychologie
L’enseignement de la psychologie est une science où tout ne se passe jamais exactement de la même manière. Les groupes et les contextes d’enseignement influencent tous l’apprentissage, et ce, de multiples façons. Le Mois de la psychologie met en vedette aujourd’hui la Dre Elena Antoniadis, la Dre Elizabeth Bowering et le Dr Steve Joorden, qui nous parlent de leur travail.
Enseignement de la psychologie
Le Dr Steve Joorsens, professeur de psychologie à l’Université de Toronto, utilise une analogie pour expliquer ce qu’est l’enseignement de la psychologie :
« Je vois l’enseignement comme un art. Comme de la bière artisanale – si vous voulez être un bon brasseur, qui produit une bonne bière, vous devez connaître les éléments scientifiques des recettes et la façon de les combiner. Il y a aussi un élément subjectif. Le mélange d’ingrédients qui vous convient vraiment peut, pour une raison ou une autre, ne pas convenir à quelqu’un d’autre. Ainsi, il y a un mélange de connaissances scientifiques – les ingrédients qui pourraient constituer une expérience pédagogique marquante – mais ensuite, le professeur lui-même doit trouver ce qui lui convient, et ce qui convient à sa classe et au contexte dans lequel il enseigne. C’est là que l’art entre en jeu, fusionnant les éléments scientifiques avec l’humain pour créer une expérience pédagogique exceptionnelle pour les étudiants. »
Le brasseur Whiprsnapr Brewing Company, de Bells Corners, en Ontario, a créé une bière artisanale appelée OK Lah. Il s’agit d’une Cream ale d’inspiration sud-asiatique fabriquée avec de la coriandre et du gingembre. Elle n’est certainement pas à la portée de tous les palais, et quand j’en ai envoyé à ma sœur, elle est restée dans son garage pendant deux ans, car elle était considérée comme « la bière dont personne ne veut ». Cela dit, elle demeure l’une des plus vendues année après année. C’est une formule qui a fait ses preuves et qui convient à beaucoup de personnes, mais pas à la plupart des gens. Comme c’est le cas de l’enseignement de la psychologie, l’inspiration peut venir de n’importe où, mais la mise au point de la formule gagnante dépend de l’individu.
La Dre Elena Antoniadis est membre du corps professoral de la Red Deer Polytechnic en Alberta et est également membre du corps professoral de l’Université de Calgary. Elle est la présidente de la Section de l’enseignement de la psychologie de la SCP et fait de la recherche sur les façons d’intégrer les applications des neurosciences fondamentales à l’enseignement afin de soutenir et de faciliter l’apprentissage des étudiants des cycles supérieurs.
« La pédagogie de l’enseignement de la psychologie est un champ de formation et de recherche qui s’intéresse aux approches fondées sur la recherche qui permettent d’améliorer l’enseignement et l’apprentissage en classe, explique-t-elle. Certaines de ces recherches proviennent de laboratoires qui font des études en sciences cognitives qui enrichiront nos façons d’enseigner. D’autres formes de recherche se font directement en salle de classe. Nous recueillons des données en classe, et ces données peuvent orienter nos pratiques pédagogiques, l’objectif étant de concevoir et de dispenser efficacement des programmes d’enseignement supérieur en utilisant ces études fondées sur la recherche afin d’enrichir la théorie et la pratique pédagogique. »
En 2016, la brasserie artisanale Beau’s de Vankleek Hill, en Ontario, a fait de chacun de ses employés un copropriétaire de l’entreprise. En 2011, elle s’était associée à un organisme communautaire local appelé Operation Come Home afin d’embaucher de jeunes sans-abri pour livrer sa bière. Non seulement elle a une place dans la collectivité qui achète sa bière, mais elle fait participer la collectivité à chaque étape du processus, ce qui lui a valu un énorme succès local. Ce genre d’approche influence une grande partie de l’enseignement de la psychologie, et la participation communautaire qu’elle implique est appelée « apprentissage par le service communautaire ».
La Dre Elizabeth Bowering est professeure de psychologie à l’Université Mount St Vincent et présidente de la Section de l’enseignement de la psychologie. Elle donne une gamme de cours, comme l’introduction à la psychologie, et des cours de perfectionnement. Certaines de ses recherches portent sur l’apprentissage par le service communautaire.
« Dans mon cours sur le développement de l’adolescent, je demande à mes étudiants d’effectuer des activités d’apprentissage par le service communautaire, dit-elle. Ils travaillent donc avec des jeunes qui présentent un risque de décrochage au secondaire. Ils travaillent avec eux, en leur offrant du soutien scolaire et en les encadrant, afin de les encourager dans leurs propres études. Nous essayons de multiples façons d’élargir le processus d’enseignement et d’apprentissage, non seulement pour les personnes qui sont déjà aux études, mais aussi pour les autres. »
La Church Brewing Company de Wolfville, qui se trouve à environ trois pâtés de maisons de l’Université Acadia, produit une Gose exceptionnelle baptisée Saltwater Joys. Une Gose fabriquée avec de l’eau salée, cela semble logique – après tout, l’entreprise est au bord de l’océan. Et il ne peut y avoir de bière plus locale! Mais ce n’est pas parce que quelque chose est là, accessible, et semble génial que cela va nécessairement fonctionner. Le Dr Joorsens le sait bien, car sa spécialité est l’utilisation de la technologie pour améliorer l’apprentissage. Il mentionne qu’au cours de la dernière décennie, les universités se sont montrées plutôt prudentes avant de s’enthousiasmer pour les récentes technologies.
« Dès le stade de l’approvisionnement, les universités sont beaucoup plus prudentes aujourd’hui lorsqu’il s’agit de définir les pratiques pédagogiques et de s’assurer qu’elles sont fondées sur des preuves. Il faut faire de la recherche pour encourager l’usage des nouvelles technologies tape-à-l’œil qu’elles achètent et nous ne laisserons pas les gens les utiliser simplement parce que c’est branché. L’un de nos grands rôles est de créer la base d’éléments probants requise pour soutenir ces technologies. On peut mettre la meilleure technologie entre les mains de quelqu’un, mais si on ne la soutient pas adéquatement, elle risque de ne pas fonctionner et de ne pas être utile. »
La pédagogie de l’enseignement de la psychologie repose sur ces recherches, sur ces instruments et sur la mesure des éléments probants qui sont intégrés à l’enseignement, mais pas seulement à la psychologie. Bien qu’une grande partie de ces travaux aient été réalisés dans des laboratoires ou dans des classes de psychologie, l’objectif ultime est que toutes ces recherches puissent être appliquées à d’autres classes, d’autres manières et par d’autres personnes afin d’améliorer l’expérience d’apprentissage de tous les étudiants. La Dre Antoniadis en donne un exemple :
« Une application pratique pourrait améliorer les interactions sociales en classe, les interactions sociales entre étudiants, mais aussi entre étudiant et professeur. Ou bien, une application pourrait être utilisée pour améliorer la motivation des étudiants, ou pour diriger et orienter l’utilisation des évaluations. »
Selon la Dre Bowering, « peu importe depuis combien de temps on enseigne, on apprend toujours de nouvelles choses, et on est surpris par les expériences qui se vivent à l’intérieur et à l’extérieur des salles de classe. Notre section offre soutien et encouragement aux gens à toutes les étapes de leur carrière : aux jeunes universitaires qui commencent à se faire la main, aux professeurs en milieu de carrière qui ont donné un cours des dizaines de fois et qui veulent apporter quelque chose de nouveau à leur enseignement, voire aux personnes dont la carrière est plus avancée et qui souhaitent offrir du mentorat à d’autres enseignants. L’enseignement de la psychologie est un domaine très vaste! »
La microbrasserie Lake of the Woods a pignon sur rue à Kenora, en Ontario, et à Winnipeg. Comme pratiquement toutes les autres microbrasseries, elle a récemment élargi sa gamme de produits en y ajoutant des boissons gazeuses, par exemple, la racinette Hockeytown. Bien que cela semble s’éloigner des produits standard de la brasserie, cette évolution vers les boissons gazeuses a été un succès pour les brasseries de tout le pays et lui a permis de vendre un autre produit aux personnes qui étaient cloîtrées chez elles pendant les confinements imposés par la pandémie de COVID-19. De la même façon, dans le domaine de l’enseignement de la psychologie, la pandémie a ouvert la voie à des façons de faire qui peuvent être appliquées universellement et avec succès dans l’ensemble du Canada, notamment, en faveur des étudiants, qui pourraient avoir du mal à assumer les coûts liés aux études supérieures.
