Psychology is rooted in science that seeks to understand our thoughts, feelings and actions. It is also a broad field – some psychology professionals develop and test theories through basic research; while others work to help individuals, organizations, and communities better function; still others are both researchers and practitioners.
Profiles
Psychology Month Profile: Dr. Jim Cresswell and Dr. Thomas Teo, History and Philosophy of psychology

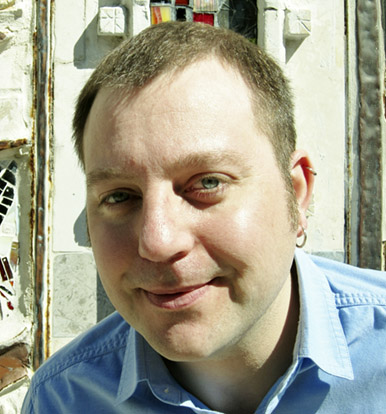
Dr. Jim Cresswell

Dr. Thomas Teo
Dr. Jim Cresswell and Dr. Thomas Teo, History and Philosophy of Psychology
The History and Philosophy of psychology is long, broad, and a truly enormous field of study. A lot of it involves ‘big-picture’ thinking. We spoke to Dr. Jim Cresswell and Dr. Thomas Teo about how they see the ‘big picture’.
History and Philosophy of Psychology
“Think about zombie movies and zombie shows – zombies are literally subhuman. You can kill a zombie, you can mistreat it completely, they don’t have any rights. In fact, you have a duty to kill a zombie because they’ll take our way of life away.”
Dr. Thomas Teo is a faculty member in the Historical Theoretical and Critical Studies of Psychology program at York University. He has been active in the advancement of theoretical, critical, and historical psychology throughout his professional career. He started out with an interest in the history of racism, worked on the relationship between psychology and racism, and on the question of the degree to which scientific psychology can be a form of violence – which Dr. Teo refers to as ‘epistemological violence’ (epistemology is the branch of philosophy concerned with knowledge). Recently, he has been studying the re-emergence of ‘fascist subjectivity’, based on subhumanism and racism, and the idea of cultural supremacy that we can find in the West.
“Whereas racism can be based to a certain degree on science, for instance using numbers and graphs, the notion of people being subhuman can’t be. Subhumanism - think about zombies - is strictly a visual ontology [the branch of philosophy dealing with the nature of being]. You just “see” and know what a zombie is and you don’t need a scientific explanation for that. And it is like this for some people when they see, say, migrants coming to the border. They run, the “caravan”, they walk on foot with suitcases through snow to the border, to a place where they can’t gain “regular” access. It appears to be “abnormal” behaviour, deviant from how ‘regular’ Americans or Canadians behave,. It shows visually that ‘they’ are not like ‘us’, that that are a class of subhumans. You can mistreat them, separate them from their families, throw them into cages.”
Dr. Teo suggests that, in fact, throwing them into those cages is a way to make them appear even more ‘subhuman’ to the general public. This stems from a long tradition of dehumanizing other people by portraying them as filthy, parasitic, dishevelled and desperate. Which is exactly how migrants will look after being kept in cages at the border without showers or soap or decent food, for weeks or months on end. He goes on,
“I’m basing this argument on two sources, one of whom is an American writer [Lothrop Stoddard] who wrote about the ‘underman’ which included ‘inferior races’, poor people, communists and Bolsheviks. The second source is an education manual by the SS in Nazi Germany that published a booklet with the actual title ‘Subhuman’. There was very little text; they just used pictures that contrasted human with subhumans: German versus Soviet soldiers; proper German versus Jewish mother; German versus degenerate art. It’s all visual, we can see that the ‘subhuman’ doesn’t have the characteristics of a full human being. They look to be in shambles, dirty, disorganized. It also means that anyone can become a subhuman. Not just Blacks and Jews but anyone who is an enemy of Germany – Churchill and Roosevelt were included. The concept of the ‘subhuman’ is a very malleable concept. This concept of the ‘subhuman’ does not just mean that you’re less than others, it also means there is an imperative to do something about you. If you are a parasite, a cockroach, a rat, “I” have to exterminate you or remove you.”
Dr. Teo speaks a lot about ‘subjectivity’, suggesting the field of psychology needs to focus in this area a little more in order to make sense of the enormous amount of information we have gleaned from empirical studies over the decades. For example,
“We divided subjectivity into thinking, feeling, and willing. Then we divided thinking into attention, perception, cognition and memory. Memory can be divided into short-term, long-term, episodic memory. Then you look at how one small aspect in a subdivision of a subdivision relates to another small aspect. And it’s very difficult to relate this back to the whole, to a first-person perspective (subjectivity)”
Looking at the big picture is a mantra of those who work in the area of history, theory, and philosophy of psychology. Dr. Jim Cresswell is a professor at Ambrose University, and the Chair of the CPA’s History and Philosophy Section. In addition to his work in history and theory, his areas of expertise are social and cultural psychology, and immigration and adjustment in the context of community-based research. He too talks about the necessity of looking at the bigger picture.
“Psychology as a discipline is having to grapple with post-colonialism, which means talking about subtle but ubiquitous systemic biases against marginalized people of all sorts. We don’t exactly have the cleanest track record in psychology, and a lot of that has to do with the fact that we don’t have a lot of training in thinking about what our theories mean in terms of big picture issues like systematic discrimination. We’re often focused on supporting the individual and doing empirical work in the present moment, but psychologists find themselves in a kind of cultural milieu where a focus ‘just on what the science or data say’ about the individual is not cutting it like it used to. We need to grapple with how and why our empirical efforts worked really well for certain populations, but quite badly for others.”
Although these interviews were conducted several months ago, a lot of what Dr. Cresswell and Dr. Teo said at the time resonates particularly loudly today, especially for those ‘other’ populations who are having a pretty bad time with the recent abhorrent invasion of the Ukraine by Vladimir Putin, and the fascist-style propaganda and disinformation campaigns that have accompanied it. Dr. Teo describes ‘fascist subjectivity’ this way:
“You can have fascist politics with authoritarianism and disinformation and propaganda, and so on. Fascist subjectivity is an individual dimension. If I believe that wealth should not be shared with ‘the other’, and I provide racist or sub-human arguments or feelings for that, then I am entering fascist subjectivity. It is based on the idea that wealth should exclude ‘the other’ or that wealth can be extracted from ‘the other’. In classic fascist subjectivity I can go into other countries and extract wealth from ‘these people’ because they are inferior, they are sub-human, they are parasites. They even can be exterminated if they become a burden”
The global pandemic of the past two years is another example of society’s attitude toward human life. Dr. Teo makes a distinction between those who are dehumanized to the point where extermination is no big deal, and those who are dehumanized to the point where their deaths are no big deal – though the two are clearly two sides of the same coin.
“We have ideas about ‘kill-ability’ and ‘die-ability’. In classical Nazism, Jews are killable, so are Gypsys and homosexuals and enemies, and so forth. Because they are inferior races, or sub-human, they don’t have the same status that we have and there’s no problem with killing them. Die-ability is a more interesting concept, because it moves us from a more classical fascist subjectivity to its re-emergence in our time, where it applies also to liberal democracies. We have debates in this culture, especially during the pandemic, where people say the elderly might be die-able, people with pre-existing medical conditions might be die-able, people in prison and precarious workers are die-able. People have provided economic arguments for the die-ability of many of their fellow citizens: ‘If you want to maintain your way of life, and our economy, then we have to accept that certain people will die.’
In Canada, we have seen that for a long time. Indigenous people were considered killable, and an argument could be made that in many parts of the States Black people are still understood as killable, without consequences. Currently, in liberal democracies we really need to discuss the problem and reality of die-ability, the softer version of kill-ability in a fascist subjectivity.”
That subjectivity – based on a philosophy of big-picture thinking and overarching theories that attempt to connect a variety of schools of thought to one another – is not new. Dr. Cresswell says that psychology in its early years started out with a keen focus on subjectivity, but has drifted over the past century away from this kind of big-picture thinking. Only recently has a concerted effort been made to meaningfully bring this philosophy back into psychology.
“Early psychologists, James, Hall, and Piaget – to name a few – were about 100 years ahead of their time in terms of thinking about topics such as subjectivity, research, and pluralism. Behaviourism and cognitivism that came later moved away from some of that early thinking, which was broader and more systematic. When you go back and look at some of these early writers, you find a lot that’s pertinent to the discipline of psychology’s current context.
Psychologists in the 20th century largely focused on empirical work and shifted away from the theory that underlies that empirical work. The cultural turn started in the 90s brought about a conversation concerning the possibility that our work could be ethnocentric. The result is a recent shift where we’re now starting to pay attention to the theory that informs our research and what we think our observations mean.”
Although not ‘philosophers’ by the strictest definition, both Dr. Teo and Dr. Cresswell certainly speak more philosophically than do most psychologists. As students of history, they are also students of the evolving philosophy that informs the discipline today. As with big-picture thinking, Dr. Cresswell says that philosophical thinking in the realm of psychology started more than a century ago.
“It’s probably more accurate to look at figures such as Sigmund Freud, or William James, as theorists who outlined presuppositions about how to examine the world. In contrast, consider how first- and second-year textbooks will talk about them as researchers who have been disproven in the progress of science. We tell students that they can move on past them without raising questions about what counts as science according to whom it counts. This message is a bit of a problematic stance to take. If you take cognitive theory and examine behaviourism or psychoanalysis from your cognitive paradigm, behaviourism or psychoanalysis will always be ‘disproven’. If you look at cognitive theory through a lens of behaviourism or psychoanalysis, cognitive theory will always fail. My point is that we have to teach students to deal with background paradigms that set the conditions for our empirical work. So when a textbook says we’ve moved on past this or that, they’re actually missing the fact that psychology doesn’t have a clear progressive development as a unified discipline. We actually have multiple disciplines within it and we have to recognize there are different paradigms, which means training students on how to think about history and theory.”
There has been an uptick in interest of late to go back to some of the periods where these ideas rose to prominence – particularly, the turn of the 20th century, the 1960s, and the 1990s. I know, thinking of the 1990s in terms of ‘history’ might be a little disconcerting for some. Like, Alanis Morisette released Jagged Little Pill just a few months ago, right? (It was in fact 26 years ago today that she won a Grammy for that album. She is now 47.) Dr. Cresswell says that yes, indeed the 1990s are part of history.
“Consider Wilhelm Wundt, who’s credited with structuralism and the creation of the first psychological laboratory. Half of his work was about völkerpsychologie, which is basically the ‘psychology of the community and people’. There is value in going back to such cultural theory. Another body of literature that we see in history and philosophy today is the continental critiques and philosophy. People like Foucault and the phenomenologists who partly enabled a birth of post-colonial thinking that largely happened worked outside the discipline of psychology, but there is value in understanding such theory in a milieu where we have to grapple with systematic injustice.”
The field of psychology is remembering, and learning from, its own history. Something we as a society should probably be doing a lot more as well. I’m reminded of another historic moment in pop culture, also from the 1990s – 1994, to be precise. A protest song released in memory of Johnathan Ball and Tim Parry, two men who were killed in the Warrington bombings carried out by the IRA the previous year.
“But you see, it's not me
It's not my family
In your head, in your head, they are fighting
With their tanks, and their bombs
And their bombs, and their guns
In your head, in your head they are crying”
- The Cranberries, Zombie

Dr. Veronica Hutchings

Dr. Reagan Gale

Charlene Bradford
Dr. Veronica Hutchings, Charlene Bradford, and Dr. Reagan Gale, Rural and Northern Psychology
There are unique challenges that come with living in small communities – especially those far in the north. Being a psychologist in these areas brings unique challenges as well. We spoke to Dr. Veronica Hutchings, Charlene Bradford, and Dr. Reagan Gale about their work in Yukon and Newfoundland.
“Cops probably have it really easy in a small town.
Cop: ‘can you describe who mugged you?’
Victim: ‘yeah, he was about 5’10”…’
Cop: ‘uh-huh’
Victim: ‘he was wearing a brown coat…’
Cop: ‘uh-huh’
Victim: ‘and he was…Jim.’”
I’m paraphrasing a comedy sketch I once heard by a Canadian comedian on Just For Laughs. Who it was and when the routine took place have proven to be un-Googleable! I remember thinking at the time, yeah – but it must be pretty tough on the cop too. The victim knows Jim, because he knows everyone in the town, but it must be the same for the police officer, who also knows Jim. So it is with psychologists who work in rural and northern settings
Dr. Veronica Hutchings is a Psychologist at Counselling and Psychological Services at the Grenfell Campus of Memorial University on the West Coast of Newfoundland and Labrador. She is also an Associate Professor cross-appointed to the faculties of medicine and psychology. Dr. Hutchings is currently the Chair of the Rural and Northern Psychology Section of the CPA.
“Burnout is a big thing in rural areas, when you look at the dual relationships and the boundary challenges you’re faced with in small communities. Imagine your waitlist is getting long, and you’re in a small place where people know you’re the only psychologist or maybe one of a handful. You end up with a lot of pressure – ‘can you take this person on, they’re really struggling, can you squeeze in one more?’ Dealing with that can take a toll on you. I do all my work here on the Grenfell campus, and half the stores I go to the workers are my students. I was in Halifax ten years, and in that time I think I ran into a client only twice!”
There are other challenges to providing service in rural and remote communities, one of which – especially now during the pandemic – is internet access. Ms. Charlene Bradford is a registered psychologist – registered in Alberta, operating at a private practice in Yukon. Ms. Bradford is the President of the Psychological Society of the Yukon.
“In the Yukon we definitely have internet issues, it’s a common complaint. We have really expensive internet, and in the communities more north of us it’s very spotty. You really wouldn’t want to do a lot of forms of therapy virtually because there’s going to be a lot of lag time, or the screen is going to freeze and you’ll lose someone at the wrong time. When the pandemic hit and we started to do things virtually, I was doing some training on how to provide therapy virtually and I thought – sure, that’s going to work here in Whitehorse where the internet connections can handle that, but there’s no way in the rural communities that I would trust the internet to be reliable.
We’re lucky in Yukon that we have a really amazing airline that hits quite a few of our northern communities regularly, so there’s a lot of fly-ins happening. This helps, but you also have to have clinicians who are able to travel.”
Dr. Hutchings says that some communities in Labrador have the same internet issues. Both in Newfoundland and the Yukon, some small communities closed their doors entirely so there could be no fly-in psychological services. Ms. Bradford saw small communities get hit really hard with the virus which she describes as ‘devastating’. The pandemic had already created a massive demand and very long wait times, and communities getting hit really hard by COVID only increased the need for psychological help.
The pandemic, and the small size of the communities where psychologists work in rural and northern settings, are just two of the ways psychologists operate differently than they do in urban areas. Dr. Reagan Gale is the Director of Psychology for the Government of Yukon. She is registered to practice in Alberta, the Northwest Territories, Nunavut, and Ontario, and is currently the vice-president of the Psychological Society of the Yukon.
“I grew up in Ontario, and one thing I’ll say since coming to the north is that I’ve noticed the necessary emphasis on cultural safety and ways of knowing and ways of understanding for Indigenous people becomes even more crucial as you move north, and as you work in some of the smaller communities in other provinces where we see a greater proportion of First Nations, Inuit, and Metis people.
I do think there’s a different skill set, a different way of being flexible in helping the people we see. I’m just traveling back through Ontario from a week doing assessments in a community where food security is a profound issue, where children are consistently hungry. While I’m sure that’s the case for many in urban settings, in a small community we’re talking about a cultural norm of hunger. It’s not aberrant or an outlier, it’s the community norm that children are hungry. It calls on us as clinicians to approach practice differently.”
You may have noticed that both Ms. Bradford and Dr. Gale are ‘registered to practice in Alberta’, even though they both operate in Yukon. This is because Yukon is the only province or territory in Canada where psychologists have yet to have any kind of regulation. Says Dr. Gale,
“The Yukon is the last Canadian jurisdiction where anything goes with respect to professional psychological practice, in the absence of regulation.”
If a psychologist in the Yukon wants to be regulated (and many do) they must do so with a provincial body outside their jurisdiction. Ms. Bradford says that while this is a partial solution, it doesn’t address some fundamental issues associated with Yukon’s lack of regulation.
“We do not have a regulation college of any form in the Yukon, so many of us who are practicing as psychologists have taken it upon ourselves to regulate in another jurisdiction. It’s great, because we’re going through the regulation process, but it’s also problematic because there isn’t any regulation in the Yukon which means a few things. One, the colleges we’re regulated with have a limited ability to enforce anything outside their jurisdiction – which the Yukon is. And the other problem is that we do have people who are practicing as psychologists who are not actually regulated anywhere in Canada, and they can do that because it’s not a restricted title here.”
There are a lot of things that might happen when folks who aren’t needing to adhere to particular standards of practice can call themselves psychologists. Maybe they haven’t met the criteria to enter the profession in another territory. There are sensitive and important functions a psychologist performs, like diagnostic assessments. It’s hard to think about what process might look like for clients, many of whom are quite vulnerable, when those are performed by someone without the proper qualifications. Dr. Gale sees this often in her job.
“In my role as the Director of Psychology for the Yukon government, I’ve had people call me and ask about practice opportunities in Yukon. This is often because they’ve failed the entrance requirements to enter the profession in another jurisdiction. Maybe they’ve written the EPPP (Examination for Professional Practice in Psychology) the maximum number of allotted times and have not been able to pass, so they can’t access regulation in the jurisdiction in which they reside. I have also been approached by clinicians who have been disciplined by their regulator, and who might lose their right to practice as a ‘psychologist’ altogether. Yukon is the only spot where there is no prohibition whatsoever on that type of practice.”
So how can this be fixed? And why is the Yukon the last jurisdiction in Canada to adopt regulation? Ms. Bradford says the other two territories have a system they would like to replicate in Yukon.
“The Northwest Territories and Nunavut have an agreement with the College of Alberta Psychologists who do the regulation piece for them. We would like something like that in Yukon, and there are a lot of great reasons for it. One of the big ones being that we’re a small jurisdiction. Regulation really protects people. If things aren’t going well with your psychologist, or something seems dodgy, there’s a complaints process. With a small community you want to know that when you’re making those complaints you want to know they’re not going to your friend, your neighbour, someone you see at the grocery store [like Jim]. With a larger college it offers that protection for people in smaller jurisdictions like ours. This is the model we’re trying to go with.”
The Psychological Society of Yukon is very small, in that it consists of only twelve members – psychologists who have formed a group to collaborate and advocate for the things that are important to them. Says Dr. Gale,
“The society is committed to advocating for evidence-informed high-quality psychological services to be available to Yukoners, many of whom live in remote northern communities. I mean, Whitehorse is northern and rural for much of Canada, but we’re talking about much smaller communities than Whitehorse. The other goal is to advocate for regulation. I don’t want to speak for all twelve members of the society, but we are open to whatever path is going to be most sustainable for our Department of Community Services, which is the government branch that holds the responsibility. Speaking personally, I think we’re too small a group to self-regulate. My personal preference would be to enter into an agreement with a southern jurisdiction. But however the government can make it happen, we want to partner with them to do it.”
Ms. Bradford recalls a memorable moment in the Yukon House – yes, there are debates in the Yukon legislature that, though not well-known to the rest of Canada, can be memorable!
“The leader of the opposition was interviewing the person who’s kind of supposed to be regulating psychologists. He said ‘my understanding is that in the absence of regulation I can put up my own shingle that says Currie’s psychological services, is that correct?’ The minister in charge said ‘yes, that’s my understanding’.”
The issue of regulation is twofold. Psychologists are regulated because it creates a standard of practice, which ensures that psychologists who are providing services to people in rural and northern communities are doing so in an evidence-based way. That they will be guided by professional standards that, at the very least, try not to harm the people with whom they are working. The second benefit of regulation is that it creates a complaints mechanism, so that people who are harmed by the services provided have a recourse, and a process to follow. Regulation can’t prevent all harm, but it does provide a set of rules that minimize the potential harm. Ms. Bradford says it should be a pretty easy problem to solve.
“From our perspective, there isn’t a lot of reason why this shouldn’t go forward. Reagan did some consultation with legal representatives about what is the easiest way to move this along, and it really can be as simple as a memorandum of understanding with the College of Alberta Psychologists. Our understanding is this is simply an order in council from the government.”
And yet, it has not yet happened. Dr. Gale explains a little more.
“The barriers are the normal barriers to the government making law. It’s a small government in a small jurisdiction. The members of our society are grateful for the licensing work the government already does. This is not to criticize the important regulatory efforts that are already under way – it’s just that in such a small area, the human resource capacity to add in another profession is an ask. We think it isn’t a big ask, but any time you expand what a government is offering, it’s a political decision. We had some success lobbying during the territorial election in the spring of 2021, and all three parties made commitments toward psychological regulation, but it was the party that had the vaguest level of commitment that ended up forming the government. But we are fortunate in that both other parties are interested, and the topic of regulation is coming up in the house.”
One of the additional downstream benefits of regulation is stability. Ms. Bradford has been in the Yukon for 19 years (not all as a registered psychologist), and in that time she has seen a real change in the mental health landscape of the territory.
“People who are operating as psychologists in Yukon, who are regulated, have been here for a while. We’re invested in the community, there’s that continuity of services, and a relationship of trust that has a chance to build up over the years as people see the same person. In the past there was quite a bit of turnover, when you had people operating in some of these mental health positions who perhaps didn’t have the same level of education or knowledge in terms of being able to cope with what’s happening. They maybe didn’t have the same kind of emphasis that psychology has on self-care and avoiding burnout. So I’ve really noticed that shift as there are now more psychologists, and people are staying, turnover is reduced and services are getting stronger.”
This kind of shift to better practices, evidence-based treatment, and stability has occurred in other jurisdictions as well. Dr. Hutchings is the first psychologist ever to work in Counselling and Psychological Services at Grenfell Campus.
“Seven years ago when I came here, there was a push for my predecessor to be replaced by a psychologist because they recognized the importance of psychology. Ten years ago at this campus, there was no intake form, there was no consent process. The clinicians working there were not regulated by an official body. Now what you’re seeing is a process, an informed consent procedure, and a more structured service operating in a regulated framework.”
People in remote communities have different needs than those in small communities, although there are a lot of overlaps. For example, communities that have to have supplies flown in might struggle more with access to food, and that has a significant mental health impact. This means that for psychologists working in these areas, there is definitely no ‘one size fits all’ approach. Statisticians have argued for years of what constitutes ‘rural’ communities, and Dr. Hutchings tries to define what ‘rural’ actually means for psychologists.
“Anything that’s northern is rural, but not everything that’s rural is northern. And there are different levels of rurality of course. For example, Cornerbrook (population roughly 20,000), where I am, is kind of a central hub on the West Coast of Newfoundland. But for any major medical procedure you still have to drive eight hours to St. John’s. It’s kind of subjective, but I define rurality primarily by the size of the community, then also by how far away you are from a more ‘urbanish’ centre.”
Or, maybe put more simply – the more rural you are, the more likely you are to know Jim.

Dr. Stryker Calvez

Dr. David Danto
Dr. Stryker Calvez and Dr. David Danto, Indigenous Peoples’ Psychology
As psychology comes to grips with the need to change practices to welcome Indigenous people and attract Indigenous practitioners, the Indigenous Peoples’ Psychology Section says this will involve many important and difficult conversations. We had one with Dr. Stryker Calvez and Dr. David Danto.
Indigenous Peoples’ Psychology
“A fish is the last to discover water.”
Dr. Stryker Calvez is Michif Métis from the Red River Territory, currently living in Treaty 6 Territory in Saskatoon. He was the Manager of Indigenous Education Initiatives at the University of Saskatchewan and is now the Sr. Manager EDI Strategy and Enablement at Nutrien. Dr. Calvez is also Chair of the CPA’s Indigenous Peoples’ Psychology Section and a longstanding member of CPA/PFC Knowledge Sharing Group/Standing Committee on Reconciliation with Dr. David Danto.
Dr. David Danto is a clinical psychologist by training, and the Head of Psychology at the University of Guelph-Humber. He has been involved in a number of efforts toward Indigenizing and decolonizing psychology, institutions and universities. He is the Past Chair of the Indigenous Peoples’ Psychology section.
Eric Bollman is the Communications Specialist with the Canadian Psychological Association.
This conversation took place November 24th, 2021. Since then, 93 unmarked graves were discovered at a former residential school in Williams Lake, BC. 12 were found in Kamsack, Saskatchewan, and 42 were found in Fort Perry, Saskatchewan.
Eric: I understand there’s some talk around changing the name of the Indigenous Peoples’ Psychology section to better reflect the collaborative nature of the work – to focus more on working with Indigenous people rather than making it exclusively about Indigenous people. What sparked this discussion?
Dr. Calvez: As a group, when the new executive came together about a year ago, we realized we had a community of people who were mostly non-Indigenous. As a community of people who are interested in supporting Indigenous Peoples in Canada, we might have to change how we operate. This meant we really had to think about the mechanisms within the section. The section was originally developed to support the Indigenous psychologists in Canada, to give them a safe space and a platform to have a voice. While that is still our mandate, we also wanted to recognize that there was this growing group of people who wanted to be of service and to provide support. So in that sense we thought the name should really be reflective of this. Rather than being a section of Indigenous people, what we needed to do was work with Indigenous people, and to bring as many people as were willing to do that work together and to create a safe environment where they have everything they need, and can have courageous conversations about what has happened to them and how do you move past those places. So the name change is supposed to be a reflection of the development of a community who want to work with and for Indigenous people. And I think we’re doing that in a good way. We’ve got lots of allies – like David.
Dr. Danto: A few years ago I worked with Stryker on a response to the Truth and Reconciliation Commission Report on behalf of the Canadian Psychological Association and Strong Minds Strong Kids (at the time known as the Psychology Foundation of Canada). What was clear from the attendees and participants in that process was that psychology has not been a great friend overall to Indigenous people historically, and even to this day in many cases. A lot of that is as a result of bringing an external Western perspective and approach to psychopathology, health, concept of the family or personality, that kind of thing, to Indigenous communities. And that’s harmful. It’s a way psychology has harmed people. It has happened in the context of education, research, and applied practice. To try to apply our ethical principles in a way that is equal to all people in this land, we have a responsibility to change those harmful practices and to use approaches that are suitable. We have to ask the question – ‘how can psychology be a good friend to Indigenous people in Canada? How can we be supportive?’ In many cases, I think the answer to that is that we can respect and acknowledge that there are already ways of healing, there’s already wisdom and knowledge that is helpful, that promote resilience and strength and well-being within the communities already. As a person who tries to be supportive in this way, I ask myself what I can do within my profession to encourage that profession to have greater respect for, and greater humility when it comes to Indigenous ways of knowing and healing. It’s not that psychology can’t or shouldn’t be involved, but we need to decentralize the approaches we use, and let the local community guide and lead what needs to be done.
Dr. Calvez: There are 1.7 million Indigenous people in Canada, and 38 million Canadians. (Re)conciliation isn’t necessarily all about Indigenous people. Although the impact of colonization has been borne primarily by Indigenous people, Murray Sinclair say that it has also harmed non-Indigenous people too. So if you think about this movement we have in psychology now, where we’re trying to get to a place where we can support the needs of Indigenous communities across Canada, there are not enough Indigenous psychologists, and not enough people with the right training to support them. So we really do need to work with allies – people who are willing to invest time getting to know and understand the needs of Indigenous communities to operate in a way that’s reflective of their expectations.
Eric: David, you mentioned ‘humility’. Is that the number one thing an ally must have when entering into this space?
Dr. Danto: Everything we learn in psychology is about ways of thinking. We talk about ‘empirical’ evidence – and the word ‘empirical’ has its root in the word ‘empeirikós’ which means known by experience. But so much of the methodology within psychology has evolved in a way to focus on what is objective and what is quantifiable objectively. That’s not a bad thing, but when we’re talking about human experience, it is an abstraction from experience. ‘Empirical’ has come to mean ‘quantitative’, and it’s not the same thing. Empirical really means within experience, and when we quantify things we’re really taking it a step away from that description of experience. That’s a very Western way of doing things. We have a respect for certain kinds of research in psychology that may not be a good fit with cultural understandings and experiences of history. So sometimes those Western approaches to knowledge get us stuck in a rut, I think, that makes us think these are the only ways of knowing that are worthwhile, testable, verifiable, and conclusive. And that means that we have lost our humility when it comes to other ways of knowing that seem to be a lower standard of knowledge. That sets us up for wanting to do only certain kinds of research within contexts where that doesn’t fit so well. When we go into communities and make use of these methods that don’t fit so well, we lose the connection with the participants in that research. Then we take our information and make use of it in our esteemed academic way, and it never comes back to the community, the community never has a chance to provide feedback because it’s not in their language. It’s not participatory or collaborative, it’s top down. And you end up with exactly the situation we have. Communities that don’t trust academics and researchers in their community, because they’re taking one more thing from the community. You know, we’ve taken land, we’ve taken rights, and now we’re taking knowledge and for who? For the sake of the university, and the researcher, not for the well-being of the community. I think humility is so important to have the approach that there’s lots of ways knowing things, and if you can take a back seat and acknowledge that your training really limits the possibilities that can be seen, rather than illuminate those possibilities – which is what those methods are supposed to be doing!
Dr. Calvez: The other element of cultural humility is that Western education and knowledge comes from a dominant position. The whole hierarchical structure of the Western world is structured in a way that one dominates another based on their education levels, or their cultural group. And that’s embedded within our paradigm of seeing the world. Cultural humility is a process through which we start to recognize that and counteract it. We need to unpack this as part of decolonization, and cultural humility gives us the tools to do that.
What might be more important than humility is commitment. This process of (re)conciliation is going to take an enormous amount of effort and it’s going to create tensions. Unless you have commitment to see things through to the conclusion of what we’re trying to do, to create a healing for Indigenous and non-Indigenous people and to the field of psychology, we can’t do that unless people are committed to go through with those intentions.
Eric: Do you ever try to recruit more people to participate in this (re)conciliation, to become allies, or are you more focused on creating a space where those allies can learn and grow alongside Indigenous people?
Dr. Calvez: An important thing about (re)conciliation is that people need to find it within themselves. The starting point isn’t knowing the issues and how to deal with them, the starting point is knowing yourself. And knowing yourself in relation to Indigenous people and the history that’s been here for thousands and thousands of years. That’s something people need to find on their own terms. Rather than promotion [reaching out to people to recruit them to become allies] it should be about attraction [creating a space where people want to become allies and reach out to you]. What we want to show people is that what we’re doing isn’t necessarily an imperative right, something that has to happen – although I do believe that’s true. What we want to show them is that this is something that’s going to benefit everybody, including our profession. There’s a good way to do this so we all learn from it, we all benefit from it. I think that’s done not by telling people you have to do it but by showing them why they might want to do it. When we get people coming on board because of their own choices, we get people who are much more capable of having the commitment I spoke to earlier, and the cultural humility.
Dr. Danto: Within the post-secondary context, I think the focus needs to be on creating the kind of post-secondary institution that’s welcoming and culturally safe and facilitates an appropriate, reflective and critical education for both non-Indigenous and Indigenous students. Rather than recruitment of Indigenous students. If you focus on asking the right questions and on being self-critical in terms of the processes that are in place, and creating that culturally welcoming safe environment, more people will be inclined to participate in what you’re doing. Indigenous people have had really negative experiences in class in the context of taking psychology courses. There are myths about genetic predispositions, assumptions and prejudices and biases because of the long history of colonization. I always use the expression ‘a fish is the last to discover water’. We are so embedded in this context of colonization, whether it’s psychology or health care or education that even with good intentions it’s very difficult for us to see. We need to do a careful examination of those spaces into which we’re inviting Indigenous people, because they may well be places where they’re exposed to re-traumatizing kinds of experiences as they’re confronted with incorrect, outdated, or unfair kinds of comments. We have a responsibility to be protective.
Dr. Calvez: When your focus is just on recruiting people in because you want more Indigenous people in your program, that’s self-serving. It’s not about Indigenous people, their needs, or what they want. If that’s your approach to supporting Indigenous people it will fail every time. We need to change the environment so Indigenous people see it as an attractive and desirable place to land. Let’s be clear – Indigenous communities have just as much need for people who are professionals in mental health as the rest of society does. We have to put the work in now, without knowing for certain that we’re going to attract those people in – just because it’s the right thing to do as a community and as a profession. I think we are moving in that direction. We’ve seen a lot of change in the last few years. That’s going to have to continue and accelerate in order to increase peoples’ interest in this work. Once they are interested, they’re going to realize that we’re not hampering anything that already exists within the profession – if anything, we’re expanding the possibilities and creating a bigger and more open space for more people to find what they’re looking for in the profession.
Eric: There have been some horrific discoveries in the past two years of mass graves at the sites of former residential schools. I think this has come as much more of a shock to white Canadians than it has to Indigenous communities who have been telling us for years that these existed. Is that true, and has it changed how you go about striving for (re)conciliation?
Dr. Calvez: I think it’s really important to recognize that when these events happen they’re really re-traumatizing to Indigenous Peoples. We’re highly affected because this is a confirmation of what we’ve been advocating for a long time. That Canadian society has not treated us right, and that they’ve actually gone to the point of harming and killing children to prove it true. That is the most horrific experience you can have as a person who comes from these communities, to know that even your children aren’t safe. I have friends who are survivors, and when this happens it sucks the wind out of you, and it takes a long time to come back to feeling like you could be okay. That’s happened multiple times this last summer alone. We knew it was bad, but I don’t thinks we knew the magnitude of it all. I very much appreciate that non-Indigenous people are having a reaction to something they didn’t know about. Having that reaction is the right thing – you probably should. But when you impose that reaction on Indigenous people to help them cope with it, that’s not necessarily the right thing to happen. We need other people to be standing up and speaking out so that we don’t necessarily have to be front and centre while we try to heal. This is where we’re moving as a profession. We should be able to advocate while recognizing you don’t go to the people who have been harmed to get support for your reaction. It’s an emerging process, and we’re new to all of this. That’s what (re)conciliation is, it’s a new idea that we’ve never seen before or had before. We’re going to have to discover it and build it from our experiences and our understanding. I think the outrage you’ve seen from both Indigenous and non-Indigenous communities shows us that we’re moving in the right direction because now there’s an awareness and an appropriate response where people are extremely upset. We’re moving in the right direction in that we’re now trying to support each other in those processes. I think this is a strong time for us as a community and as a society. There are a lot of tensions we’re going to have to navigate as more revelations come forward and we experience this more and more. Most important are the conversations we’re going to have around these and other issues – and they’re going to get difficult. We need to be prepared to have those conversations both as a profession and as an individual.
Dr. Danto: My personal view is that a genocide has happened against Indigenous people in this country. Not a ‘cultural genocide’. A genocide. We are finding bodies at the sites of these residential schools, and there’s little doubt that many more remains will be found, and that no matter how many are found many more will not. As a person who is not Indigenous, recognizing that this occurred in this country – that the killing of Indigenous people in large numbers because of who they are occurred in this country. If we don’t want to admit that, we have to ask ourselves why we don’t want to. To me it is clear that is what has happened. In order to move forward, that’s part of truth. There’s a responsibility when you name something, to act on it.
Eric: Why is it that people use the term ‘cultural genocide’ when it seems quite obvious that what has happened is an actual genocide? Is it a way of minimizing the damage done, or of using a term that doesn’t require as much soul-searching of themselves, or is it something else?
Dr. Danto: The story of the residential school system in Canada was always about ‘saving’ the child while destroying the Indigenous aspect of them. Severing the cultural ties to their community and family. While that may have been the stated objective of the residential school system, and of forced adoption initiatives, much more than that was done. Many people lost their lives within that system, and within those federal government funded (and in many cases church-run) institutions, many children lost their lives. There’s no doubt about who bears responsibility for that. Calling it merely a ’cultural genocide’ is choosing to define the harms that were done in terms of their intention, rather than the outcome. We wouldn’t do that in a court of law. If your intention was to harass but not kill, and you ended up killing, you wouldn’t just get the harassment charge.
Dr. Calvez: We have to recognize that Canada as a society is just now coming to terms with what it’s done. As a stepping stone, ‘cultural genocide’ was the thing they did. They were still in this belief that residential schools could have possibly been a benefit to Indigenous children. I think that now that we’re seeing how untrue that was, people are going to come to terms with the fact that it was more than just a ‘cultural’ genocide, that it was purely genocidal. That said, I don’t dismiss the malevolence of cultural genocide itself. I am who I am because of my ancestry, my beliefs, my identity, because everything I’ve ever been is tied to the land. So to take away my world views, beliefs, and everything else, is to leave me with nothing. Although I’d physically be there I would be a stranger in my own body. It was a significant step forward to use the term cultural genocide, but we’ve now become more articulate. We’ve understood the truths that surround it, and we can call it what it really was, which is a genocide.
Eric: You’ve said that there is progress being made and that we’re moving in the right direction. Can you give me a concrete example of something that is happening now that demonstrates this?
Dr. Calvez: A large group with David and I came up with Psychology’s response to the Truth and Reconciliation Report. Since then, it has not collected dust. What has happened is that we’re seeing this invigorating conversation starting to emerge in different spots in the field of psychology. You’re seeing a change to the ethics standards. The standards are going to change, we’re increasing it and adding a value as well as a practice that will support the Indigenization of psychology and support for (re)conciliation. We’re also seeing CPAP (the Council of Professional Associations of Psychologists) and ACPRO (Association of Canadian Psychology Regulatory Organizations) step up and change the way they want regulatory boards to start addressing these issues. And David will be giving a workshop for the CCPPP (Canadian Council of Professional Psychology Programs) with Ed Sackaney on ‘Allyship, Reconciliation and the Profession of Psychology’. So even within our profession, we are now starting to see an enormous amount of change. It has just begun and the ripples are beginning to be felt across the profession.