« Au cours de la dernière année, j’ai fait des recherches sur les ressources pédagogiques ouvertes. J’ai également découvert le Diener Education Fund, qui a été créé par deux psychologues qui, par hasard, forment un couple et qui ont recueilli des fonds pour financer les dégagements d’enseignement des membres du corps professoral qui sont des experts dans certaines sous-disciplines, explique la Dre Antoniadis. Ils peuvent ainsi trouver un expert en psychologie évolutionniste et lui demander d’écrire un chapitre sur la psychologie évolutionniste. Puis un expert en statistiques ou en psychologie du développement, et le fonds financera le dégagement d’enseignement de l’expert pour qu’il puisse écrire ce chapitre. Le Diener Education Fund a conçu un site Web appelé Noba Project où les membres du corps professoral peuvent aller et personnaliser leurs propres manuels. Je peux entrer sur le site et prendre les chapitres de mon choix, qui couvrent la même matière que celle présentée dans les ouvrages publiés par des maisons d’édition de manuels scolaires. J’ai élaboré ainsi mon programme de cours afin de l’harmoniser avec les résultats d’apprentissage. Les modules sont accompagnés d’images libres de droits, de présentations PowerPoint que je personnalise moi-même, et j’ai intégré cette ressource pédagogique ouverte à mon système de gestion de l’apprentissage. Dans notre étude, nous cherchions à savoir si cette méthode pouvait faire vivre une expérience d’apprentissage similaire à celle d’un étudiant qui aurait acheté un manuel auprès d’une maison d’édition scolaire, et nos résultats le confirment. Les étudiants ont vécu une expérience positive et ont obtenu les résultats d’apprentissage du cours. J’ai reçu un courriel d’un étudiant qui m’a dit qu’il venait de perdre son emploi et que s’il avait dû payer les manuels, il n’aurait pas pu suivre le cours. »
« Je nous vois comme des spécialistes du « savoir-faire ». La société remet continuellement sur le tapis des choses que nous pourrions mieux faire : offrir une formation scolaire équitable, offrir un enseignement de haut niveau accessible, tenter d’améliorer les compétences de tous nos étudiants afin qu’ils obtiennent leur diplôme équipés d’une pensée critique aiguisée et d’une grande créativité, et ainsi de suite. S’assurer que les pédagogies autochtones sont représentées dans l’expérience éducative que nous offrons à nos étudiants. La société exprime beaucoup de ces désirs; mais comment faire cela? Et nous sommes les psychologues qui essaient de répondre à cette question. C’est un peu comme si la société décrivait le paradis, et que c’était nous qui construisions les escaliers menant au paradis », explique le Dr Joordens.
La Burton Bridge Brewery, située à Burton-on-Trent, en Angleterre, produit une bitter anglaise baptisée – pour le moment – Stairway To Heaven, en attendant l’inévitable poursuite de Led Zeppelin.
« J’ai récemment découvert le terme “intra-preneur”, un mot qui désigne les personnes qui travaillent au sein d’une organisation en essayant constamment de trouver des manières différentes et innovantes de faire les choses au sein de cette structure, poursuit Steeve. Et je pense que beaucoup d’entre nous, les spécialistes de l’enseignement de la psychologie, sont des “intra-preneurs”, qui se demandent constamment “comment puis-je améliorer les choses? Y a-t-il quelque chose que je pourrais faire différemment pour rendre mon cours plus intéressant?” Enfin ce genre de chose. »
En 2015, le brasseur, copropriétaire (avec Chris Phillips, ancien joueur des Sénateurs d’Ottawa) et intra-preneur Lon Laddell, de la brasserie Big Rig d’Ottawa, a changé la formule et les ingrédients de l’Iron Arse Ale. L’Iron Arse est la bière en édition limitée que crée Lon chaque année à l’occasion de la campagne de lutte contre le cancer de la prostate Ride for Dad. Cela a provoqué une certaine consternation à l’époque, car la formule précédente était très aimée à Ottawa. Mais la nouvelle formule s’est avérée encore plus réussie, et la bière, encore plus savoureuse qu’auparavant. Pour l’heure, j’ai épuisé les analogies, mais, simple suggestion, si vous vous trouvez à Ottawa en mai ou juin, ne manquez pas d’aller déguster une Iron Arse Ale au Big Rig.
 Dre Helen Ofosu
Dre Helen OfosuFévrier, c’est le Mois de l’histoire des Noirs, et la SCP met en vedette des psychologues noirs contemporains tout au long du mois – comme la Dre Helen Ofosu, qui aide les organisations à combattre le racisme structurel grâce à son entreprise I/O Advisory Services Inc., à Ottawa.
La Dre Helen Ofosu est une psychologue du travail et des organisations, une coach pour cadres et une conseillère en ressources humaines, qui a fondé I/O Advisory Services Inc., un cabinet de conseil établi à Ottawa. Elle possède une vaste expérience de travail avec les organisations et de la lutte contre le racisme structurel à plusieurs échelons.
« En général, je travaille avec des organisations, comme les ministères, les entreprises du secteur privé ou les organismes sans but lucratif, qui, souvent, me demandent de les aider à rendre plus inclusif leur processus d’embauche ou à améliorer leur culture organisationnelle. Au cours des dernières années, j’ai fait beaucoup de formations sur l’équité, la diversité et l’inclusion, auxquelles s’est ajoutée la problématique de l’antiracisme et de la lutte contre l’oppression.
Cet hiver, ce qui m’enthousiasme le plus, c’est de travailler avec un grand ministère sur un programme de mentorat assez unique. Nous dispensons une formation initiale aux mentors pour nous assurer qu’ils comprennent certains des problèmes rencontrés par les employés racisés qu’ils tentent d’encadrer. L’idée derrière cette formation est que, avec une plus grande sensibilisation et une meilleure compréhension, les mentors ne contribueront pas à certains des problèmes auxquels sont confrontés les employés racisés. En outre, en acquérant une vision plus réaliste, les mentors pourront mieux cibler leurs interventions. Il s’agit d’une formation pour les mentors, mais aussi d’un accompagnement pour les mentorés, au-delà du soutien apporté par les mentors.
En gros, l’objectif au cœur de la formation est de soutenir les personnes et même les organisations qui sont aux prises avec des problèmes en rapport avec l’intimidation et le harcèlement et, bien sûr, avec diverses formes de discrimination. »
La Dre Ofosu a récemment parlé de la « Grande Démission » et écrit sur le sujet. Dans les deux dernières années, depuis le début de la pandémie, elle a remarqué que beaucoup d’employés racisés décident de changer de travail, car ils se rendent compte qu’en travaillant à domicile, ils ne sont plus soumis aux outrages quotidiens qu’ils subissent dans un lieu de travail physique.
« Ce genre de choses se produit depuis des années, mais maintenant, les gens ne sont plus dans l’environnement habituel, et ils ont la tranquillité d’esprit que procure le fait de pouvoir travailler sans se soucier des microagressions, ou craindre de se faire regarder de travers ou d’être exclus des pauses-café, des déjeuners et des conversations. Lorsque tout cela disparaît, les gens se sentent beaucoup plus détendus car ils peuvent se concentrer sur leur travail.
Je crois que le véritable déclencheur a eu lieu à l’été 2021, au moment où de nombreuses organisations planifiaient le retour au travail de leurs employés. Ce n’est que lorsque les gens ont commencé à réaliser “Oh mon Dieu, je vais peut-être devoir retourner au bureau” qu’ils se sont mis à se dire “Un instant! Je ne pense pas être capable de retourner au bureau. Je ne veux pas retourner au bureau! Je ne veux pas retourner à ce que les choses étaient avant” ».
Pendant tout ce temps de réflexion, beaucoup de gens ont jugé qu’il était opportun pour eux de changer d’emploi et de trouver un lieu de travail où il y a plus de représentation, plus d’inclusion, plus de diversité, en somme, un milieu où il y a une meilleure culture organisationnelle. D’après ce que j’ai vu, les gens réfléchissent à plein de choses pendant la pandémie. Ils tentent donc de trouver un emploi où ils peuvent être eux-mêmes et se concentrer sur leur travail au lieu de chercher continuellement à se protéger contre les agressions psychologiques. »
Dans une certaine mesure, comme elle est travailleuse autonome, la Dre Ofosu est protégée personnellement contre ce genre de choses. Il est heureux qu’elle continue à faire son travail, car elle est parmi les très rares psychologues noirs à faire ce travail dans cet espace – un travail qui est plus que jamais d’actualité, et qui a plus d’importance et d’impact qu’il n’en a jamais eu.

Dre Nasreen Khatri

Dre Colleen Millikin
Dre Nasreen Khatri et Dre Colleen Millikin, Développement adulte et vieillissement
La psychologie du développement adulte et vieillissement est l’étude, l’évaluation et la gestion du fonctionnement physique, psychologique, cognitif, émotionnel et social des personnes âgées de 18 ans et plus et comprend le vieillissement sous toutes ses formes, les étapes, les joies et les défis. Dans le cadre du Mois de la psychologie d’aujourd’hui, le Dr Nasreen Khatri et la Dre Colleen Millikin discutent du travail qu’ils font dans ce domaine.
Développement adulte et vieillissement
« Ce n’est pas votre faute. C’est votre cerveau qui vous laisse tomber. »
La perte de mémoire est encore, à ce jour, fortement stigmatisée. C’est pourquoi la Dre Colleen Millikin utilise cette phrase lorsqu’elle parle à des personnes âgées atteintes d’un trouble cognitif léger ou de démence.
« Les gens ne le prennent pas personnellement quand ils marchent et que leur genou lâche. Mais ils réagissent différemment lorsqu’il s’agit de leur cerveau. Si notre cerveau nous lâche et que nous n’arrivons pas à trouver tel mot ou tel nom, nous avons tendance à nous en vouloir beaucoup plus que si c’est notre genou qui nous lâche. »
La Dre Millikin est neuropsychologue clinicienne au programme de psychologie clinique de la santé de l’Office régional de la santé de Winnipeg et professeure adjointe au département de psychologie clinique de la santé de la Faculté des sciences de la santé Rady de l’Université du Manitoba. Elle est la présidente de la Section du développement adulte et vieillissement de la SCP. Elle travaille principalement dans le système public, où elle évalue les personnes âgées présentant un risque de trouble cognitif léger ou de démence. Le terme « trouble cognitif léger » (TCL) est utilisé pour décrire les problèmes de mémoire qui se situent entre le vieillissement normal et la démence. Comparativement à d’autres personnes du même âge, les personnes atteintes d’un TCL présentent un risque plus élevé de démence à long terme.
« Beaucoup de choses peuvent interférer avec la mémoire sans que ce soit la maladie d’Alzheimer ou des problèmes cérébraux. La douleur chronique et les médicaments pour la traiter, les problèmes de sommeil, le stress, l’ESPT, en fait, plein de choses. Le simple fait de penser que vous pourriez être atteint de démence peut être une source d’anxiété, et l’anxiété peut rendre plus difficiles la concentration et la mémorisation des informations. »
Le domaine de la psychologie du développement à l’âge adulte et du vieillissement est très vaste. Il s’agit de l’étude, de l’évaluation et de la prise en charge du fonctionnement physique, psychologique, cognitif, émotionnel et social des personnes âgées de 18 ans et plus, ainsi que du vieillissement sous toutes ses formes, incluant ses étapes, ses joies et ses difficultés. La Dre Nasreen Khatri est psychologue du développement de l’adulte et neuroscientifique à l’Institut de recherche Rotman, un institut de neuroscience cognitive entièrement affilié à l’Université de Toronto. Elle est à la fois agréée comme psychologue clinicienne pour adultes (18 à 65 ans) et comme gérontologue (65 ans et plus). Elle est la trésorière de la Section du développement adulte et vieillissement de la SCP.
« Plus précisément, j’étudie les répercussions de la dépression et de l’anxiété sur le cerveau, à partir de l’âge de 30 ans et jusqu’à un âge avancé. La principale idée fausse sur le vieillissement est que le vieillissement est une catégorie d’âge ou un état statique. Ce n’est pas le cas. Il commence dès la conception et est un processus dynamique et continu. Vieillir, c’est tout simplement un autre mot pour dire « vivre »!
La Dre Millikin parle beaucoup de l’étendue du domaine du vieillissement et de grande diversité du travail qu’y effectuent les psychologues. Sur le déficit cognitif, qui est sa spécialité, elle dit :
« L’âge est le facteur de risque le plus important de troubles cognitifs, mais j’ai connu des personnes de 90 ans avec un cerveau en très bonne santé et des personnes dans la cinquantaine atteintes de démence. Il n’y a pas de cause unique aux troubles cognitifs. Dans la plupart des cas, il y a une interaction entre les gènes de la personne et d’autres problèmes de santé. »
Ces problèmes de santé sont mieux compris depuis quelques années, en grande partie grâce aux psychologues qui travaillent dans ce domaine.
« Nous savons maintenant que l’activité physique favorise la croissance de nouvelles cellules dans la partie du cerveau qui influence l’humeur et la mémoire. La meilleure chose à faire pour votre cerveau et pour bien vieillir est de pratiquer des activités physiques. Nous savons également désormais que les personnes qui ont des antécédents de dépression non traitée dans la quarantaine ou la cinquantaine ont presque deux fois plus de risques de développer une démence plus tard dans leur vie comparativement à celles qui n’en ont pas. La dépression est tout à fait traitable au moyen d’une variété de traitements fondés sur des données probantes. Actuellement, la démence est incurable. Par conséquent, il ne faut laisser personne s’engager sur la voie du déclin cognitif et de la démence en raison d’une dépression non traitée. L’évaluation et le traitement opportuns de la dépression aujourd’hui peuvent prévenir la démence plus tard. En d’autres mots, prendre soin de sa santé mentale aujourd’hui pourrait sauver son cerveau demain! »
Idéalement, les interventions visant à promouvoir la santé du cerveau devraient commencer le plus tôt possible dans la vie. Toutefois, il est prouvé que le fait de modifier son mode de vie peut réduire le risque de développer une démence, même chez les personnes présentant déjà un déficit cognitif léger. C’est ce que la Dre Millikin et sa collègue, Lesley Koven, une gérontologue clinicienne, cherchaient à aborder lorsqu’elles ont mis sur pied, en 2013, la Early Cognitive Change Clinic for Older Adults, un programme d’évaluation et d’intervention pour les personnes âgées présentant un déficit cognitif léger. La clinique propose une évaluation pour identifier les personnes souffrant de troubles cognitifs légers ainsi qu’un entretien pour évaluer les besoins psychologiques du conjoint de la personne concernée ou d’un autre membre de la famille ou ami proche.
« Nous offrons un programme d’éducation thérapeutique aux personnes atteintes de TCL et aux membres de leur famille afin de les aider à se familiariser avec le TCL, les stratégies permettant de contourner certains problèmes de mémoire et les habitudes de vie qui favorisent la santé du cerveau. L’exercice et l’alimentation sont bien sûr importants, mais nous constatons également que le sommeil joue un rôle majeur. Le sommeil est très important pour la santé du cerveau, mais les personnes âgées ont tendance à avoir des problèmes de sommeil à un niveau plus élevé. L’un des problèmes vient du fait que le manque de sommeil est mauvais pour la mémoire, mais aussi que beaucoup de médicaments sur ordonnance ou en vente libre que les gens prennent pour dormir peuvent interférer avec une substance chimique présente dans le cerveau qui est importante pour la mémoire. Heureusement, il est possible de modifier son comportement pour mieux dormir et l’insomnie peut être traitée par des interventions psychologiques! »
En outre, les membres de la famille des personnes atteintes de troubles cognitifs légers peuvent également ressentir un stress important. Encore une fois, la Dre Millikin insiste sur les répercussions que peut avoir une intervention précoce.
« Nous reconnaissons de plus en plus les besoins des aidants. Nous savons depuis longtemps que les membres de la famille des personnes atteintes de démence peuvent ressentir un stress important. Même lorsque le trouble cognitif est léger, les membres de la famille ou les amis proches peuvent tout de même éprouver un certain stress dû à la situation, même s’ils ne se considèrent pas comme des « aidants ». Donc, si l’on souhaite intervenir pour aider un membre de la famille à gérer son stress, on doit commencer le plus tôt possible.
Il existe de nombreuses autres facettes de la psychologie du vieillissement et du développement de l’adulte, toutes aussi importantes les unes que les autres. La Dre Millikin en donne quelques exemples.
« La Dre Kristin Reynolds, qui est professeure adjointe aux départements de psychologie et de psychiatrie de l’Université du Manitoba, a mis sur pied un programme de soutien téléphonique pour aider les personnes souffrant de solitude pendant la pandémie. Le président sortant de la Section du développement adulte et vieillissement, le Dr Marnin Heisel, fait des recherches à l’Université Western pour trouver des façons de réduire le risque de suicide chez les hommes âgés. La Dre Norah Vincent, une collègue de mon département, a élaboré des programmes de thérapie cognitivo-comportementale en ligne pour traiter l’insomnie. »
La Dre Khatri affirme que la pandémie a eu un impact profond sur les personnes âgées, allant de la santé mentale (p. ex., dépression et anxiété) jusqu’à l’aggravation des problèmes systémiques qui affectent depuis longtemps les soins de longue durée.