Dr. Lindsay McCunn
Dr. John Zelenski
Dr. Lindsay McCunn and Dr. John Zelenski, Environmental Psychology
Environmental psychology has two main branches. We spoke to Dr. Lindsay McCunn about the architectural branch (designing buildings and rooms for the well-being of occupants), and to Dr. John Zelenski about the conservation branch (examining sustainable behaviours through peoples’ connectedness to nature).
“When I say I’m not judging you, I think I really mean ‘not more than other people’.”
I’m a little nervous that, during this Zoom meeting, Dr. Lindsay McCunn and Dr. John Zelenski might be judging my decidedly cluttered Zoom background. All my kitchen appliances are on a shelf behind me, giving the (accurate, it turns out) impression that my home office space is a cramped corner by the kitchen. Dr. McCunn and Dr. Zelenski are environmental psychologists, experts on the spaces we occupy and how we interact with them. Dr. Zelenski is being quite nice, and honest - we as human beings do pick up on these subtle clues based on each others’ spaces, but that is probably not unique to environmental psychologists. We all judge Zoom backgrounds, if only a little bit.
Dr. Lindsay McCunn is a Professor of psychology at Vancouver Island University. She is the Chair of the Environmental Psychology Section of the CPA and the Co-Editor in Chief of the Journal of Environmental Psychology. She says examining peoples’ Zoom backgrounds, or the way they lay out their gardens or living spaces, is a curiosity for all of us.
“The way people express themselves and set up their homes and place meaningful things around is really interesting. Sam Gosling wrote a book called Snoopology, it’s a study of how you can sort of deduce peoples’ personality and thought processes based on how they arrange their trinkets and belongings in their homes and offices.”
Dr. McCunn specializes in Environmental Psychology, and describes it this way.
“Environmental psychology is the study of the transactions between people and place. I mean a lot of different types of places – a coffee shop, an office, a school, a park, an ocean, a mountain. We study the different ways in which people interact with their settings. Much like the way a social psychologist might study and understand relationships and interactions between people and other people, environmental psychologists study and understand the relationships between people and places. In my research, I look at how people interact in communities and work environments, especially hospitals, schools, and offices. In that capacity, I look at staff, mostly, and people who use the environments in different ways than you might expect like students and patients, teachers, and so on.”
Dr. John Zelenski is a Professor at Carleton University in the department of Psychology. He is also an environmental psychologist, but he specializes in a much different area than does Dr. McCunn. One might say they represent the two major branches of environmental psychology – the architectural (Dr. McCunn) and the conservationist (Dr. Zelenski).
“In addition to being an environmental psychologist, I also think of myself as a bit of a personality psychologist and a positive psychologist. I’ve been very interested in what we call nature-relatedness, or what others call ‘connectedness to nature’. It deals with peoples’ subjective impressions – are they a part of nature, or is nature separate from them and something that has little to do with their sense of self? I’ve also been interested broadly in what I call a ‘happy path to sustainability’. That’s the idea that we know that nature is good at putting people in a good mood. Nature is associated with happiness both over long periods of time and also right there in that moment. We know that people who spend a lot of time in nature and feel very connected to it behave in more pro-environmental and sustainable ways. In the last couple of years, we’ve started thinking that maybe the reverse is true as well. That if you could get people to do a couple of nice things for nature, by engaging in some sustainable behaviours, there could be ways to use that to make them feel more connected to nature and also feel happier about these activities. The idea is that doing nice things for the environment doesn’t have to be onerous, that we might be able to link it to positive emotions.”
What ‘spending time in nature’ means to each person is subjective. Maybe it’s taking a weekend to go hiking in the hills, or spending a day ice fishing, or just going into your backyard and tending to your radish garden. For Dr. McCunn, it has meant a big shift since the beginning of the COVID-19 pandemic. She is speaking to us via Zoom from what appears to be a cabin in the woods. She and her family lived in the downtown core of Nanaimo BC for a few years, living across the street from the ambulance service, the police service, and the fire station. Sirens increased significantly when the pandemic began, their sleep patterns began to be affected, and they decided to rent a place in the country.
“It was kind of a good case study in environmental psychology, in that we could realize what was stimulating us in our home environment, and then decide how best to alter that for our mental health. So we thought about moving to a larger natural setting where we can have a little bit more control over the things that stimulate us. We were very lucky to be able to rent something in the country. It was interesting, because I was quite attached to the house that we owned. One of the things we study as environmental psychologists is the ‘sense of place’, or a sense of place attachment/identity/dependence. At the start of the pandemic, I was hearing a lot of questions about how people could address the feelings of loss they had now that they were working from home. Not just feelings of loss in terms of social elements, but also a loss of the habitual ways in which they got to those places. Maybe they took the same bus every day, or stopped at the same coffee shop on their way to class or work. Even physicality of the office environment or the classroom itself – they were missing the setting. So I really wondered how I would react when I moved away from this familiar home environment to which I had become so attached. I didn’t want to put myself in a position of place-loss, but I quickly formed a strong attachment to this place, and the natural features around it. It has been a nice journey to explore environmental psychology from the inside out in this circumstance.”
Feeling close to nature can be as simple as being able to go outside and touch a tree, or look out your window at a mountain or a variety of bird species. So how does this translate into more pro-environmental beahaviours, when climate change has become the most pressing issue of our time? Dr. Zelenski gives an example.
“What we have is a lot of good circumstantial evidence and lab studies and we’re trying to assemble it. There have been a few programs that have been promising! My former student/friend/collaborator Lisa Nisbet has collaborated with the David Suzuki Foundation to do something called the 30 By 30 Challenge. They get people to spend 30 minutes in nature every day for 30 days. The people they get signing up for this tend to be pretty pro-environmental, and pretty connected to nature already. But over the course of this month that connectedness does seem to grow. It’s not a randomized control trial, but it seems like spending that time in nature for these folks does make them feel more connected, and along with that comes more commitment to sustainable behaviours.”
Conservation is a (relatively) new branch of environmental psychology, and has certainly become much bigger in the past twenty years, when climate change has quickly become a top-of-mind subject for so many of us. Dr. Zelenski is not alone in having moved in this direction.
“Just the attention and the amount of notice and importance the conservation side of environmental psychology is receiving seems to have really amped up in the past ten or fifteen years. I came to environmental psychology after my PhD just out of personal interest, and I feel like I’m one of a million people who are jumping on this bandwagon! It’s for a few reasons. People seem to be increasingly exhibiting symptoms of depression, anxiety, and so on – and nature seems to be a nice respite from that. Also the awareness of climate change just keeps growing and growing as we’re seeing the effects more and more. And policy-makers are interested in knowing what social science can contribute to try to solve those problems.”
The conservation branch of the discipline has naturally evolved out of the traditional architectural branch, which has been around since the 60s. Dr. McCunn says that there are a few formalized graduate programs in ‘environmental psychology’ in Canada, but there are more in England and the States, the Netherlands and South America. So when she tells people she’s an ‘environmental psychologist’, they often know what she means.
“Some people – and rightly so – split the field into the architectural psychology side and the conservation psychology side. I do that too if I’m going to clarify with people what it is I study, because I’m more on the architectural side. I work with engineers and facility managers and city planners, whereas other colleagues of mine, like John, work particularly on nature-relatedness and with people who study pro-environmental attitudes and behaviours. This idea of conservation has become very popular for the field of environmental psychology – not that it’s taken over the architectural side that deals with building infrastructure and so on. Really, environmental psychology started in this architectural realm but has very much branched out into this line of inquiry that includes asking people questions about eco-consciousness and how they relate to nature.”
The two branches do go hand-in-hand. Think of the push toward ‘green’ buildings, with energy-efficient heating, solar panels, maybe a garden on the roof. Says Dr. McCunn,
“When engineers ask me ‘should we be designing this building with sustainability in mind,’ they want to know – are people going to notice it? Care about it? And make changes in their behaviours inside (and outside) of the building because of it? I can help them study the ways in which people behave and work and function in buildings that are more (or less) sustainable. I did a study in grad school that showed that just because an office building is ‘green’ or sustainable, doesn’t necessarily mean that it will predict strong productivity or satisfaction. It’s important to be quite critical about what you expect from sustainable design and what you don’t.”
Think of some spaces you’ve been in where you felt instantly comfortable with the people around you – and others where you didn’t. It’s possible that one of the reasons wasn’t the people who were there, but the design of the space that made interaction more awkward, or made that room or building or train car feel more comfortable. Dr. McCunn explains further.
“If you want a certain space to feel homey and comfortable, you might design it for a particular number of people to be there to sit at certain distances. I’m thinking of a coffee shop design or a restaurant or even a classroom where you want people to sit in a certain way and get along in a certain way.
I think it’s important to make use of different methods, much like other psychologists do. We’re good at integrating a variety of mixed methods into our work. We use naturalistic observation to watch, and see how people are moving and behaving in a space in order to make design decisions from there. We do a lot of surveys and interviews and from these we can help architects and designers make the most humane buildings possible. If the point of clinical work, and other types of psychology, is to help people feel well, then environmental psychology is very much aligned with that. We want buildings to be designed in ways that can help people feel as healthy, motivated, enthusiastic and well as possible.”
Dr. Zelenski bridges the two sides of environmental psychology as well, in a number of different ways. Collaborations with groups who are already doing some environmental work makes it easier for him to collect data, and the analysis of that data allows those groups to be more efficient and effective in the way they operate.
“I’ve collaborated with an architect, bridging these two parts of environmental psychology. He was very interested in making buildings that make people want to behave in environmental ways. Also, maybe it’s not just the inside of the building, but what kinds of natural spaces close to the building might encourage that. This is asking a more nuanced question about what kinds of nearby nature might make people feel better, be happier, be more productive.
There’s a small non-profit that provides water testing kits. They distribute them to people and those people go out and test the nearby water quality, then they upload their data to this kind of crowd-sourced database where you can see if the lake or river near you is in good shape or bad shape, and how is it changing over time. It would be hard for me to put together an experiment where I handed out a bunch of water testing kits, but I can try to follow up with the people who are already doing this to see if it’s changing their sense of connection to nature, is it making them happy, and is it making them want to do other nice things for the environment other than just test the water?”
Since the advent of lockdowns as a result of the pandemic, we’re hearing a lot of people saying they’re appreciating nature more. It’s a safe way to get out of the house – if you can’t go to a crowded mall or a concert, you can still go to a park and walk around. People are seeing nature as a source of well-being and coping, and there have been some studies that indicate nature is one of the more positive things people have experienced during these past two years of physical distancing. But this connectedness to nature, along with the awareness of the grave threat posed by climate change, are creating new problems in some ways. Dr. Zelenski says,
“Lots of people are talking about eco-anxiety, where to the extent that people are becoming more aware of climate change it could be a double-edged sword. So it could be motivating – which is a positive outcome, people wanting to behave in a more environmental way – but for some people it might upset or worry them so much that it creates new forms of stress and concern that for some people can be maladaptive.”
One way to combat eco-anxiety, a big new buzzword on the conservation side, is an increased awareness of environmental psychologists and the seeking of their advice. This increased awareness is being felt on the architectural side of things as well, as the contributions of these experts are now seen by many as invaluable. Dr. McCunn says she’s seen this shift first-hand.
“When I come across engineers and architects and facilities planners, they’re more aware of environmental psych and are very willing to work with us. When I was doing my Master’s, I found that very few people in those positions wanted to work with a social scientist. Many said that they did that kind of research off the side of their desk, and that they ‘already knew how to study people’. Now they’re seeking me out, wanting that professional element in their business or in their processes.
Spatial cognition, for example, is very traditional topic in environmental psychology. I think it’s worth noting because the population is aging. Environmental psychologists often consult with designers about how to help people living with dementia navigate a care home, for example. We can observe them and help them with signs and symbols and ways of integrating their psychology into design to make their lives better.”
Have you ever been in a store where there is a very simple pattern on the floor that changes a little as you approach the bathroom, and a little more near the cash? Maybe there are brightly coloured hand rails along the walls, and the toilet seat is a noticeably different colour than the rest of the toilet. It’s brightly lit but not overwhelming because there are few reflective surfaces and no mirrors. A store that looks like this has probably been designed to be accessible to people with dementia, assisted by environmental psychologists.
People with Alzheimer’s Disease and dementia of different types usually work with a team of people that can include a neuroscientist (see the profile of Clinical Neuropsychology from earlier this month). Increasingly, environmental psychologists are working on larger interdisciplinary teams, and neuroscience itself is becoming a larger part of the discipline. Dr. McCunn says she is seeing this thanks to articles submitted to the Journal of Environmental Psychology.
“I see a lot of articles coming up that merge neuroscience with environmental psych. This is something I’m also doing in my own work—I’m almost finished a second Master’s in applied neuroscience just to get my research more involved in the realm of environmental neuroscience. I like trying to understand things like ‘what is happening in the brain when we feel place attachment? Is that different from when we feel attachment to a person? What’s happening in the brain when we encounter different settings?” These are important questions that I think are becoming very popular.”
As environmental psychology is becoming a discipline that is more and more in demand, the expertise of those in the field is being applied to a larger and wider variety of subjects. Dr. McCunn hopes this continues, so that the full skillset of her colleagues can be used to help solve significant problems.
“I want environmental psychology to be a part of lots of different teams. Of course architects and urban planners, but also clinicians, doctors, neuroscience teams, and so on. I think that we’re good team players and we can add facets to research questions that can complete an answer and make it more comprehensive. It’s very difficult to draw conclusions from only a few variables. Getting some big data and modeling going in environmental psych can help us help others get more reliable answers to larger questions in society about what makes people act and think in particular ways. I’d like to see environmental psychology at more tables more often.”
But rest assured – if an environmental psychologists ends up at your table, they are not going to be judging the layout of your silverware or the positioning of the gravy boat next to the jar of Nutella. At least, not more than anyone else would.

Dr. Maria Rogers

Dr. Maria Kokai
Dr. Maria Rogers and Dr. Maria Kokai, Educational and School Psychology
While the terms Educational and School Psychology are sometimes used interchangeably, they can also refer to the two parts of psychology in the education system – the researchers who come up with evidence-based best practices, and the practicing school psychologists who implement that research. Dr. Maria Rogers and Dr. Maria Kokai joined us to explain further.
Educational and School Psychology
“It’s like teaching children how to swim way before they have a chance to fall into deep water.”
Dr. Maria Kokai is a school psychologist who spent 30 years at the Toronto Catholic District School Board, the last 14 as the board’s Chief Psychologist. Now retired, she is now the chair-elect of the CPA’s Educational and School Psychology Section. Over the course of her career, she has seen a shift in the field of school psychology, as it has been moving away from a focus on assessments and dealing with children in crisis toward more of a prevention model, however this move is happening too slowly.
“COVID has really drawn attention to the importance of mental health and addressing it on a regular and consistent basis. It has also shone a light on the inequities that resulted from all the school closures and other consequences. One lesson for us and for schools I think is to make sure that mental health is addressed in a preventative way on a regular and intentional basis – as we did with anti-bullying – so that children learn coping skills, relationship skills, problem-solving. They can then apply these skills in challenging situations (which COVID has been) so they can adapt more easily with less stress.
School psychology across Canada is very different in different places. In some places we have the full range of services school psychologists are capable of providing, and in others there’s a very narrow focus on assessments and problems. What we would like to see in the profession is consistently across the board being able to provide equitable and accessible services to all students regardless of where they live, which province, a city or rural. Everybody should have access to services in an equitable way in the future. We’re not there yet.”
This focus on prevention is something school psychologists are advocating to see across all school boards across Canada. There has been significant progress in this direction over the past decade or so, but there is still a lot of work to do. Dr. Maria Rogers is a professor in the school of psychology at the University of Ottawa. She is the current Chair of the Educational and School Psychology Section at the CPA. She says,
“This really points to larger systemic issues within the field. There are not enough school psychologists, and not enough are coming out of graduate programs in Canada. There aren’t enough resources allocated toward mental health in schools. We really want to move toward a preventative mental health student success approach. There are some boards and districts that are better able (better resourced) to take a preventative approach. But many larger school districts are working under a wait-to-fail approach, which is really unfortunate. There are parallels with our health care system, where we often wait for someone to be really sick instead of taking preventative measures ahead of time.”
Some of the delays in implementing preventative programs stem from a fundamental misunderstanding in the public about what it is school psychologists do. In the minds of many, school psychology is all about testing and psychoeducational assessment. This turns out to be a rather narrow and inaccurate description of school psychology, and of what school psychologists are trained to contribute to the educational system. This idea originates from a much earlier model of school psychology work, one which arose around the mid-20th century. At that time, many schools categorized students based on their abilities and their disabilities, and they required school psychologists to participate in this classification by testing students for their eligibility for various programs. But school psychologists have a much wider range of skills and expertise. And misunderstanding or underutilizing that expertise can deprive students of a wide range of services they could otherwise be receiving. Dr. Kokai explains further.
“A lot of the public still thinks school psychologists deal primarily with students who are having problems. That’s one reason people talk a lot about assessment waitlists which are endless and a constant problem. If school psychologists had the opportunity to focus on preventative measures – mental health prevention, promotion, and early identification and intervention of potential learning and mental health problems – then those severe problems could often be prevented and there would be less need for assessments for severe problems. We advocate for a full range of school psychology services and it is for this reason – shifting the focus from strictly problems to a more preventative approach means we don’t wait for those problems to become more severe.”
Some regions have moved faster than others in focusing on student well-being, and Dr. Kokai points to one place where it is working.
“A good example is an organization called School Mental Health Ontario, which has an advisory role to the ministry of education and a resource to school boards. About a decade ago, the ministry of education in Ontario added student well-being to their goals in addition to student achievement. This meant that schools are now required to focus on student wellness and mental health and also address issues related to mental health. During that decade, a lot of progress has been made in general, and some progress in terms of using the skills of school psychologists to support the prevention and early intervention areas.”
The biggest change in school psychology in the past, say, 30 years is the narrowing of the research-to-practice gap. There has been a larger systematic effort to translate knowledge from researchers to practitioners, to make sure those psychologists and other education professionals who work with children can access research findings and apply this knowledge in evidence-based practices with kids in schools. Dr. Rogers wears both hats, as both a researcher and a practitioner.
“I do research in educational psychology as well as being a practitioner. I think that overall, the research has led us to a deeper understanding of the intersections between children’s mental health and children’s learning. At one time the two constructs would have been considered separate elements. The research has brought those disciplines together to understand how those are inseparable domains of a child’s life. What I’m seeing as well is more of a focus on researchers from around the world working together and learning from one another. We’re pooling data and resources from regions around the world to allow for larger-scale and bigger-picture investigations.”
The difference between ‘educational psychologists’ and ‘school psychologists’ is not quite as simple as the idea that ‘educational’ refers to researchers and ‘school’ refers to practitioners. Some regions in Canada and elsewhere in the world use the terms interchangeably. For the CPA’s Educational and School Psychology Section though, ‘educational – research’ and ‘school – practice’ has become a useful shorthand and is understood well by those in the field. Researchers create the science, practitioners apply it. Dr. Kokai explains,
“School psychology is applying the science of psychology in school settings. School psychologists apply knowledge and expertise in the areas of learning, mental health, behaviour and child development to help all students thrive and become the best they can be. They also connect with and support those who are most important in the children’s lives – parents, teachers, communities. It’s a very collaborative type of work in the interest of our children and youth.”
That collaboration has borne a lot of fruit over the past few decades, as practices change and focuses shift in the goal of best helping students to maintain well-being and thrive in a school setting. Dr. Rogers gives an example.
“Starting in the early 2000s, researchers started to really look at the concept of self-regulation or emotion-regulation. Some researchers started to look at it in a classroom context, and how self-regulation impacts learning. A number of researchers, and more practice-focused people like Stuart Shanker, built curriculums and supports for teachers around understanding self-regulation and how it impacts behaviour. That allowed for an improved understanding for educators.”
Psychologists and researchers have also been involved collaboratively in new methods for teaching children how to read. One of the places where a lot of this work has been done is at Sick Kids in Toronto. When Dr. Kokai was the Chief Psychologist of the Toronto Catholic District School Board, they were one of Sick Kids’ experimental sites. It was a direct link between educational practitioners and researchers. Dr. Rogers was doing her internship at Sick Kids about fifteen years ago when this new program began. She says,
“There has been a tremendous amount of attention in recent years around how we should be teaching children to read. A lot of researchers in Canada, primarily out of Sick Kids, did years of research on phonological processing and reading comprehension. They developed a program called ‘Empower’ which is an extremely rigorous and evidence-based reading remediation program. When I was doing my internship at Sick Kids about fifteen years ago, Empower was just starting to be implemented in schools in Toronto, and now it’s being used in schools across the country and teachers are being trained in the program.”
The influence of science on school psychology is just one part of this large collaborative system. Psychologists of all kinds collaborate and learn from one another. The skills imparted by a school psychologist can be useful for more than just the student. Dr. Kokai recalls assisting families in the context of helping a child.
“If you are a parent, you would use similar communication and behaviour management practices that we would maybe recommend with teachers. How to communicate, how to establish positive relationships with children, to help them become more independent and deal with peer pressure or bullies. Many of these skills very much apply to adults as well. Your relationships in your workplace, your community, and so on.”
Dr. Rogers, who works as a clinical psychologist in addition to her work at the University of Ottawa, sees the influence this kind of collaborative mindset has had on all parts of the discipline.
“One of the things clinical psychology may have learned a little bit from school psychology is this holistic viewpoint of the child within their system. When we’re working with a child in a school psychology setting, we’re working with them in the context of the school environment, or their families, or the educational system as a whole – often all three. Traditionally, clinical psychology tends to be more individual-focused, and there have been some great lessons that have come from schools.”
You have probably seen parents complaining online about the “new math”. The way math is being taught in many schools is changing and many parents, particularly millennial parents, are finding it hard to grasp – what do you mean you’re not carrying the one any more? That’s how I learned and consarn it, it worked for me! (We’re of course referring to millennials who talk like 19th-century prospectors.) There really isn’t a ‘new math’. Math remains the same. 2+2=4. n! is equal to n x (n-1)…1. What has changed is the method in which it is delivered, which puts a greater focus on understanding the concepts than it does on arriving at the correct answer. But the resulting process is different enough that parents and children now have something of a disconnect when trying to work together on math homework. Dr. Kokai says that while researchers have been studying this for a while, as far as she knows psychologists were minimally or not at all involved in the implementation of these new programs.
“This seems to be an example of ‘silos’, that we sometimes talk about in education. In this math silo, psychologists were not involved. What we are trying to do as school psychologists is trying to support students with learning disabilities to help them acquire math skills. But I know that there are researchers here in Ontario and likely elsewhere who are focusing now on math and the basic skills in math. We will have to listen to these scientists and researchers and build a math curriculum that takes those findings into account.”
There are many good reasons to get psychologists involved – in all areas of education, of course, but specifically in math. Dr. Rogers says that “unlike other most other subject areas, there’s a cognitive-psychological aspect to math where you either feel like you’re good at math or you’re not. And that self-perception seems to start very young.” Helping kids through that from a very young age goes right to the heart of the prevention argument – the earlier you can intervene, the better the outcome for the student both emotionally and academically. And the more likely they will be able to swim once the deep water arrives.