« Elle a mis en lumière la façon dont nous traitons nos aînés et la façon dont nous devrions les traiter. Le moment est venu de repenser les politiques de soins, et les politiques gouvernementales et sociales qui ont un impact sur les Canadiens vieillissants. Le Canada est une nation vieillissante et, dans le futur, nous devrons appliquer des politiques systémiques qui optimiseront la santé de notre cerveau (santé mentale et cognitive) et nous permettront de vieillir dans la dignité, l’autonomie et le bonheur. L’avenir de la santé du cerveau au Canada est entre nos mains, et l’un des meilleurs moyens de prédire notre avenir est de le créer.
Enfin, la pandémie nous a appris que nous devons nous concentrer sur notre mode de vie personnel (alimentation, exercice, repos, liens sociaux) à tout âge pour préserver notre santé physique, émotionnelle et cognitive et notre épanouissement. »
Autrement dit, il existe de nombreuses façons d’empêcher votre cerveau de vous laisser tomber. Cela étant dit, cela pourrait arriver quand même. Et si c’est le cas, il est important de se rendre compte que ce n’est pas votre faute.

Joanna Collaton
Joanna Collaton is the CPA’s Student Representative at the University of Guelph, the Past President of the Student Section, the editor of the student publication MindPad, and over the past three years has been involved with the CPA in just about every way a student can be.

Dr. Adrienne Leslie-Toogood and University of Manitoba psychology student (and Olympic swimming medallist) Chantal Van Landeghem discuss the mental health of elite athletes in the wake of Naomi Osaka’s withdrawal from Wimbledon.

Caryn Tong

Rohit Gupta
Last year Caryn Tong mentored Rohit Gupta through the CPA Student Mentorship Program. While both were looking for experiences that differed from their own, they found many similarities in one another.
 Dr. Justin Presseau
Dr. Justin PresseauPsychology Month has been extended two days, so we can bring you the work of Dr. Justin Presseau, who is co-Chairing a working group of behavioural scientists advising Ontario healthcare executives and government representatives on best practices during the COVID-19 pandemic.
Justin Presseau
Dr. Justin Presseau is going to welcome a new baby in about a month. His wife Leigh is eight months pregnant, which means this new child will be born in the middle of a global pandemic.
This adds one more job to Dr. Presseau’s portfolio, which also includes Scientist at the Ottawa Hospital Research Institute, Associate Professor in the School of Epidemiology and Public Health and in the School of Psychology at the University of Ottawa, and the Chair of the Health Psychology and Behavioural Medicine Section of the CPA.
As with many researchers, much of Dr. Presseau’s work had to pivot because of the pandemic. He leads a team co-developing new ways to support new Canadians with diabetes to be comfortable taking an eye test. Retinopathy is a manageable issue for people with diabetes when identified through regular screening but attendance rates could be improved, and so Dr. Presseau and his team are building relationships with different communities and community health centres virtually.
Another thing that’s difficult to do from a distance is blood donation. Dr. Presseau and his team are working with Canadian Blood Services and local communities to develop approaches to support men who have sex with men who may want to donate blood plasma, as screening and deferral policies continue to change to allow more MSM to donate if they want. Part of that work involves addressing the historic inequities that led to the exclusion of these men in the first place. But then – there was a pandemic, and his team like so many others have pivoted to continuing to develop key community relationships and campaigns virtually.
In addition, Dr. Presseau is tackling a lot of COVID-related projects, like for example a national survey of to understand what factors are associated with touching eyes, nose and mouth. The research is changing as we continue to develop an understanding of how COVID-19 is transmitted.
Maybe the most important of these COVID-related projects is the , a group of behavioural science experts and public health leaders who summarize behavioural science evidence in the context of COVID-19 and identify actionable guidance for Ontario’s pandemic response. Dr. Presseau is the co-Chair of this working group, which also involves CPA President Dr. Kim Corace.
“We sit within the larger Ontario Science Advisory Table. We’ve brought together expertise in behavioural science and particularly psychologists across Ontario, based both in academia and within government, to work alongside public health experts and ministry representatives.”
Dr. Presseau says that because the working group contains representatives from all these different areas and the team can communicate directly in this setting with decision makers and policy creators, it is the most direct form of knowledge transfer and knowledge mobilization of behavioural science in which he has been involved in his career.
“From an impact perspective, we get to translate our science to people who can make use of it right away, and they can also provide feedback to us – what are they looking for? What’s helpful to them? Of all the things I’ve done in my career this feels among the most impactful. One of the hats I also wear in the hospital where I’m based is Scientific Lead for Knowledge Translation [in the Ottawa Methods Centre], so I think about knowledge translation a lot. The ability to connect directly with those in the field that are making a difference is excellent. It’s also such a validating experience for me, as a behavioural scientist and a psychologist, to see that there’s recognition of our science and a need for an understanding of how we can draw from the behavioural sciences to support Ontarians and Canadians.”
The Behavioural Science Working Group is currently focused on vaccine confidence and uptake among health care professionals. Over 80% of Ontario health care workers say overwhelmingly that they intend to receive a COVID-19 vaccine when it is available to them. The working group is looking to communicate behavioural science approaches to support healthcare organisations across the province to optimise their vaccine promotion programs – for instance, by clarifying that despite having been created at record speed, these vaccines have been shown to be safe and effective and it’s important that those in the healthcare field get one.
Part of this is modeling good behaviour for the rest of the population. And within the healthcare field, modeling good behaviour is one way the working group is hoping to reach those who may be undecided. It’s one thing to have politicians and celebrities get vaccinated publicly, it’s another far more effective thing for your peer group, and hospital CEOs, and team leaders, to do so in front of your team.
Much of this work involves drawing on the literature from around the world to inform hospital policy or public policy. But some of it happens directly, and goes in two directions. For example,
“Our co-chair Dr. Laura Desveaux and her team did surveys with healthcare workers that not only ask if they intend to get the COVID vaccine, but also ask questions that are drawing from behavioural science and psychological principles around the specific constructs or factors might be associated with greater or lesser intention. So they were able to identify key predictors in healthcare workers in January of 2021, the most current data we have. So it’s kind of exciting to be able to quickly draw from on-the-ground data, iterate principles, and push that out to the field to support those who are doing this.”
We have asked most of our Psychology Month participants if they see a ‘silver lining’ in the pandemic. Something that is good, but that would not otherwise have happened absent the pandemic. Dr. Presseau says one silver lining is that it has highlighted just how important and relevant health psychology and behavioural medicine are to understanding and supporting health behaviour change and health and well-being during pandemics.
“After all, behaviour underpins most if not all the public health measures and vaccination activities that are key to seeing the other side of this pandemic.”
When Leigh and Justin’s baby is born, the pandemic will still be ongoing. But that baby will be born into a world that has a much greater understanding of pandemic science, of the behavioural science that accompanies it, and with more and more diverse teams of interdisciplinary experts working together to solve problems – locally, provincially, nationally, and globally.
One day, this baby will grow into a person who can take pride that Dad had a lot to do with that.
 Silver Linings in the Pandemic
Silver Linings in the PandemicPsychology Month has focused on dozens of aspects of the pandemic, a global catastrophe that is deeply tragic. To close out Psychology Month, we focus on a few positives that have come about as a result of COVID-19.
Silver Linings in the Pandemic
It has been a tough year for everyone, and so Psychology Month this year has been tough as well. No matter how many innovative, creative, dedicated psychologists are doing incredible things, it’s tough to forget the reason why. A pandemic that has ravaged the globe, caused untold economic damage, mental health issues, and more. Above all, we can’t forget the two and a half million people who have died as a result, which makes the subject of this year’s Psychology Month deeply tragic.
It is for this reason that we want to end on a high note, in as much as such a thing is possible. We asked many of the psychologists who were profiled for Psychology Month to tell us something good they saw come of the pandemic. A personal or professional observation of a way things had improved despite the global catastrophe. Here is what many of them had to say:
“Across hundreds of universities, dozens of countries, many languages, many disciplines, from the virologists to the immunologists to the mental health practitioners – all these people are working together over months. And doing this work under pandemic conditions, doing this work in labs that themselves could cause a super-spreader event. It’s an amazing human accomplishment that we’re already talking about how to get it under control.”