Photo: Enje Daniels Photography
Dr. Cranla Warren
Dr. Cranla Warren is the Vice-President of Leadership Development at the Institute for Health and Human Potential. Her professional work focuses on organizational systems, leadership development, and emotional intelligence, and her volunteer work focuses on mentorship for professional women and Black girls.
“You’ve been my therapist since we were 13 years old.”
Dr. Cranla Warren’s lifelong friend reached out to congratulate her on being named one of the Top 100 Accomplished Black Canadian Women for 2022. She said she wasn’t surprised that Dr. Warren was being so honoured, since she had been helping people as long as she could remember. Which included being a de-facto “therapist” for her friends from a very young age. "I never doubted you would be a therapist, as you were mine since I was 13! But now you have helped so many people over the years, whose lives were no doubt changed for having known you."
For Dr. Warren, that passion went beyond simply being a shoulder to cry on, or a sympathetic listening ear. She was the person to whom all her friends came to talk about their struggles or their issues, and she started to actively study what drove and motivated people. She started to read psychology books – there weren’t a lot of them in the 70s, but she read every one she could find. Like books by Dr. Joyce Brothers, one of the very few well-known female psychologists at the time.
“I became a student of human behaviour in my teens, reading everything I could, trying to understand everything that I could. I realized this was the path I wanted to take, but it was a very circuitous route.”
That route started out in social work, moved into psychotherapy, then into business. Through it all, Dr. Warren remained a student of human behaviour, figuring out how to connect with people at every step along the way. She obtained a Ph.D. in Organizational Psychology. She is currently the Vice-President of Leadership Development at the Institute for Health and Human Potential (IHHP), where Dr. Warren specializes in organizational culture and (as the title implies) leadership development.
Much of her success as a psychologist, a professional, and a person has come about as a result of her ability to understand others. But that success was not easy to attain, and got off to something of a rocky start.
“Don’t worry about becoming a psychologist, that it isn’t in the cards for you because you have too many strikes against you. Go for something that’s attainable, like becoming a secretary.”
This was the advice given to a young Cranla Warren by a guidance counselor before she applied to university, before she began to shape her career path, and before she had the “Dr.” in front of her name. The ‘strikes’ were that she was a Black girl – someone for whom academic success was unlikely, and for whom the path to that success was filled with dozens of barriers that did not exist for others. She overcame those barriers thanks, she says, to a very supportive family and series of great mentors. Not only through school, but through her professional life afterward.
“I’m very fortunate, I realize that every day. I’ve had incredible mentors through every step of my professional journey. I think, though, that I was vocal in seeking them out. Not everybody knows how to be proactive in doing this. When I was hired on at a pharmaceutical company I had worked in a hospital, I’d been a clinician, but I’d never worked in a business. I had done a talk, someone had seen it, and they loved what I presented, and they knew I was an advocate for mental health. They wanted someone like me to be in their medical education group. I got connected to the people who were in the seats of power, who said ‘I believe in what I see you doing and I’m going to help you rise in this organization’. Even though it may have been a potential career hazard for them. My advocates, mentors, and sponsors in the business world have always been white men, because that’s where the seat of power has traditionally been held.”
That proactive approach to seeking mentors and sponsors within an organization is one Dr. Warren imparts to many professional women, who seek her out for that very purpose. She mentors so that women and girls can see and work with someone who represents them, knows them, sees them and is also in a position of influence and power to a certain degree. The hope is that in these circumstances, and one day in all circumstances, these women and girls will no longer have to rely on white men to be their sole mentors as more and more women and people of colour assume leadership roles.
“I get sought out quite often by women, women of colour in particular, who say they want to learn how to crack the glass ceiling as it exists in their organization. They want to be leaders in their companies. But they keep bumping up against so many systemic barriers that they don’t quite know how to navigate. I’m trained as a coach, and I help coach them to create a development plan that’s separate from their organization to get them on a leadership path. A lot of it starts with self-awareness, emotional intelligence, how are you showing up? From there it broadens to the organization itself. Who can mentor them? Who might be a potential sponsor? Black women are often overlooked, and are invisible in many organizations.”
Dr. Warren has deconstructed her own path in order to see where the barriers lie, where the seats of power are concentrated, and what is required to break through in organizations for Black women in particular.
“Unless you have someone who has a seat at the table who’s advocating for you, who’s your champion and sponsor, who’s talking about you and your capabilities when you’re not in that room, it’s very, very hard to move forward.”
Having deconstructed her own path, and helped to create a path for many Black women to succeed in organizations across North America, Dr. Warren doesn’t stop there. The idea of mentorship, and the value that it imparts, is core to her philosophy in every way. She extends that idea to women and girls in her area as well.
“I’ve been a mentor for Black women and girls for probably 20 years. In the last decade, very formally, under the umbrella of a group called Trust 15, where I worked with their founder Marcia Brown to help provide very different experiences for the people in their programs Girls on the Rise and Ladies on the Rise. They hadn’t met anybody who had my level of education before, and I was driving into Toronto to be a role model, to be a mentor, to support them to effectively create their dreams and then to make a plan to achieve them.”
Dr. Warren created a program that brings young inner city Black youth she mentors to Stratford, where she lives, to take in the famous Stratford Festival. The young people get to tour the warehouse area and meet all kinds of people involved with the theatrical productions from actors to set designers. They come out of the experience with a newfound sense of what is possible. You can get work designing costumes, creating props, or making wigs? You mean those could be actual jobs?
“That advice I got [not to aim too high] from my guidance counselor was in the 70s, and here we are in the 2020s and young black girls are still receiving that same message. So, we bring them by bus to Stratford, partner with the festival, and provide a whole new lens for them to see the world through. It’s an incredible experience just to walk by the river and have lunch outside – things these girls don’t typically get to enjoy in their own neighbourhood.”

Dr. Andrea Howard
Dr. Andrea Howard, Developmental Psychology
Developmental psychology covers everything from infancy to old age, as human beings are continually developing throughout our lifespans. The ability to change as we progress is called ‘plasticity’, and we spoke to Dr. Andrea Howard about it.
“Plastics.”
When Walter Brooke uttered this memorable line to Dustin Hoffman in The Graduate, it was 1967. Brooke, as Mr. Maguire, was trying to impart wisdom to young Benjamin Braddock, telling him where the future lay. Audiences at the time were aware of the abilities of plastic, but would probably have been shocked to learn how prescient it really was. By 1976, plastic was the most-used material in the United States, and remains the most-used in the world today. There is no indication that this will be slowing down any time soon.
Because of the ubiquity of plastics, we all have a pre-determined sense of what they are, and when we hear a term like ‘plasticity’, it can seem odd. We think of plastics as mostly defined shapes – wagon wheels and Fresca bottles and inflatable reindeer and the like. Yet ‘plasticity’ is a term used to indicate the ability to be molded, to change, to adapt to fit a new container based on circumstance.
Dr. Andrea Howard is a developmental psychologist. An Associate Professor in the psychology department at Carleton University and the Director of the Pickering Centre for Research in Human Development at Carleton, she studies wellness during important developmental transitions like the transition to adulthood. She talks about plasticity a lot.
“A person at any time can be molded or changed in one way or another. Either by themselves, or by their environment or their genes or a combination thereof. It’s a term that caught on many years ago and we use it to describe potential. There’s really never a point in your lifespan where something different couldn’t happen. We talk often about people who start from a common place. Like two children who both had university-educated parents with similar incomes and similar childhood experiences, but who ended up in vastly different places.”
Many years ago indeed. The term was first used in the 1630s, usually in relation to art (sculpture, pottery, and so on). The term ‘plasticity’ does not come from ‘plastics’, and in fact predates it by several centuries. Rather, they share the same root word – ‘plasticus’ in Latin or ‘plastikos’ in Greek, meaning “capable of being molded into various forms”. It also forms the root for words like ‘plaster’ and ‘plasticine’. Dr. Howard says there are two periods in life when that plasticity is most prevalent – infancy and the teenage years.
“Developmental psychology has learned a lot about child development and the critical periods for capitalizing on that plasticity – on moving a child up or down in terms of their potential. Advances have helped us to see how critical the first three years – really, the first six years – are. Things like play-based kindergarten and play-based preschool are the result of that work. We don’t treat children like miniature adults any more because we understand they have different needs, and their ability to process and grow and thrive with information is very different than that of adults. Kindergarten in Ontario, for example, is a reflection of the science of child development. It’s certainly different from what kindergarten looked like when I was younger.”
In infancy, childhood, and adolescence an awful lot is happening in a short amount of time. That makes it of interest not only to psychologists but to parents, teachers, children themselves and the general public. But developmental psychology is a field of study that deals with the entire course of life.
“I think people have the mistaken impression that developmental psychology is about childhood and child psychology, and that’s not entirely true. All of our theoretical foundations are about understanding change across the lifespan, and a lot of the earliest work in developmental psychology came from aging. Many of the most foundational scholars studied development in the later part of life, and cognitive aging. A lot of very prominent developmental psychologists today still focus on that part of the lifespan.”
When I was a university student, I lived with two roommates, Sang and Kent. We threw a Super Bowl party one year, and my dad attended. I remember there being one play where neither team could corral a fumble, and the ball eventually ended up going out of bounds. My dad turned to me and said “you’d think they could just pick up the damn ball!” That, for me, was the moment I felt like I had entered adulthood. Dad was talking to me like a peer – casual swearing! Directed at me! I’m a grown-up! This transition to adulthood is what Dr. Howard studies, and she says it looks different for different people.
“Reaching adulthood is not something that happens in a short period of time. Children start approaching adulthood from the moment they’re born, but there are a lot of things happening in rapid succession as adolescents are reaching the end of high school, learning to drive at 16, becoming legal adults at 18. From the late teens to the late 20s is what most people would consider the transition to adulthood phase, but it’s very fluid and very individualized. Some people are going to feel that they have reached adulthood at an earlier age than others when they’ve taken on conventional roles like full time employment, becoming the head of a household, and paying their own bills.
There are plenty of people in their 60s and 70s who say ‘you know, I don’t really feel like an adult’. Or they feel like in some ways they are but other ways they’re not. There are no formal rules as to when someone ‘becomes’ an adult. We do have legal definitions of adulthood, and if you’re 19 you’re a legal adult and you have legal rights. But developmentally we’re more interested in how people perceive themselves and perceive others in terms of adulthood.
Over the past 30 years, people in Western countries – countries with more resources – have started to care more about less tangible indicators of adulthood. Like the ability to take care of yourself broadly, and taking responsibility for your actions, or individuating yourself from your parents in an interpersonal relationship. Whereas conventional markers have always been marriage, parenthood, full time employment, financial independence, that sort of thing. But those things matter a lot less, and plenty of people who have not necessarily met all those role transitions feel completely like adults. For a long time we’ve been seeing that people care more about intangible characteristics in defining whether you’ve crossed a transition to adulthood.”
The teenage years, as one approaches becoming an adult – however one might define that for oneself – are a key part of development. Once again, this is because it is a time with a very high degree of plasticity. Dr. Howard says that the brain development of teenagers has been a very important part of the research in the past several decades.
“One of the most important contributions of developmental psychology has to do with how we think about teenagers, and how much they need to be treated as children versus adults. A lot of that is coming from our understanding of brain development from age 10-25. Developmental neuropsychology has allowed us to understand that the brain continues to change in really meaningful ways, and that adolescence in particular is a period of extremely high activity and neurological change. It’s similar to infancy in terms of how much activity is happening. Over the years that’s changed how we think about adolescent decision-making and risk-taking and good versus poor judgement in high intensity situations. We know pretty well that a 16-year-old is just as good as a 30-year-old at reasoning during a calm, cold-cognition situation – a situation that doesn’t require rapid decision-making under pressure. Like voting, for example. But the 16-year-old is not so good at stuff like deciding whether to run a red light. Teenagers who are with friends tend to make riskier behavioural decisions. That’s something that has helped society decide how to deal with teenagers in decision-making and legal situations.”
So if 16-year-olds are just as capable as older adults in making a decision like who to vote for, how come they can’t vote? Dr. Howard reiterates.
“At one point 18-year-olds couldn’t vote either, but then they needed more people to fight in wars so they lowered the voting age. There’s no developmental reason not to allow a 16-year-old to vote. Whether our country would choose to go that route has more to do with whether adults are comfortable ceding some control of decision-making to younger people. The science of adolescent development suggests that a 16-year-old should be able to make as informed a decision as an older adult.”
And yet, 16-year-olds can drive. Those of us who have, at one time or another, been (or had) teenage boys might remember the incredibly high insurance premiums we had to pay – much higher than teenage girls, and astronomically higher than our parents or grandparents. I remember when Ontario instituted their ‘graduated licensing’ program – I was just a bit too young to have been exempt, and it added an extra step (and two extra years) to the process of obtaining a full driver’s license. That added to the expense, but not nearly as much as that insurance did. Dr. Howard says there’s a good reason for this.
“The reason your car insurance was so expensive when you were a 17-year-old boy is not because developmental psychologists told the insurers it needed to be that way, but because the insurance companies were recognizing that teenagers had way more collisions. And the reason that was happening is because of developmental differences. The graduated licensing program goes a long way toward moving novice drivers to being safer drivers.”
In addition to changing our attitudes about how we approach children in infancy, and teenagers during adolescence, a major shift in developmental psychology over the past three decades has been toward longitudinal studies. Hugely influential pioneers in the field once focused on the idea that there was a lot of universality in human development. Jean Piaget, for example, came up with the famous ‘stages’ theory, which divided human lifespans into four distinct developmental stages. Today, Dr. Howard says we see things a little differently.
“At one time questions focused on the idea that children achieve a stage and then can’t regress backward, and that everyone is pretty uniform at each stage of development. Now we know that’s a bit too fixed of a way of looking at things. The field has moved on from stage theories of development. In terms of how you would design a study, I think the biggest change has been moving from single-time-point surveys and experiments to collecting data over a long period of time (longitudinal data). There has always been longitudinal data, but it has grown to become a much bigger part of developmental psychology than it was in say the 90s. When you do a study now, you’re almost expected to collect data over months, years, or even decades.”
We’re starting to see some more prominent longitudinal studies come about as a result of COVID. Most of us have been asked to participate in one survey or another in regard to our mental health over the past two years, our daily habits, and our perception of the pandemic at different points along the timeline. Dr. Howard is no exception, although with one of her studies she says COVID ended up being more of a really interesting asterisk at the end than a central focal point.
“In 2019 we collected data from undergraduates at Carleton, 16-to-19-year-olds in their first year. They were straight out of high school and entering the transition to university, and we believe there’s an important opportunity for change with meaningful transitions like that. We collected data from them four times over the course of the first academic year, to see if the indicators of wellness we were measuring were moving around from month to month. Things like depression and anxiety tend to get worse from the beginning of the semester to the end, which we’ve seen over and over again. What was really valuable for us in collecting that data was that we ended up gathering some data right around the time we started having some lockdowns for COVID at the end of the academic year. Having several time points means that I have a data set to look at that can tell me how people in this particular population were doing up to and then during the transition to pandemic living. It allows us to see not only how groups of people in general are changing over time, but how individuals themselves change relative to their own baselines over time.”
COVID has of course been the #1 topic of discussion for all of us over the past two years, but for the past decade or so it has been social media. LinkedIn launched in 2003, followed quickly by MySpace. Twitter went online in 2006, and in 2008 Facebook overtook MySpace to become the dominant site. Today, we also have Pinterest (2010), Instagram (2010), Snapchat (2011), TikTok (2017), the list goes on and the landscape is endless. This is a big topic in Dr. Howard’s area, the transition to adulthood.
“There’s a lot of back-and-forth over the extent to which social media use is problematic for young peoples’ mental health and general well-being. Developmental psychologists are trying to remind the world that the things that are on your phone aren’t static activities you do, they’re contexts in which you live your life. When children go to school they experience a whole environment with people around them that could be influencing them, and they are also influencing the environment and the other people by their presence. Something like an Instagram platform is a developmental context that people are growing up in, which is a new thing compared to even a decade ago. So approaching social media use from a developmental perspective will help us understand not just whether being on the platform is good or bad for you, but what kinds of experiences you’re having on that platform that might be plastic – pushing you forward in a positive way or creating risk and negative experiences.”
In late 2021, a study conducted by Facebook themselves made huge international news. The major headline was that Facebook knew that Instagram (which they own) is having a profound negative effect on the body image of young girls. Adding to the sensational nature of the story is that the study was exposed by a whistleblower, and it certainly appeared as though Facebook had tried to bury it. But Dr. Howard says developmental psychologists aren’t buying the sensational headlines, the results of the study, or even the validity of the study itself.
“We had a real problem with that study, because it’s not well done. Facebook was accused of burying that research, but it was extremely low-quality work and doesn’t at all show that Instagram is bad for teenage girls. But because it was buried, and there was a whistleblower, it has a lot of visibility right now. In the public, parents and politicians often voice concerns that social media is damaging our teens. From a developmental perspective, that’s the wrong question to ask. Teenagers are on social media, as are adults and some children. So what is happening in those environments that’s good and bad? What is happening that improves peoples’ developmental potential, and what hinders it? The whistleblower study gathered young people who had completed some questions about body image and were exhibiting negative body image, and asked them how big a problem do you think Instagram has been for your body image? Priming your participants by saying ‘this is one of the reasons you’re having bad body image, how bad of a reason is it?’ is not a great way to get a response that tells us anything about the platform. But more than that, it was something like 70% of those girls, even after being primed, said it was either essentially not a problem, or that it helped them. But the focus was on the 30% or so who said that being on Instagram made them feel worse about themselves and that became the big headline. So, bad study design, wrong way to ask the question, and the results were interpreted poorly. Developmental psychologists would suggest approaching this issue very differently.”
Social media certainly has its ups and downs, and has sparked positive development as well as the more-publicized negative effects. Dr. Howard says the same can be said of virtually every domain studied by developmental psychologists.
“What brings people together under the banner of developmental psychology is an adherence to a theoretical framework about how we view the lifespan. Change is continuous and ongoing across the lifespan. There is always some plasticity and malleability in developmental experience and people can always change. There is potential for positive or negative growth at any time. What modulates your experience is what’s going on in your environment. We take a really broad theoretical perspective on how people progress across their lifespan, so that can bring together people who study infancy from that perspective and also those who study aging and dementia at the end of life.”
There is always plasticity. And it will always be called plasticity, even if our modern sensibilities suggest a different name might evoke a more apt visualization of how it works. That said, calling it ‘sillyputtyicity’ might be too…silly.