- Andrew Ryder
“One thing that amazed me was how quickly our field – psychology – was able to pivot to online services and mostly remote delivery of therapy when beforehand it was more of an exception to the rule to see people online or over the phone. Seeing that in-person visits can sometimes be adequately replicated via Zoom, or the phone, or other technologies, has been a really interesting experience for me as a trainee.”
- Chelsea Moran
“It wasn’t on the radar at all to offer virtual group psychotherapy for chronic pain, or for psychologists to have virtual appointments. The way Quebec is set up, we cover people who live seven, eight hours away from our centre. For them, being able to have weekly sessions with a psychologist is something that’s very precious. And for others in chronic pain where even thirty or forty minutes driving in the car to the hospital brings their pain level from a three to an eight, not having to come in on some days can be helpful as well. It’s a door that opened that wouldn’t have opened as fast had it not been for the pandemic.”
- Gabrielle Pagé
“There are certain people who, pre-pandemic, were super-productive and making amazing contributions at work. But because they weren’t bragging, and because they weren’t charismatic, they didn’t get the attention of their bosses and they were kind of overlooked. But now when everyone’s at home, it’s easier to track who’s contributing stuff, who is sending in work product. So all the ‘do-ers’ are getting their chance to shine.”
- Helen Ofosu
“I think the move toward virtual care is something that many many patients find very positive. In the capacity that they’re able to receive care from their home, rather than having to work to get themselves or their children or their family over to the hospital. Parking, and having to sit in a waiting room to come to your appointment – to know that you can do it from home is a huge advantage for a number of patients. This has really pushed us to advance in this area that is a real advantage for many of our patients.”
- Ian Nicholson
“For me, it’s being able to spend time on things I really enjoy. I really like to bake, and I really like to read non-academic books. I love murder mysteries! Being able to give yourself permission to actually engage in the activities that you enjoy, that are non-work-related, that are just for you, to me has been my silver lining.”
- Joanna Pozzulo
“Now that the pandemic has gone on for a long time, I don’t really miss the things like international travel – those were perks. But the things I do miss are seeing my family more, my friends more. Some of these things were clarifying, that the things I thought I was missing were perks but not necessary. As soon as I started giving up on my expectations and the things I was missing, it became easier to deal with them, and easier to reach out to other people for connection.”
- Vina Goghari
We also asked our members to point out some ‘silver linings’ in a poll question we included in our monthly newsletter. Here are some highlights of the responses we received:
“The involuntary aspect for many people to slow down as they were laid off or take time to quarantine and are forced to take time off from vacations and traveling is an opportunity to reflect on goals, and "reset" intentions coming out of the pandemic.”
- Charlene F.
“I have seen increased accessibility to services for people with disabilities.”
“I have seen distance barriers disappear - people are able to access learning, support, and other services virtually no matter where they are (assuming they have access to reliable internet!).”
- Gillian S.
“One positive thing for me was that I left my office and started to work virtually from home. It is much easier for me not to have to drive and find parking, and I don’t have to pay rent. The clients are really happy with that option, too, because it is a lot easier for them not to have to take a half day off work to come to the office.”
- Sharon Z.
“More people enjoying the great outdoors!”
- Julie B.
“One positive thing that I have seen come out of the COVID-19 pandemic is an increased societal focus on the importance of both mental health and social justice.”
- Danial A.
“I'm a third-year undergraduate psychology student at Ryerson. I've really been struggling with adjusting to an online semester, work from home, and volunteering and researching from home. This time has really challenged my mental health, but something positive that has come out of this pandemic is that for the first time in my life I am actually putting my mental health first and prioritizing my own wellbeing. I think I'll come out of this pandemic with so much self-growth, and I truly believe if I did not have so much time alone with my own thoughts, I would not have gone through this self-care journey.”
- Giselle F.
“I have noticed that staying at home has increased my focus on family life. Learning new and fun activities to keep the family busy while staying away from everyone we used to visit. For example, we have discovered new trails in our local area which is difficult because we are already active hikers so know most of the trails. Also, we have taken up painting rocks and searching for others' painted rocks on the more common trails.
As a student I have noticed a high increase of togetherness among students. There is a massive use of discord in the psychology department at VIU. This has helped to stay on top of school work and have discussions about our projects or simply to figure out how to get onto the zoom link the teacher put in a funny spot we can't find. Also on the psychology discord site, students are looking at common interests like gaming that they can do together and discussing various interesting novels that they enjoy.
I have never felt so connected to other students while walking around campus. Now I can log on and ask about test topics or paper ideas.
It's been tough distancing from everywhere, but I realize family life is the most important thing in my world and will not disappear from my life. School is a long term goal and I know one day I will be done with it, COVID is just a bump in the road.”
- Donna S.
“The pandemic has been grounding in the sense that many people have suddenly recognized and remembered the most important aspects of life. When faced with a universal threat to health and livelihood, the superficial details of a day become recognized as such, and the aspects with the most weight and meaning to our lives become clear.”
- Kathryn L.F.
“I believe that this pandemic has taught most individuals the importance of well-being. Seeing as we are no longer under the extreme pressures of traveling from day to day events, we now have more time for self-reflection, personal examination, questioning, and learning. It takes a certain level of resilience to shift perspective from uncertainty and anxiety to gratitude. However, with the pandemic disrupting what we knew as our normal lives and continuing to do so, those who are fortunate enough have been able to embrace this shift. Despite what may be happening in the world the most important thing we can focus on and should focus on moving forward is our overall well-being.”
- Emily T.
“A personal silver lining of the pandemic was having the time to finish my research and apply for residency a year earlier than anticipated. I also had more time to spend with my fiancée since both of us were working from home.”
- Flint S.
“More slowing down. A chance for children to play and be.”
- Jen T.
“Something positive I have seen from the pandemic is a newfound appreciation for in-person interactions, particularly in the younger generations. With so much screen time and so little face to face interaction, not only is in-person socializing of higher value, it’s become higher quality. I’ve noticed people are more likely to put their phones away and live in the moment. Interactions are limited, and we need to make the most of what we get. In my own life and for many of my friends, family, and classmates, it’s been something we’ve come to stop taking for granted.”
- Genevieve J.
“Psychologists being forced to become familiar with providing telehealth services, and the increased access that has provided.”
- Janine H.
“Nonobstant la dure réalité de la pandémie, beaucoup de réalités positives ont émergées. En premier lieu, l’esprit d’entraide et communautaire. Deuxièmement, la créativité, que ce soit dans toutes les formes d’art en tant que telles, mais aussi dans l’adaptation, la réinvention et la recherche de solutions. Troisièmement, toutes les nouvelles habitudes acquises, que ce soit le jardinage, l’exercice, l’apprentissage d’une langue, d’un instrument de musique ou d’une habileté ou encore de connaissances en général. Pour ce qui est de la psychologie, en particulier, la création de portails sécuritaires pour offrir des services en ligne.”
- Elisabeth J.
“Something positive in the pandemic- people have slowed down and reassessed their priorities, needs, and desires.”
- Heather P.
“The negatives from a global pandemic have been catastrophic. The most damaging effects being the crippling of the economy, deaths of millions of loved ones world wide, and an extreme toll taken on people's mental health in so many different ways. Keeping children away from school and their friends, forcing families to remain in abusive situations under the radar, allowing small business's to close down permanently day by day... this damage will take years to repair, and maybe won't be repairable at all.
This cannot be forgotten; however, in order to keep my head above the waters of these unforgettable events, I choose to remain optimistic and seek the positive in a sea of negative.
I remind myself that I have been given a chance to spend quality time with the most important person in my life - myself. People tend to neglect themselves daily, and I believe this pandemic has allowed us to check in with ourselves and take the time to look after our needs and self care. I also think that we often neglect the loved ones in our life. This time of isolation has encouraged me to pick up the phone and call people that I have not spoken to in a long time. I have called my parents more than ever before. I even call my friends instead of just sending them silly photos back and forth on Instagram. These conversations are meaningful. When we are allowed windows of social gathering, these windows are so meaningful also.
Besides these main points, I think that there are some little positive outcomes as well such as cooking more meals at home that are healthier for our bodies and mind, spending more time in nature and trying new activities we never would have tried otherwise, and of course, saving money if you are lucky enough to keep your job.
Negativity will drown you if you let it and positivity will keep you afloat. “
- Sacha H.
“Since COVID, I have become closer with my roommates. We spend more time together instead of doing our own thing all the time.”
- Laura J.
“1] a lot of children may be spending less time on screens by going outside tobogganing, building snow forts, and snowmen.
2] parents are actually spending more time with their children that they did before such as helping and supervising homework but also playing like colouring together and even playing non-screen table games like the good old days, monopoly, snakes and ladders etc.