Dr. Elizabeth Hartney

Dr. Mari Swingle
Dr. Elizabeth Hartney and Dr. Mari Swingle , Quantitative Electrophysiology
Quantitative Electrophysiology studies electrical activity in the brain. We spoke with Dr. Elizabeth Hartney and Dr. Mari Swingle about the real value of lie detector technology and the value of boredom.
Quantitative Electrophysiology
No lies detected
There’s a scene in a Seinfeld episode where Jerry is interrogated using a lie detector by a police sergeant who doesn’t believe him when he says he’s never watched an episode of Melrose Place. Thanks to some advice from George (“it’s not a lie if you believe it to be true!”) he does fairly well until anxiety gets the better of him and he cracks under the pressure, admitting to being very much into Melrose Place. For an examination of the ‘femmephobia’ present in this scene, see the spotlight on Sexual Orientation and Gender Identity earlier in Psychology Month!
We’ve all seen similar scenes on TV and in movies, where people have electrodes attached to their fingers and hands, and where the machine quantifies their response to the questions being posed. I think most of us know by now that the machine is not actually measuring truthfulness, but rather anxiety. And while it is not very useful in its purported purpose – the detection of lies – this technology is actually very useful in the detection of anxiety! This is the realm of quantitative electrophysiology.
Dr. Mari Swingle is a practicing clinician, a researcher, an author and a presenter. She has a PhD in psychology and an MA in education, and she is certified in neuroelectrophysiology. She is the treasurer of the CPA’s Quantitative Electrophysiology section. She describes the discipline this way:
“We read the electrical activity from the brain, which tells us so many things. We can read from the upper levels of the cortex and get lots of information, and we can also go very deep into structures and circuitry within the brain. You need extremely sophisticated equipment to do this, and you need extremely sophisticated clinicians to read all of it.”
Another of those extremely sophisticated clinicians is Dr. Elizabeth Hartney, the Chair of the Quantitative Electrophysiology Section. Dr. Hartney is a registered psychologist in BC, and is board certified in neurofeedback and biofeedback (two predominant forms of quantitative electrophysiology).
“We’re certified by the BCIA, which stands for the Biofeedback Certification International Alliance. They provide biofeedback certification across the world. Biofeedback includes a few subdisciplines. The one Mari and I most closely work in is EEG (electroencephalogram) neurofeedback – but we also have peripheral biofeedback, which picks up electrical activity from the nervous system through the rest of the body. So we could be applying electrodes to your fingertips, to the palms of your hand, to read your heartrate variability or skin conductance. It’s basically all the stuff you see in the lie detector test on TV – which isn’t really great at detecting lies, but is really good for detecting anxiety. Anxiety is one of the things we work with a lot.”
Biofeedback is about becoming more aware of, and gaining greater control over, the functions of one’s own body. It can be used to help people experiencing anything from irritable bowel syndrome to side effects from chemotherapy. Dr. Hartney continues,
“We work with people to get feedback on their breathing, their heart rate, their blood pressure, all kinds of conditions that can be psychosomatic and involve both the mind and the body. There are specializations that others do in this space around urinary incontinence. The whole approach is about empowering the individual to gain control over their own body and their own brain – and in some cases their own bladder!”
In case the words ‘quantitative electrophysiology’, ‘neurofeedback’ and ‘biofeedback’ weren’t daunting enough, the clinicians who work in this discipline tend to add a few more. Like physiology, which also describes their work! There’s neurophysiology, which deals with the signals from the brain. There’s also general physiology, which deals with the full body, including the brain. Depending on the circumstance, quantitative electrophysiologists might be talking about only the body, or only the brain, or both in tandem. Dr. Swingle talks about two different ways this might look.
“There are huge volumes of research on what we call ‘brain mapping’. So, how do we read the electricity and what does it tell us? We work to either clinical or normative baselines. Normative baselines are measurements taken from brains of individuals who don’t have any overt symptoms or diagnoses. They don’t have ADHD, depression, psychosis, and so on. We look at what the brain looks like in that case, and we can then treat people who are suffering from ADHD, depression, or psychosis and we help them get to normative (or typical). What Elizabeth and I primarily do is the other branch, working from clinical databases. This means we have electrical readings from the brains of individuals who do suffer from anxiety, insomnia, scholastic difficulties, you name it. We then train the brain away from that measurement.”
This mostly involves taking existing processes in certain areas of the brain and either enhancing or diminishing their strength. This can be an effective way to treat depression, anxiety, ADHD and other conditions. When it comes to situations that involve actual damage to the brain itself, the treatment looks much different. Says Dr. Swingle,
“When we’re dealing with very severe strokes, or structural brain differences, then we’re looking for different pathways [what is often referred to as neuroplasticity – the ability of the brain to overcome damaged parts by learning how to use other parts to perform the same functions]. The majority of the work we’re doing is working toward making existing pathways more efficient. Some are underpowered and some are overpowered. A good example is the foundational work of Davidson. He looked at the balance of the frontal lobes, left vs right. He found that if the cortical electricity was more than 15% higher on one lobe than on the other, that was almost always indicative of emotional deregulation.”
Showing the brain an easier way
The field of quantitative electrophysiology has changed a great deal in the last twenty years, most notably because of the advent of the personal computer and greater technological power. For a discipline that relies enormously on technology, this has been a boon – but has also made disorders, and the treatment of them, much more complex. Dr. Hartney reflects on this change.
“It has actually become easier – but also much more complicated – with the rise of personal computers. They’ve made the process of getting and giving feedback from and to the brain much more entertaining. Therein lies a problem. Before we had computers, psychologists like us used lights and sounds that would light up or ding when our brain was doing what we were training it to do. That would be the ‘feedback’ part of the ‘neurofeedback’ or ‘biofeedback’. That actually worked really well! What we have now is fancy computer games and puzzles and videos that go on and off according to what your brain is doing and we have fantastic arrays that we can observe that show the frequencies of peoples’ brainwaves in several different sites at once.”
Dr Swingle provides a specific example of the kind of work she and Dr. Hartney might do for a client.
“We might want to augment a brainwave at one location on the brain for a specific purpose. For example, we want to augment theta [a type of brainwave] at the back of the brain because when theta is higher at the back of the brain you have greater stress tolerance. We can use that to help with insomnia, anxiety, addictions, all these types of ailments that would benefit from the brain being quieter. We attach an electrode to a very specific site, and ask an individual to interact with a computer. A really simple way of doing this is when the theta moves in minutia, a cricket jumps on the screen. Let’s say we have a young person who is having trouble with extreme anxiety and they need help with calming. All we do is ask them to make the cricket jump. Little ones don’t ask how do you do that, why do you do that – they just say okay. So it’s really easy to work with munchkins! We’re behind the scenes watching the pure wave forms and the amplitudes and ratios so we can see the frequency of theta come up, and manipulating thresholds to make it easier or harder to make the cricket jump. What we’re doing is giving that child the control to augment the theta wave on their own. When we show the brain an easier way to do something, it will take it.”
Boing boing boing boring
As I’m writing this spotlight right now, there is a TV on mute in the background. Team Canada is playing for the gold medal against the United States in the Olympics on the screen. My phone sits next to me and is constantly issuing notifications – Dr. Jonathan Stea just liked my tweet, CTV Ottawa has started a live video on Instagram from the protests in downtown Ottawa. I haven’t played Words With Friends in three weeks, and they want me to know they miss me. I have to stop typing every now and then because email notifications obstruct the screen, and I’ve received 14 since I started writing. Dr. Swingle has written a book called i-Minds: How Cell Phones, Computers, Gaming, and Social Media are Changing our Brains, our Behavior, and the Evolution of our Species about just this sort of thing. She says,
“An issue in our discipline is that things have become so fancy that they’re not as efficient. A cricket jumping for five minutes is fun. A cricket jumping for forty minutes is boring! And the kids go back to these incredibly involved amazing-looking video games. So what happens is we’ll get really good data in session, but the brain doesn’t change on any permanent level. When working with children, especially those with attention difficulties, screens have to be a little bit boring to work. That’s become something of an inner conflict within our discipline.”
So how has that changed in the past decades? Do kids find the cricket boring today because they are used to a much higher level of interactive screen time with more stimulation? If they had been exposed to this in 1988, would they have found the cricket to be entertaining for a longer time? Dr. Swingle says yes – and no.
“You could sustain the attention longer with lesser stimuli 20 years ago, but it was still boring! It’s a larger problem now because a lot of interactions with technology are affecting the development of childrens’ brains. A lot of children don’t know how to ‘sustain the mundane’ because everything in their lives is going at such a high pace. If you do one hour of neurotherapy a week, but 20 hours of gaming a week, the gaming is likely to win. And it does the exact opposite of neurotherapy, it trains the brain to respond only to excitement.”
If you hop on a treadmill or a rowing machine for 30 minutes a day, that’s likely very good for you – but if you spend the rest of your day eating nothing but poutine and peanut butter cups, the effects of that rowing machine will likely be greatly diminished, and you are unlikely to see the results you desire.
At the same time, if you go to the gym every day for three months, working with a personal trainer to figure out an ideal workout regimen, you might be able to maintain the fitness level you desire afterward by going only once a week. This is the goal of electrophysiology – that the changes you make in your brain become part of you, and they stay after the process. Says Dr. Hartney,
“The ultimate goal is that you want your client to learn how to change state without the help of the feedback. One of the things we’re dealing with is that young people in particular see this as a form of entertainment, and don’t necessarily understand that it’s an educational process. We’re trying to teach them to change state, but because they’re overloaded with the bells and whistles and animations it’s much harder for them to generalize what they’ve learned in a session outside that environment.”
On the value of boredom
Every Friday night, my family does a Games Night with friends over Zoom. We play a game using our phones as we all share a screen. The rapid advancement of technology over the last several years has made such incredible things possible, and it’s great that we’re able to connect this way, especially during a pandemic where other methods of connection might not be available to us. But I notice the kids approach it a little differently than the adults. While we’re waiting for a game to load, they’re playing a different game on their phone. Or, while it’s not their turn they’re dealing out cards on the table here in the house so there’s another game to play during the 90 second gaps in action. Dr. Hartney explains why this is becoming more common.
“We’re of an age where being bored was a normal part of childhood. If you went to your parents and complained about being bored they’d give you a chore, or suggest you figure it out on your own. We grew up expecting things to be a bit boring and seeking out our own entertainment. This generation just don’t have that same kind of baseline.”
Like Dr. Hartney, Dr. Swingle is also a big fan of boredom!
“All creativity and all innovation comes from boredom. If you don’t have boredom, you don’t have curiosity. You don’t have time to assimilate things and see patterns, and so on. We’re going far beyond our work in quantitative electrophysiology to the bigger picture now, but they are intrinsically linked.”
Before we go too far beyond quantitative electrophysiology, we’ll leave it here.
Stay bored, folks!

Dr. Jen Theule

Dr. Cathy Costigan
Dr. Jen Theule and Dr. Cathy Costigan, Family Psychology
The field of family psychology is as dynamic and complex as families themselves. We spoke to Dr. Jen Theule and Dr. Cathy Costigan about families, definitions, and the vast ‘systems’ that encompass them all.
“No healthy person is totally independent.”
At the end of The Godfather Part III, Michael Corleone (Al Pacino) dies alone in a courtyard, having apparently cut all ties with his family and the family business. On closer examination however, he can never have fully cut ties with his family – they made him who he is, and they shaped the path of his entire life. In fact, even the courtyard where he is sitting as he slumps over and dies is in the villa belonging to Corleone family friend Don Tommasino.
In our culture we tend to think about people as individuals much of the time. In this way, we think of a good health individual separately from their family, and rarely think about them in that larger context. Family psychologists, on the other hand, think about that context all the time. Dr. Jen Theule is an Associate Professor at the University of Manitoba in the school and clinical psychology programs, and the Chair of the Family Psychology Section of the CPA. She says many things we experience in our daily lives come about as a result of family psychology.
“Rooming in at the hospital instead of the baby going to a nursery as they once did – that’s a family psychology thing. Inviting family members into medical appointments and discussions. Parent-teacher meetings. Anything where we involve your family context, and involve more people in the discussion, those are the kinds of things family psychologists push for.”
When Amerigo Bonasera comes to visit Don Corleone on the day of his daughter’s wedding to ask for a favour, it is not just him and the Godfather in the room. There are others, among them the family consigliere Tom Hagen (Robert Duvall). These decisions are not made by the Godfather alone – he values input from those closest to him.
There are the discoveries brought about by science and the study of families, and then there are the applications of those innovations in dealing with family dynamics, often but not always in a therapy scenario. Says Dr. Theule,
“I think of family psychology as two things. One, it’s the study of ‘the family’ – parent-child relationships, romantic relationships, multigenerational families, close friendship groups, that kind of thing. Learning about how families operate, both the larger family units and all the subsystems within them. And two, it’s the application of that research to interventions. Family therapy, couples counselling, those kinds of things.”
Dr. Cathy Costigan is a Professor in the psychology department at the University of Victoria.
“I teach about what we call ‘developmental psychopathology’, or the mental health challenges of children and youth. I teach that from a strong family lens, all about how we understand childrens’ normal and abnormal development. I also teach family therapy to graduate students, which involves ways to intervene at a ‘systems level’. We see problems not as ‘there’s something broken within a child that we need to fix’ but rather by looking at the relationships among the different family members and their communication patterns. It is these broader ‘systems’ issues that might be creating or maintaining some stresses in a family where the child might be the one expressing the stress in the family by say, acting out in school or having meltdowns at home.”
Both Dr. Theule and Dr. Costigan speak a lot about ‘systems’. It’s a way to be a little more broad and inclusive when speaking about families. It’s not just a nuclear family of two moms and two kids – it could also refer to the extended family of grandparents and cousins, or a close-knit friend group, or a large hippie commune in California that has been running continuously since the 70s. Dr. Theule explains,
“Everyone’s impacted by various systems. Whether that’s who you work with, or who you live with, or are related to, or your friend group. All of those things operate quite similarly to families. Most people would consider a foster family to be a family unit of a sort, but the larger world might struggle with things like ‘is my roommate my family?’ By and large, society still considers ‘family’ to be a nuclear family – a mom and a dad and 1-4 children. But in some communities families are more broadly defined, and are larger. So when I use the term ‘system’ people might be more okay with the idea that the family can include Auntie or Grandma – or even roommates.”
How big, exactly, is the Corleone ‘family’ in the Godfather movies? Is it limited to just the immediate family members – Vito, Michael, Fredo, Sonny, and Connie? Does it extend to spouses? Children? Is Tom Hagen, informally adopted by the Corleones at a young age, truly a family member? What about all the ‘made’ guys – is that official induction into the organization, or into the family itself? In fact, where does the ‘family’ end and the ‘criminal enterprise’ begin?
Every community, and every culture, defines ‘family’ a little bit differently. For Dr. Costigan, it is these definitions of family, and the cultural differences in what constitutes a healthy family, that interests her.
“These days my research is predominantly focused on immigrant and refugee families. Looking at ways in which families under stress and cultural adjustment harness the resources and strengths within them as they go through changes from one country to another, along with the various traumas that might have accompanied that journey to come to Canada. How do they maintain strong family ties against this backdrop of many cultural differences, where each individual family member might be adjusting to Canadian culture in different ways and at different rates that might create tensions within the family?”
One of the ways these tensions manifest themselves might be for parents who are here in Canada, but whose own parents and extended families are still living back home. With today’s global technology, they are more connected to those remote family members than they could ever have been before. Sometimes that connection puts parents in a tough situation. The expectations of their own parents as to the proper way to raise children might now contrast greatly with the expectations of their own children who are growing up in Canada. It’s this kind of tension Dr. Costigan deals with often within the families with whom she works.
Family Psychology, as a discipline, has been moving this way for some time. An increased emphasis has been placed on cultural variation in families. It’s moving away from an implicit assumption that the Canadian context (the white family with Western values) is the way a family should function. Instead, the focus is more on what good and effective parenting looks like, or good communication within a family. This, of course, varies greatly by culture. Healthy family functioning doesn’t look the same for everyone, and acknowledging this has been a big step forward for family psychology over the past few decades. Dr. Costigan gives an example:
“In White Western culture, we have the primacy of the marital relationship between partners, whether that’s same-sex or opposite-sex. The partners play a leadership role in the family and there should be good boundaries around the decision-making in the family, where kids aren’t really a part of that. We might consider it problematic if kids are too privy to adult issues or too involved in adult decision-making. In some cultures, however, the primary relationship is parent-child. It can be desirable for children to contribute to the family at a much higher level than we expect in Canadian culture. Fulfilling those family obligations is really a strength, and it’s part of a healthy adaptation for that child from that cultural lens.”
For psychologists who specialize in working with families, their work can involve every moment of the lifespan, from dealing with a newborn arrival into the family to planning for end-of-life care for a parent or grandparent. Dr. Costigan says that in all those situations, although the approach might be vastly different, the fundamental principles remain the same.
“The core family functioning systems principles around communication and problem-solving have relevance at every phase of the lifespan. How do you get families to share what they’re thinking in respectful and helpful ways, how do you get them to solve problems in ways where everyone feels heard? Adult children can live their own lives fairly independently. Then when their parents start to decline they have to interact with one another and deal with each other much more, in a really emotional context. Some of those old wounds of childhood interaction can really rear their heads and disrupt that process. That’s an example of a prime time when psychologists might want to get involved, to help a family navigate that difficult phase of the lifespan.”
Or, maybe, psychologists might want to get involved right after the death of a family patriarch. This could potentially avoid future disagreements and betrayals, and ensure that Fredo never sealed his fate by taking sides against the family. I mean, maybe. The Godfather had some pretty difficult family dynamics and precious few psychologists.
Over the past two years, a new test has been placed on families and, by extension, the family psychologists who help them. Not only has the pandemic increased mental health difficulties, it has made it harder to reach out for the supports that could once have alleviated some of those issues. Says Dr. Theule,
“I think the last two years have put a lot of pressure on families who live together. The pandemic has taken away a lot of the larger system, and the supports that come with it like grandparents. We have a lot of great technological innovations, but those innovations aren’t going to come over and take care of your kids when they’re sick, or change a diaper for you. They don’t solve instrumental needs. In my estimation, a lot of research in the last two years has opened a lot of eyes outside the field of family psychology. Psychologists all sort of anticipated this, but to see the stress that children, people with disabilities, and older individuals – people who rely on the family system a little bit more – how impacted those individuals were by stresses to caregivers. It made people realize that maybe focusing on the adults who help those who need the extra care is one of the best ways to help those people who need extra care. For anyone who’s relying on others, a caregiver is really important and I think that may have been a shift in the larger community.”
Again, Dr. Theule is talking about systems. The future of family psychology is an integration of what the experts know now into a much larger, and more complex system that we can call a ‘family’.
“Family psychology is just starting to scratch the surface of the whole system. We’re really good at examining the parts of the system – what happens between a couple, what are the dynamics between one parent and one child, and so on – but a family isn’t just all these little parts added together, it’s greater than the sum of its parts. So how do you look at, and measure, something as complex as a family system? They vary in size, in culture, in dynamics in every single family. That’s where we’re trying to go – to look at the larger systems. Some research is being done now into triad dynamics, like one parent and two children, or two parents and one child. But the amount of complexity it adds to go from two people to three is so large that this is a huge shift already.”
Picture a diagram that you draw on a piece of paper. If you have two people (two dots on the diagram), there is only one line that can be drawn between them. Add a third person (third dot), and there are now three lines that can be drawn between individuals. One more person – three times as complex. Add a fourth, and there are now five possible lines. And so on – so you can imagine how difficult it must be when you’re dealing with a whole family system, where there can be upward of nine, ten, or even thirty people involved. Making sense of those systems might be the monumental task facing family psychology over the next several years.
Dr. Theule and Dr. Costigan will be a part of that – making sense of the incredible complexity of family systems, and coming up with more effective interventions and treatments as a result. There may, however, be one question they will not be able to answer. What, exactly, convinced Francis Ford Coppola and Al Pacino that making that third Godfather movie was a good idea?
 Dr. Donna Ferguson
Dr. Donna FergusonFebruary is Black History Month, and the CPA is spotlighting contemporary Black psychologists throughout the month. Dr. Donna Ferguson is a clinical psychologist in CAMH’s Work Stress and Health Program and also runs a private practice where, among other things, she does refugee and humanitarian assessments.
“It’s nice when we hear back from some lawyers who say our report really made a difference in this case.”
It’s rare that a lawyer will reach out to Dr. Donna Ferguson to give her an update of any kind. But when they do it’s a great feeling because she knows she’s made a difference for a refugee seeking asylum in Canada. Dr. Ferguson is a clinical psychologist in CAMH's Work Stress and Health Program and also runs a private practice where, among other things, she does refugee and humanitarian assessments. She says,
“A lawyer may have a client who’s here from their country of origin, where they may have experienced trauma. Sometimes at the hands of a spouse or partner, or it could be bigger than that – it could be political violence. They might be fearful for their lives. Part of their refugee claim might be to have a psychological assessment to establish a diagnosis.”
The diagnosis from Dr. Ferguson and her team is not deciding whether or not a person stays in Canada, or whether their claim of refugee status is legitimate. They are not functioning as some kind of lie-detector test that one might see in the movies. Rather, they’re assessing a person and making recommendations based on what that person has been through, and what they might experience in the future.
“If there is a diagnosis of Post-Traumatic Stress Disorder (PTSD) for example, we would build a case to say how it happened and if possible, get them into treatment here. And we can say that if they were to be sent back to their country of origin, they would have an exacerbation of those symptoms, and we would make recommendations around that.”
During the pandemic, these assessments are happening more rarely – doing them over virtual platforms has proven to be difficult, especially when a translator has to be added to the mix. During this time, Dr. Ferguson has found herself focused more on her job at CAMH, where she has found herself moving away from her original speciality, gambling addiction, and more into the space of workplace mental health.
“I do a lot of panels for CAMH as the Workplace Mental Health Person, giving advice to business leaders. We do Workplace Safety and Insurance Board (WSIB) work, and those are the primary clients we see. Over the past 20 years I’ve got to know a lot about the workplace! The dos and the don’ts in terms of what business leaders should be doing for their employees, and how to keep people well at work.”
Again though, the pandemic has thrown a bit of a wrench into that. Years of learning the ins and outs of business culture, the best practices, and crunching the data from all kinds of studies has not prepared anyone for the sudden shift to a virtual business operation.
“A lot of this is a work in progress. People had to get creative really quick when it came to the pandemic, to build a virtual environment. CAMH has done it in a lot of ways – our program is fully virtually functional. We rebuilt our assessment tools to be virtual, our individual and group treatment programs, and all of our meetings became virtual. CAMH as a whole, and not just our program, has really done a lot virtually, and that knowledge has been instrumental in helping other organizations.”
Whether helping businesses with a longstanding culture adjust to pandemic life while looking after the mental health of their employees, or helping people from a vastly different culture find assistance here in Canada, Dr. Ferguson’s plate remains full. And the work, no matter what form it takes, remains rewarding!

Dr. Brigitte Sabourin

Dr. Nicholas Carleton
Dr. Brigitte Sabourin and Dr. Nicholas Carleton, Clinical Psychology
Clinical psychology is the branch of psychology most of the public thinks about when they hear the word ‘psychologist’. But we have moved far beyond the patient-lying-on-the-couch cliché, and clinical practice has entered the virtual world online. We spoke to Dr. Brigitte Sabourin and Dr. Nicholas Carleton about where clinical psychology is today.
Early in his career, Sigmund Freud specialized in hypnosis. He would hypnotize patients in order to get them to open up about their symptoms, which would then presumably reduce their severity. He was quite new to it, and not very skilled, so he needed his patients to be as relaxed as possible – so he had them lie on a couch while he smoked his cigar and told them they were getting very sleepy.
Eventually, he discovered that simply having patients talk about their symptoms in a relaxed atmosphere might be even more effective. He ditched the hypnosis, but kept the couch (and the cigar). Other psychoanalysts who followed in Freud’s footsteps adopted the couch themselves – to the point where the Imperial Leather Furniture Company in New York City became a very wealthy corporation thanks to the sales of ‘analytic couches’ in the 1940s. The psychoanalyst with the cigar and the austere couch became a ‘meme’ of sorts more than seventy years ago. One that persists to this day.
Where would the New Yorker cartoons be without the psychologist couch? Bob Mankoff, himself a former experimental psychologist, is the cartoon editor of the New Yorker. He says the analysis couch in cartoons is a useful shorthand, one that immediately conveys a power dynamic. In The Sopranos, when Tony sees his therapist, he sits in a regular comfortable armchair – but the couch is there in the background, lest we forget what kind of office this is.
Of course, the field of psychoanalysis has progressed a great deal since the heyday of the Imperial Leather Furniture Company, and sitting behind a patient’s head while they talk on your couch is a thing of the past. But powerful images, engrained in popular culture, can hold a certain amount of sway long past their expiry date. As the image of the cigar-couch-psychologist fades, so too does the stigma around seeking help for one’s mental health.
Dr. Nicholas Carleton is a Professor of psychology at the University of Regina, a registered clinical psychologist in Saskatchewan, and is currently the scientific director of the Canadian Institute for Public Safety Research and Treatment. He is encouraged by the progress of the field in debunking and breaking down stigma in seeking help for mental health concerns.
“I think we’re watching stigma fall, and I think it’s largely because psychologists are increasingly out in the community. The notion that it will look like a Mad Men episode when you walk into a psychologist’s office, with a big old leather couch and someone smoking a cigar, all of which could feel very ominous, I imagine is pretty much gone from what actually happens. I also think we’ve started to diffuse that now mythical notion of what happens a little bit.”
Dr. Brigitte Sabourin is an Assistant Professor at the University of Manitoba in the clinical health psychology department, and a practicing clinical psychologist in Winnipeg. She is the Chair of the Clinical Psychology Section at the CPA, and says the field has come a long way but the core goals remain the same.
“We can define ourselves as a field of practice where we deal with human functioning. Clinical Psychology runs the gamut from identifying human problems and solutions to promoting general physical, social, and mental wellbeing. This involves assessment, treatment, consultation, program development, program evaluation, research, mentoring, teaching…”
Dr. Sabourin specializes in clinical health psychology, at the intersection between health psychology and clinical psychology. She does her work in a tertiary care clinic dealing with people who have chronic pain. This means looking at the biopsychosocial aspects of living with a chronic health condition, and applying clinical psychology skills and behavioural health principles to try to support them. Most clinical psychologists have a specialization like this, whether it’s in a hospital setting or in dealing with specific mood disorders. This is not the only way the field has changed over the past few decades. Says Dr. Sabourin,
“I think for one thing, the field has become more diverse. Historically it was dominated by white men, and that continues to change. Our commitment to evidence-based practice is continuing to evolve in bringing together all our knowledge in terms of what we know about anything from mental disorders to human flourishing. We’re now using that knowledge a lot more in terms of improving our services and being accountable to the people we serve. I think also the settings in which we practice have evolved. You see clinical psychologists in settings anywhere from primary care to very specialized services, which means the settings and the populations we deal with are much more diverse than they used to be. I also think the acknowledgement of how helpful it can be to access services has progressed. It’s not about there being something wrong with you, or that you’re crazy – that stigma has started to go away and people are realizing that we can help anyone from an elite athlete to someone who’s really having trouble with basic day-to-day tasks.”
Bringing together that knowledge and using it in clinical practice is something both Dr. Sabourin and Dr. Carleton know well. Both are researchers in addition to clinicians. Dr. Carleton sees, and treats, a lot of first responders in Regina – particularly RCMP, as the academy is there in the city. He also does a lot of research with the RCMP and other public safety personnel (PSP). Recently he and his team created an anonymous online tool where PSP could assess their own mental health and then reach out for support should they need it. He says,
“I think we’re seeing a better integration of science and practice. We’re doing a better job of connecting with one another, and having reflexive relationships between those psychologists who are doing research and those who are doing practice. We’re seeing how science informs practice and vice versa in a more dynamic way. For example, there have been significant changes when it comes to PTSD. Thanks to clinical practice interacting very closely with research, there are now four symptom clusters instead of only three. PTSD diagnoses can now happen without having a singular event, considering the aggregate of compounding events. Certainly for our first responders and other public safety personnel, those were two huge steps forward. Public safety personnel were having difficulty specifying which event was causing them the most trouble because they would have experienced hundreds or maybe thousands of them within a single calendar year. Previously, they would go to see a psychologist and say ‘I’m in trouble’, and the psychologist might have said ‘so am I because I’m struggling to diagnose you unless you pick one event’. We’ve fixed those things, and we’re making sequential improvements and important advancements.”
Another advancement, one with which we’re all familiar by now, is technological. I am conducting this interview with Dr. Sabourin and Dr. Carleton via Zoom, and there are dozens of other virtual platforms available for meetings – and even therapy sessions. Dr. Sabourin says,
“I think something else that’s really taken off, especially since the pandemic, is the role of technology and innovation in terms of accessing psychological services. The idea that you have to go into a psychologist’s office for even a fifteen-minute session somewhere in a forbidding building is no longer how we think about clinical psychology. Now we can access video conferencing platforms, phone apps, and so on. For example, we’re doing a lot of our group-based programming where participants can be in the comfort of their own home, and not have to drive to the hospital and pay for parking, and figure out where they’re going and all that. Decreasing the barriers to care and increasing the flexibility of how we do things is an exciting development. It has been moving that way for a while, but in the last two years with the pandemic has really taken off.”
Doing virtual therapy was a pretty fringe notion two years ago before the pandemic hit, but over the course of the last two years a lot has changed. Psychologists who were wary of holding sessions on virtual platforms have learned to do so effectively, and the prevalence of this kind of technology has eliminated some barriers to care, made more psychological help available, and gone a long way toward the continued erosion of the stigma surrounding the seeking of mental health support. Dr. Carleton says it has also helped in other ways.
“At the risk of speaking heresy, I actually think that being required to work remotely – while it may have stymied conferences – has actually increased collaboration in many ways. I can meet with someone in Australia at the end of my day and beginning of theirs, and for half an hour we can swap notes. We’re not locked into a mindset that requires one of us to fly somewhere for 16 hours.”
Dr. Sabourin agrees. Not only are collaborations easier, but getting more psychological care to more people is as well.
“We’re looking at how to increase resources and our reach. Part of this is adapting the ‘stepped care’ model that’s rolling across the country. It’s a little bit of psychology for a lot of people, and then as the needs increase and get more complex you get to a more intense model. We were reading an article in a research journal about this model in Ottawa, and the director of my clinic was saying ‘I wish we could just fly to Ottawa and sit down and talk to this person!’ And I said ‘I’ll set up a Zoom meeting for Tuesday’. It can just happen so fast and we’re so used to the platforms that it almost feels like we are face to face when we talk this way.”
I do this food order thing, where I get food delivered from local farms in my area. The food gets delivered by Miles [not his real name], a big burly man with a beard down to his belt buckle who drives the enormous freezer truck. A little while ago we were talking about this new job I had just started with the Canadian Psychological Association, and Miles told me about a co-worker he was worried about who was becoming more withdrawn. He was worried about his friend’s mental health. Should I reach out to him? Should I leave it alone? As a non-psychologist, I couldn’t give great advice about exactly what to do, but I thought that gently reaching out could never hurt. The next few times I saw Miles he would give me updates about how his friend was doing. One day last summer when I was working out of my garage, Miles and this co-worker were both in the truck and came in to sit for a few minutes. Now every time they make a delivery to my house, we sit for fifteen minutes or so to talk a little bit about our own mental health. How we’re holding up with this pandemic, what the struggles have been for ourselves and our families. Dr. Carleton says this kind of thing is happening more and more often.
“We’ve seen huge improvements in the discussion of mental health. Instead of it being something that’s kept in the dark, people are having frank conversations. The fact that we’re at a stage where we’re trying to mobilize knowledge about mental health to help transition toward substantial change – that’s a monumental shift even in the last two decades. We may not be exactly sure what we’re going to do next, but at least now we’re no longer denying that we have important opportunities for the population with mental health. I think a lot of that’s come about as a result of the advocacy of clinical psychologists and other mental health professionals.”
We’re not all the way there yet – some stigma remains and hangs on, like that image of the cigar and the couch. But mental health professionals continue to work at eradicating it, and clinical psychologists are no exception. Dr. Sabourin sums up the message very well.
“It’s okay if you’re struggling – you’re human. Being a human being on this planet is not easy! We’re all trying to live our life but we didn’t choose who our parents were, we didn’t choose our genes, we didn’t choose the fact that our brains are probably still programmed to help us survive 20,000 years ago and our environment has changed substantially since then. It’s about normalizing that it’s okay when there are times in your life that are harder than other times. We see these amazing human beings who have flourished – like Clara Hughes, the Olympic athlete who recognizes she’s had trouble. We have really famous actors and politicians who are becoming open with their difficulties and that something can be done about it. We’re recognizing as a society that it’s not the case that you’re either well or you’re sick. You can find tweaks. You can find ways of having a bit of an easier go, becoming more comfortable in your skin, being more present in engaging with your kids. Many of us struggle, and the fact that you’re seeing a clinical psychologist doesn’t mean there’s something wrong with you, we’re just all human beings trying to do the best that we can in this not-easy world.”