3] couples like myself with my wife spend more time having coffee together and talking about all things which there may not have been time for before when people ran off to work for the entire day.”
- Jack A.
“I work in education, and I see teachers paying more attention to their own mental health. We bend over backwards for the kids we work with, but it is rare for a teacher to step back and say "I am not okay", and I have seen more of that this year than ever before. They are getting the help they need and taking time off to rest and heal. I hope this continues as teacher burnout is a real thing.”
- Danielle F.
Thank you to everyone who followed along with Psychology Month in 2021. This past year has been difficult, and it has been hard to put into words. Thankfully, there are psychologists all over Canada willing to try. We salute them all, and we salute the resilience of Canadians who have weathered this storm with diplomacy and aplomb. Take care of yourselves, and those around you.

Psychology Month has focused on dozens of aspects of the pandemic, a global catastrophe that is deeply tragic. To close out Psychology Month 2021, we focus on a few positives that have come about as a result of COVID-19.
 Dr. Karen Cohen
Dr. Karen CohenThe CPA has been adjusting, like everyone else, to working from home and embracing the new normal. Our work has been guided by our CEO, Dr. Karen Cohen.
CPA’s Communications Specialist, Eric Bollman talks to CPA’s CEO, Karen Cohen
“The tail of COVID is going to be a long one. It’s going to be psychosocial, and financial. Long after we get vaccines, long after we achieve population immunity, we’re still going to be addressing the psychosocial and financial impacts of living through a pandemic this long.”
Shortly after the NBA announced the suspension of their season on March 11, 2020, there was an all-staff meeting at the CPA head office in downtown Ottawa. The realization was dawning on everyone, and fast, that we were about to enter a different world – both in terms of our own work lives, and in terms of the role of psychology in the world at large.
We knew things were changing – if the NBA could shut down, the rest of the world was not far behind. We knew we’d all be sent home, and we spent that meeting discussing how that would work. Who needed a laptop? Who needed a refresher on Microsoft Teams, having slept through the training session less than a week before? What we did not know was that this would be the last time we saw each other in person for more than a year.
Our CEO, Dr. Karen Cohen, does not follow basketball. For her, the realization was more incremental. But she reached it at the same time, if not a little before, the rest of us. She made the decision to shut down the office and send everybody home.
“We were trying to make the decision that not only would best take care of our workplace, but that would make us a good corporate citizen. It was clear that if the world was going to be successful in managing the pandemic, we had to put in a community effort. “
As the world changed, and the CPA started working from our homes across Ottawa and connecting with people across the country, we realized that psychology was going to have an outsized role to play in helping people and communities manage the pandemic. CPA wanted to help in that effort. Dr. Cohen credits the staff at the CPA for making this transition work, almost seamlessly.
“Everything CPA has been able to contribute to managing the pandemic is to the credit of the association’s leadership, its membership and its staff. From the outset, our goal was to listen and respond to what people needed; what staff needed to work efficiently from home, what individuals and families needed to support each other, what members needed to face disruptions in their work, and what decision-makers needed to develop policies to help communities.
At first though, those lockdowns were not extended – we truly thought we’d be back at work in a few weeks, maybe a couple of months. Karen and the rest of the management team made sure to check in, and to cover their bases early on.
“One of the things we did at the outset was to survey staff – asking what’s keeping you up at night? How can we make things better? What are you most concerned about? And not just to ask the questions but to try to do something about them. We developed policies and made decisions that considered the things staff were worried about and responded to what they needed. We realized that psychology had some tools and suggestions to help them cope so we developed a webinar for staff on coping and resilience. We also reached out to staff one on one and really tried to hear them so we could help make things easier for them.”
We then thought that the survey and webinar might be helpful to the staff of other of CPA’s not for profit association partners and we delivered them to about a dozen of them. The survey enabled leaders to better understand the needs of their workplaces and psychology had some tools and suggestions to help workers cope. Something that was created internally, for the use of our own staff, ended up being of value to other organizations and an unforeseen contribution our team has been able to make.
While we didn’t know how long the pandemic would last, or what the long-term effects would be, the one group we knew for sure would be affected long-term were frontline health care workers. We were already seeing reports from Italy and Spain of overflowing hospitals, a health care system in crisis, and doctors and nurses overcome with exhaustion and despair. So what could we do?
The first major effort of the CPA during the pandemic was to ask our practitioner members if they would be willing to offer their services to frontline healthcare workers, on an urgent basis, as they faced the stressors of delivering health care services during a pandemic. It seemed essential that the people who were out there fighting against this scourge of a virus had every support possible as they took care of everyone else and, because of their work, faced heightened risk of contracting the virus and bringing it home to their families.
“Hundreds of psychologists came together to do that. It was good for CPA, it was good for psychology, and most importantly, it has been good for the health providers psychologists helped.
From there, it was a question of developing and delivering information, and getting as much of it out to members, decision-makers and Canadians as possible. Psychologists across Canada answered the call to help create more than a dozen COVID-specific fact sheets for students, psychologists, faculty, people working from home and more. Our team developed webinars, started a podcast, and undertook the herculean effort of moving the CPA annual convention online with just a few months notice.
The CPA team has been collaborating with innumerable other organizations and agencies, commissioning surveys and public opinion polls, and advocating for mental health to be front and centre in every governmental pandemic-related decision and policy across Canada. The work is ongoing, and it is not likely to stop any time soon.
“We know that rates of anxiety, depression and substance use have gone up as people cope with this prolonged chronic stressor. We can see the impact managing the pandemic has had on our work, relationships, and wellbeing. Maybe the pandemic has shown us that a pandemic takes as much of a psychological toll on our lives as a biological one. Maybe the pandemic has shown us that managing a critical health event successfully is as much about psychological and social factors as it is about the biological ones. Maybe, governments, workplaces, and insurers will fully realize that mental health matters and that it is time that making investments in mental health care matters too.”
 Dr. Jenn, Dr. Laila, and Dr. Mary
Dr. Jenn, Dr. Laila, and Dr. MaryFriends since they did an internship together at the Children’s Hospital of Eastern Ontario, child psychologists Dr. Laila Din Osmun, Dr. Mary Simmering McDonald, and Dr. Jenn Vriend are trying to reach as many kids and parents as they can during the pandemic with the Coping Toolbox podcast.
Laila Din Osmun, Jenn Vriend, and Mary Simmering McDonald
Everyone is swamped. Kids, learning virtually for the past year and dealing with constant uncertainty. Parents, looking after those kids and trying to work remotely or cope with being out of work. Psychologists, whose services are more in demand than ever but who don’t have any spots available for new clients.

Dr. Laila Din Osmun is a parent and a psychologist, dealing with two young children learning from home and an increasing demand for her professional services. She started spending time with her two children, aged five and seven, throughout the week and moved her practice to the weekends. She found she was turning people away because she just didn’t have the availability to see the number of people seeking services. And so she did something that may seem illogical – she added a whole other project to her workload.
In conversation with her friends Dr. Jenn Vriend and Dr. Mary Simmering McDonald, Dr. Din Osmun found that they were experiencing the same thing. The three had become friends during an internship at the Children’s Hospital of Eastern Ontario (CHEO), and now all three were child psychologists in private practice in Ottawa. None of them could keep up with the demand.

How do you get essential information to as many people as possible as quickly as possible? Nothing can replace one-on-one therapy, but there was clearly a void as the supply was not coming close to matching the demand. Dr. Din Osmun proposed a podcast. Coping techniques for kids, delivered one episode at a time, coupled with discussions of the issues facing families during the pandemic and some personal stories about spending time at home with their own children.
The CopingToolbox: A Child Psych Podcast was born. The first episode was published February 17th, discussing specific coping strategies (setting boundaries, practicing gratitude) for children and parents during COVID.

“Everybody’s feeling overwhelmed right now, myself included. My friends, my clients – it’s a really difficult time. One of the things I’ve been practicing is just allowing myself to feel some of those feelings. Sometimes we feel sad and we don’t want to, or we feel anxiety and we don’t want to. But it’s a really difficult time and we’re going through a lot, and I think it’s really important that we allow ourselves to feel that feeling for a little while.”
Jenn Vriend, The Coping Toolbox Episode One
Future episodes will deal with subjects like depression, as the three friends try to bring more services to more people through a new and interesting platform. On the podcast, they refer to themselves as ‘Dr. Laila’, and ‘Dr. Jenn’, and ‘Dr. Mary’. To an outsider, this might remind people of the ‘Dr. Bobby’ episode of Friends (okay it’s me – I’m the outsider who was reminded of that episode) but it also creates a friendly and welcoming atmosphere should kids be listening with their parents. This was clearly an intentional choice, as was the use of the word ‘toolbox’. Says Dr. Laila,
“We called it The Coping Toolbox because we wanted to provide tools for coping. Not getting into too much detail, and we wanted it to be useful. At the end of every podcast we give three coping skills that we review for the people listening.”
In episode one, those skills are; take a few minutes and breathe, modeling positive behaviours for your kids, and being kind to ourselves. On the podcast, Dr. Jenn says;
“We’re modeling positive behaviours, but we’re not doing it perfectly. So we can take a deep breath, do our best to model those positive behaviours, for ourselves as well as our kids, and then just be gentle and kind to ourselves knowing that we’re doing the best we can given the situation.”
All three Coping Toolbox podcast co-hosts know about doing their best given the situation. They all have young children at home, and each of them brings a different perspective. While Dr. Din Osmun has set aside a large portion of her work to take care of the kids while her husband works a demanding job, Dr. Simmering McDonald, a mom of 3- and 5-year-old boys, is balancing her clinical practice with her husband’s long work days, limited childcare, and weekly appointments regarding the health needs of family members.
In The Coping Toolbox Episode One, Dr. Simmering McDonald notes, “it’s important to consider our own well-being and our own mental health. This is necessary for our own functioning but also for the functioning of our kids and our families.” Dr. Vriend speaks about grief, something many people are experiencing with COVID-19. She separated from her son’s father a few years ago, then sadly he passed away in the summer of 2020. “I’ve had to learn not just single parenting but lone parenting, where you’re it – you’re kind of the everything. I think that perspective, during the pandemic, is going to be interesting to discuss. I remember at one point feeling like ‘I’m my son’s entire world’. I’m his teacher, and I’m his coach, and I’m his mom, and I’m his dad, and it felt very overwhelming. It can add a different perspective because there are a lot of people who discuss both parents, and when you’re a single parent it can hurt a little bit and I think the pandemic has created a whole other layer for single parents and for lone parents.”
In professional practice, divulging personal details is not something psychologists do. But in the context of a podcast, doing so can help the narrative hit home – a narrative that, in the case of The Coping Toolbox, is warm, friendly, expert-driven and truly helpful for many who can’t access that help in other ways at the moment. Dr. Din Osmun says,
“It’s been a crazy time, and we just can’t meet the demands right now. It was getting really frustrating, and the three of us kept talking in group conversations – how can we help? We’re so limited in what we can do. We had the idea of creating a podcast, but we knew nothing about podcasting. The three of us are clinicians in private practice, we have no expertise in podcasting whatsoever. It was a huge learning curve, but we figured this IS something we can do to help people because it’s something the three of us can do from home. We felt like this was a way to help more people in a shorter period of time.”
Laila has taken the lead on the podcast, including taking on hosting duties and – the most painstaking and time-consuming job of all – the editing after the fact. It will all be worthwhile if enough people listen and take away something helpful they did not already know.
You can find The Coping Toolbox: A Child Psych Podcast on Apple Podcasts. https://podcasts.apple.com/ca/podcast/the-coping-toolbox-a-child-psych-podcast/id1553993639

Introducing The Coping Toolbox: A Child Psych Podcast. Dr. Jenn Vriend, Dr. Laila Din Osmun, and Dr. Mary Simmering McDonald are three child psychologists from Ottawa.
https://podcasts.apple.com/ca/podcast/the-coping-toolbox-a-child-psych-podcast/id1553993639
 Charles Henry Turner
Charles Henry TurnerCharles Henry Turner was a zoologist, one of the first 3 Black men to earn a PhD from Chicago University. Despite being denied access to laboratories, research libraries, and more, his extensive research was part of a movement that became the field of comparative psychology.
Dr. Turner was a civil rights advocate in St. Louis, publishing papers on the subject beginning in 1897. He suggested education as the best means of combatting racism, and believed in what would now be called a ‘comparative psychology’ approach.
Charles Henry Turner was a zoologist, one of the first 3 Black men to earn a PhD from Chicago University. He became the first person to determine insects can distinguish pitch. He also determined that social insects, like cockroaches, can learn by trial and error.
Despite an impressive academic record, Dr. Turner was unable to find work at major American universities. He published dozens of papers, including three in the journal 'Science', while working as a high school science teacher in St. Louis.
Despite being denied access to laboratories, research libraries, and more, his extensive research was part of a movement that became the field of comparative psychology.
Dr. Turner was a civil rights advocate in St. Louis, publishing papers on the subject beginning in 1897. He suggested education as the best means of combatting racism, and believed in what would now be called a 'comparative psychology' approach. He retired from teaching in 1922, and died at the age of 56 on Valentine's Day in 1923.
Photo: biography.com
 Penny Corkum
Penny CorkumDr. Penny Corkum studies sleep and children, and created Better Nights Better Days, a cross-Canada trial that improved sleep for both kids and parents before the pandemic. In the last year, Dr. Corkum and her team went back to those families to see how they were doing during COVID. Their launch of a revamped Better Nights Better Days for the pandemic era is imminent.
“When we launched our survey study asking parents during the pandemic how their child’s sleep was impacting them, what really came up was that it’s the whole family and not just the child. So we not only had to help the child sleep better but also give strategies for the parent to sleep better. So we added that into the intervention as well.”
It probably goes without saying that sleep is incredibly important for children. Difficulty falling asleep and staying asleep can have a big impact on a child, in terms of daytime functioning. They’re not able to focus or learn as well, and it might result in behavioural problems. Dr. Penny Corkum has been studying sleep in children for a long time. In the last decade, her sleep studies have taken the form of connecting parents and families with the interventions they now know work for children and sleep. Part of this is an e-health program, online tools that parents can access when they need them.
Between 2016 and 2018 Dr. Corkum and her team ran a cross-Canada trial called Better Nights, Better Days, to see if this program was effective. It was, and the program resulted in improved sleep, improved daytime functioning, and even parents were less tired during the day as a result. Then the pandemic hit, and it became a constantly evolving crisis – lockdown for a while, then lockdown lifted. School online from home then back to in-person classroom learning. Right away, sleep patterns were disrupted for both children and adults around the world.
The team went back to the families who had participated in the original Better Nights, Better Days trial, to see how they were doing during the pandemic.
“It seemed like a good place to start because we already knew about their sleep, and we knew that they had learned a lot of strategies to help their child sleep. We were curious – were they still using these strategies? There was some research coming out at the time that suggested families were actually having better sleep, since they didn’t have to get up at a certain time. But that’s not what we found. A small portion of our families were doing better, but about 40% of the children and 60% of the parents were sleeping worse than they were before the pandemic.”
A lot of this was happening because of disruptions in routine and structure. We sleep best when we have consistency in our days – a regular bedtime, a regular time to wake up, a standard time for supper. All of this was being upended by a constantly evolving pandemic and the restrictions that went along with it. Two of the biggest factors were anxiety as a result of worry about the pandemic, and screen time. Kids were using screens a lot more while locked down at home which was disrupting their sleep in a big way.
With new data collected from the Better Nights, Better Days cohort, Dr. Corkum and her team could move forward. Almost all the parents said they were still using the interventions they had used for sleep pre-pandemic. 95% of them said that they thought other families should have access to these strategies during the pandemic. Based on this, the Better Nights, Better Days team was able to get some funding to launch an intervention for all families during the pandemic.
That new program launches Very soon – hopefully very early in March. It is free for families to use, intended for parents of children ages 1-10 who are struggling with falling asleep and staying asleep. There have been slight modifications, now that Dr. Corkum and her team have information about the pandemic and how it impacts sleep. They’ve also added to the intervention some information about parents’ sleep, and how to help parents sleep better. Sleep is essential for the whole family!
Dr. Corkum also runs a diagnostic clinic in Truro, Nova Scotia that brings together pediatricians, school psychologists, health psychologists and others to do differential diagnostics for kids who have fairly complex presentations and need a comprehensive assessment. Well, she normally does. But in the past year the doors have remained closed because they just can’t have all those people together in one room. It’s disappointing for Dr. Corkum and her team, who likely won’t be able to re-open until next year. Therapy can be done virtually, diagnostic assessments not so much.
Dr. Corkum says she misses working at Dalhousie and seeing her students, staff and colleagues but doesn’t miss the walk! Her parking spot is far from the office that carrying a bag, and papers, and a laptop through deep snow or a blizzard makes the walk to work something of a nightmare and a serious workout, every winter. She’s still getting the walk and the workout in – but walking a big dog three times a day is a much more pleasant experience.
Fresh air, exercise, and sleep are three of the things that can make life during the pandemic a more pleasant experience. And with the launch of Better Nights, Better Days which has been modified for the COVID-19 context, Dr. Corkum is making at least one of those things easier and more accessible as of today.
Some of Dr. Corkum’s current studies:
Pediatric Sleep Knowledge, Attitudes, and Beliefs
Did you know that there are no well-developed, validated measures to assess healthcare providers’ pediatric sleep knowledge, attitudes, and beliefs? Help us develop one by testing your pediatric sleep knowledge today!
This study will involve completing a survey about your pediatric sleep knowledge, attitudes, and beliefs at two time points. It should take about 15 minutes to participate at each timepoint. Once you finish the survey, you will be contacted again in one month to complete the survey again. After completing the survey for a second time, you will receive the correct answers, as well as access to the first version of the Promoting Healthy Sleep for Early Childhood online training program for healthcare providers, once it has been developed.
To be eligible for this study, individuals must:
- Be a licensed healthcare provider practicing in Canada (e.g., physician, psychologist, nurse, or other allied health professional)
- Have current clinical experience working with young children (under the age of 5 years) at least some of the time
If you are interested in participating, please follow the link below to review and complete a Screening Questionnaire to determine your eligibility: https://redcap.its.dal.ca/surveys/?s=AXENE3YXNA9DCM4L
Develop and Validate the Insomnia Knowledge, Attitudes, Beliefs, and Practices (iKAB-P) Questionnaire
You are invited to participate in a sleep expert panel to assess the content validity of the initial draft of the iKAB-P questionnaire for adults aged 18-64 years old. Please also share this invitation to anyone who you think may be interested in participating!
As a part of the development and validation of the questionnaire, we are requesting your expertise to estimate the content validity of the draft. This is an exciting study as there are currently no validated KAB-P tools for insomnia for Canadian adults!
The inclusion criteria to be eligible to be apart of the sleep expert panel includes:
- Currently live and work in Canada
- Experts who have 3+ years' experience in working with adults with insomnia/insomnia symptoms. Experts include academics (i.e., clinical or research appointment at a university) and healthcare providers who assess and/or treat patients with insomnia
- Those who have expertise in the development and validation of any aspect of sleep measures (i.e., published peer-reviewed development and validation studies)
- Experts who have at least five years’ experience in working with adults with insomnia/insomnia symptoms
If you are interested in learning more, please go to https://redcap.its.dal.ca/surveys/?s=FXT3W8WPYAYCLM44
“Najimpay”: Gathering Indigenous Adult Perspectives on Sleep through Interviews in Nova Scotia
Join us for an interview about sleep in Indigenous adults! We are conducting individual interviews, and we will as you questions about sleep, sleep habits, sleep challenges, and sleep education/intervention.
To be eligible for this study, individuals must:
- Live in Nova Scotia
- Be aged 20 years or older
- Identify as Indigenous
- Be able to communicate in English or Mi’kmaw
- Be associated with Membertou First Nation or the Mi’kmaw Native Friendship Centre (e.g., be a community member, user of services)
If you are interested in learning more, click the following link: https://redcap.its.dal.ca/surveys/?s=FFJXKK74WXJML3H7
 Natalie Rosen
Natalie RosenAt Dalhousie University, Dr. Natalie Rosen studies sexual health in the context of couples. Many people thought there would be a baby boom during the pandemic – Dr. Rosen explains why this hasn’t happened.
Natalie Rosen
Where are all the babies? When the COVID-19 pandemic started creating lockdowns in March of 2020, the memes were everywhere. The generation that was sure to come from the pandemic baby boom was being given all kinds of names – Coronials! Baby Zoomers! We were all looking forward to making lame jokes in 2033 about these children entering their Quaranteens.
It made some sense that we would think that way – hey, we’re stuck at home with nothing else to do, we’ll probably all bake more cheesecake, learn a new instrument, and make a bunch of babies. But the boom never came. In fact, Canada’s birth rate in 2020 declined by 0.73% from 2019 – continuing a steady trend downward that continues into 2021 (we are projected to decline by 0.74% this year). So what gives?
Dr. Natalie Rosen specializes in couples and sex. Dr. Rosen is a clinical psychologist and an associate professor in the departments of Psychology and Neuroscience, and Obstetrics and Gynecology at Dalhousie University. She and her team are currently in the middle of several longitudinal studies with couples, some of which began before the pandemic. They’re hoping that they get some good data at the end of the studies that can shed light on the impacts of pandemic-related stress on sexual health, particularly for vulnerable groups like new parents. In the meantime, she’s looking at other studies that are just now starting to release data.
“A study published last Spring in the States looked at the impact of COVID on people’s sex lives. What they found was that just over 40% of people said their sex lives had taken a hit and were declining. Just over 40% said it was about the same, and then there was a minority of about 13% who reported that their sex lives had actually improved during the pandemic. I think it’s fair to extrapolate to some extent to Canadians, which means a big chunk of us are experiencing a declines in their sex lives.”
So what happened? Why aren’t people having sex more than ever? Where are all the babies we were promised in the memes? Dr. Rosen says we probably should have known this would be the case.
“I think that was wishful thinking. We actually know that for many people, stress and uncertainty puts quite a damper on mood and desire for sex. Of course, there are lots of individual differences, so not everyone is the same, but for many people stress and uncertainty negatively impact sexuality. Also, when you think about all the young families who have had these extended periods of time with their kids at home – not only is that a stressor, but it’s also interfering with opportunities for sex.”
Dr. Rosen’s research focuses on sexual dysfunction from a couples’ perspective. In the past, much of the research has focused on the person with the problem – but of course many sexual problems exist within the context of the couple, and she says that very often the other person in the relationship really wants to be involved and to do something differently in order to help their partner and improve their sex lives. Dr. Rosen’s team is hoping to expand the availability of couple-based, empirically supported, treatments available for sexual dysfunction. They have an upcoming publication reporting on a randomized clinical trial for the results of a novel couple therapy vs. a medical intervention for pain experienced during sex, and they are hoping to do the same with low desire. They’ve just launched a CIHR-funded study into couple therapy when women have low sexual desire.
Dr. Rosen’s clinical work is small. She works with a few couples each week who have sexual problems, such as pain during sex and low desire, and with couples who are going through major life transitions, like becoming new parents. In the beginning of the pandemic she paused her practice because it was impossible to meet in-person, but Halifax is doing well enough that she was able to start seeing couples in person again last Fall. She says that some of the couples she sees have adapted to virtual sessions and now prefer that, so going forward it looks like her clinical practice will be the kind of hybrid model we might expect to see in most clinical settings post-pandemic.
The biggest disruption for Dr. Rosen is likely the lack of travel – in a typical year she’s on a plane every six weeks or so, going to an academic conference, or visiting her family in Ottawa or Toronto. She says that now, she hasn’t seen most of her family in over year outside her husband and two children – but that this slowing down of the pace of life has had its benefits.
“For us it’s been a kind of investment in the nuclear family, spending lots of time just the four of us. And we’ve also had the chance to really explore a lot of the nooks and crannies of Nova Scotia! I also find that it’s forced me to take a step back and evaluate what’s important to me. I can get caught up in the minutia of my work, and particularly early in the pandemic I felt the frustration of trying to find work-life balance with two young kids at home. But you take a deep breath, and you figure out your values - health, family, happiness. I care about my work a lot, but there’s a pandemic, and there are many times when it just can’t be the number one priority!”
People across Canada are re-evaluating their priorities and have been for almost a year now. Like Dr. Rosen and her family, they are finding ways to support one another, to balance work and home life, and to stay as healthy and happy as they can throughout. Dr. Rosen emphasizes that finding ways to prioritize and connect sexually with your partner has many benefits for health and well- being. And that’s a valuable thing to do – just don’t feel like you have to live up to the memes of March!
 Keturah Whitehurst
Keturah WhitehurstA mentor to countless black psychologists, Keturah Whitehurst’s contributions to psychology extend beyond her own work to the work of her protégés that continues today.
Keturah Whitehurst was the first African-American woman to intern at the Harvard Psychological Clinic, and the first Black psychologist to be licensed in Virginia. She created the first counseling service at Virginia State College.

She received her Master's from the historically Black research university Howard in the 40s, and a PhD from Radcliffe in the 50s. She was a mentor to many future leaders in Black psychology - notably Aubrey Perry, who was the first Black person to graduate with a PhD in psychology from Florida State.
Dr. Whitehurst died in 2000, at the age of 88.
Photo from Kirsten's Psychology Blog