Dr. Keira Stockdale

Dr. Sandy Jung
Dr. Keira Stockdale and Dr. Sandy Jung, Criminal Justice Psychology
The field of criminal justice is vast, and psychologists are involved with nearly every facet of it, from prevention to probation. We spoke with Dr. Keira Stockdale and Dr. Sandy Jung about their work in this space, and where the profession is headed from here.
“I was one of those people who watched shows like CSI when they first came on the air…”
Dr. Sandy Jung’s eyes just rolled out of the back of her head. “Oh no! No, Keira, don’t say that! Noooooo!”
Dr. Keira Stockdale is a psychologist with the Saskatoon Police Service and an adjunct faculty member at the University of Saskatchewan in the department of psychology. She is the current Chair of the CPA’s Criminal Justice Section, and she’s explaining what got her interested in psychology and, in particular, the psychology of criminal justice.
Dr. Sandy Jung is a Professor at MacEwan University in Edmonton. Her research is in forensic psychology, and she is trying to keep it together as she hears the words she dreads the most. TV shows that represent criminal justice science, in inaccurate and badly misleading ways, have been a thorn in her side for some time, it seems!
“I’m cringing because I hear this from students all the time. They get interested because they watch these TV shows and it’s sexy, it’s very interesting. To be honest I never watch crime shows and I still hate them to this day! So when students recommend something like Dexter to me, I just can’t. I won’t.”
Any student who thinks they’re getting into the world of CSI when they head off to school is quickly disabused of the notion. No crime is solved through DNA analysis and the identification of eucalyptus on a shoe sole in an hour. Very few investigations are enhanced by the taking off, and then putting back on, of sunglasses over the majestic riff of Won’t Get Fooled Again. This is, of course, true for Dr. Stockdale as well. She continues,
“I went to U of T to do a forensic science degree. And in the process of doing gel blots to compare the DNA to see if they match at a crime scene, I realized that the classes I was taking about the people who were actually perpetrating these crimes were way more interesting. From there I was fortunate enough to do a placement with the OPP in their Behavioural Analysis Unit. After that I just continued to get more and more people-focused, and that took me down the path of clinical forensic psychology!”
Yes, the Behavioural Analysis Unit is a real thing. Many of us even know all the shorthand – BAU! Unsubs! CODIS! Thanks a bunch, Criminal Minds! It will likely not come as a surprise to learn that a real-life BAU has precious few private jets, video-game spinoffs, or cameos by Jason Alexander. Dr. Stockdale says,
“When you walk in there are no pictures of people and phones ringing and all that – it’s just a quiet office where people do really good investigative work. They also develop risk-assessment tools or other methodologies that we can use to combat crime such as domestic violence and internet-facilitated sexual exploitation.”
So what, then, do psychologists who specialize in criminal justice actually do? Is it like B.D. Wong’s character on Law & Order, or more like John Francis Daley’s character on Bones…”no”. Dr Jung says there are two main types of psychologist involved with criminal justice, but that the field is incredibly broad with hundreds of different specializations.
“A clinician is probably the prototype of what we think of as a ‘Criminal Justice Psychologist’, but that’s only one half of it. The other half is the research and experimental psychology side. Not just research within practical settings like correctional or treatment facilities, but also research in terms of how the legal system intersects with psychology. Every decision that we make has a psychological component to it – it’s making decisions about how you interview a witness, or a suspect. How you’re gathering data and how you interpret it. And in the courts there are so many different decisions that get made that psychologists examine, like sentencing or jury decision making.”
Jury decision making, you mean like that guy in Bull who…”absolutely not”. Dr. Stockdale says that most psychologists who work in this space are, in a way, jacks of all trades and masters of just one or two.
“To be a good forensic or criminal justice or police psychologist, you’ve got to be a good generalist. We’re bringing a lot of our general psychological knowledge and our clinical understanding into this area of practice. At present, working with a police service, I’m working with an interdisciplinary team that tries to assess risk and intervene with serious violent offenders. The team has prosecutors, police, community probation, correctional facilities and mental health workers – and also psychology residents. We’ve developed risk assessment tools as psychologists that our partners in, say, probation or policing use. So part of our work is educating this team about how we can work together to really help these justice-involved individuals with histories of violence. Many have mental health needs, and we want them to get the services they require while promoting community safety. At present, we’re looking to develop greater virtual services and we’re also doing some great stuff with big data, predictive analytics, and modelling to try to improve risk assessment technologies. How do we assess needs for our clients, how do we know who’s at risk for re-offending, and why. We’re also applying that same technology to missing persons cases.”
One of the most well-known missing persons cases in the past decade in Canada happened in the Village in Toronto. Between 2010 and 2017, eight men from the gay community went missing. It was eventually determined that they had been murdered by a serial killer, who was arrested in 2018. The handling of the initial investigations by the Toronto Police Service into these missing people has come under heavy criticism and led to several inquiries and reviews. The external independent review was conducted by Judge Gloria Epstein. It was a failure on the part of the police, and the gay community in Toronto was failed. But Dr. Stockdale is hopeful that meaningful change will come about as a result.
“I’m optimistic that we’re going to see more and more academic partnerships with all areas of criminal justice going forward. We did work around missing persons, that came out of people reported missing in The Village in Toronto. In Judge Epstein’s report, she recommends that police departments (in this case Toronto) work with academic institutions and researchers because then you have people to support you in evaluating your programs and initiatives. People can’t do it alone – it’s a resource issue, but it’s also an issue of cognitive thinking and attitudes. The more we can work in interdisciplinary teams in criminal justice, the more we can guard against biases and maybe test out some of our assumptions or interventions. We can then tailor those going forward.”
The field of criminal justice psychology is always moving forward, always changing, and always (if slowly) getting better. Dr. Jung says the key to this is knowledge mobilization – the process by which research comes up with data and answers and then translates that work into real-world changes and best practices.
“We need to have a lot more knowledge mobilization going forward. There’s still a ton of research that has to be done, but we need to do better at implementing things that we already do know. There are some really nitty-gritty practical questions that we can help to answer. We know that high-risk groups should receive more supervision, but where is the cutoff? How many hours should we spend administering treatment? We’re disseminating this information, but we’re not putting it to use in practical terms the way we could be. The reality is that it takes about seventeen years before any evidence gets implemented. I remember hearing that citation once and thinking ‘well, that’s depressing!’”
Seventeen years is indeed a depressing statistic, and change can certainly appear slow. But Dr. Stockdale says she can see that change in many facets of criminal justice, including the work that she herself has done.
“I look at some of the psychological assessment reports that I wrote for justice-involved individuals years ago, and I realize just how much practice has changed. Canadians are known internationally for our development of risk assessment tools and technologies. Assessment years ago was a judgement call – will this person re-offend? Maybe? Now it’s a lot more structured and evidence-based. Now we look at a bunch of factors and figure out where we can intervene or provide support to reduce a person’s risk for violence, sexual offending or general criminality. Our treatment programs are much more focused than they were decades ago, as we really hone in on these dynamics or changeable factors.
We’re moving from negative and stigmatizing labels toward more positive language. Like ‘justice-involved individuals’ instead of ‘offenders’ or ‘inmates’. We are also moving away from focusing on the negative in treatment of people – and I think this is particularly important for youth in the criminal justice system – we’re accentuating the positive things like strength and resiliency.”
Another way criminal justice is changing is in terms of social justice. Again, this is a very slow process, as the justice system has so many giant components that it is a huge ship to steer. Dr. Jung says that researchers in the area have historically stayed in their own silos, but that this is changing now with social media and digital data making collaboration and interdisciplinary work easier and more accessible. She also says there is a long, long way to go before the justice system in Canada and those around the world achieve the equity toward which they strive.
“There are a few court cases that really brought attention to something that everyone already knew existed, but that we hadn’t investigated as much as we should have. It takes those cases to remind us that this is an incredibly important issue. When it comes to equity diversity and inclusion, there are certain subgroups that have been looked at but not all – we’ve done very little when it comes to gender, for example. I’d say we’re barely scratching the surface of the issue.”
Dr. Stockdale says that in thinking about issues like Me Too, Black Lives Matter, Indigenous oppression, she thinks about how little training in these matters she received when doing her clinical psychology PhD. In addition to educating teams, there’s a need to continue to discuss these issues more broadly. We’re moving into an era of smart prisons and risk-assessment apps, so she thinks maybe we can use technology in positive ways to move us down this road. She is also an advocate for a larger overall shift in philosophy.
“I think there’s a need to involve community groups and organizations, special interest groups who work with some of these populations and people. We, as criminal justice psychologists, like to apply science, but we also recognize that’s only one way of knowing. And in the justice system we have to be open to and respectful of other ways of knowing. That will be a challenge going forward, and I think we need to put a lot of focus there.”
Even the TV crime shows that create interest in criminal justice are starting to make a shift toward social justice themes – at least they’re trying. It’s often awkward, and sometimes ham-fisted, but then most of those shows are already awkward and ham-fisted. We know by now that it was not televised crime shows that got Dr. Jung into psychology – so what did?
“I was going to go into psychiatry, initially. I took a course in the third year of my undergrad at UBC with John Yuille and Robert Hare. Dr. Hare is the developer of the psychopathy checklist, and I found that so interesting and sexy and all of a sudden I was interested in a whole different field. From that point onward I started volunteering in some labs and gaining interest in both eyewitness testimony and psychopathy. I knew at that point I was in for good. It’s been quite a journey from there – I would never have thought I would go from doing forensic mental health to today working with police detectives on how they manage offenders in the community.”
Alright, one more pop culture reference. Dr. Robert Hare appeared in the 2003 award-winning Canadian documentary film The Corporation, where he appeared to conclude that, were a corporation a person, it would check almost all the boxes on the psychopathy list. However, in later edition of his book Snakes in Suits: When Psychopaths Go to Work, Hare suggested his comments were taken out of context by the filmmakers, and that in practice a corporation really wouldn’t meet the criteria of being called a ‘psychopath’.
As the vast subject of criminal justice grows and matures, and the psychology that accompanies it does as well, both Dr. Jung and Dr. Stockdale want to make sure we know that things are, in fact, getting better. That no matter how bad something looks today, remembering what it might have looked like twenty or thirty years ago shows that we are in fact making progress. Dr. Stockdale says,
“You’re safer now than you would have been in previous times, just walking around. Back in the 80s there were all these Stranger Danger campaigns and this kind of thing, imagining that you were most in danger from that unknown person who was lurking around a corner somewhere. Now of course, we know that you’re most at risk from people you know, and we’re all more aware of that now. We may not like these true crime podcasts, or cringe at CSI type TV shows, but I think there may be a protective function in that some of the evidence we’ve learned in criminal justice that’s talked about on these platforms has actually made us safer.”
Dr. Jung cringes.

Dr. Zarina Giannone
Dr. Zarina Giannone, Sport and Exercise Psychology
As the accomplishments of Olympic athletes capture our attention, we place today’s Psychology Month focus on the psychologists who help them attain that high performance. Sport Psychology, however, extends far beyond just high-performance athletes. We spoke to Dr. Zarina Giannone all about this exciting field.
Brooke D’Hondt is just sixteen years old, and she already has a team of coaches and experts helping her excel in the snowboard halfpipe. Brooke finished in tenth place in snowboard halfpipe for Canada at the Beijing Olympics, and when the games are over she’ll be going back to high school. Imagine being in her gym class!
Sport psychology sort of emerged from gym classes – physical education originated in the education world, and over time evolved into the sport psychology we know today. Traditionally, sport psychology graduate programs are housed within schools of kinesiology at universities. They offer graduate degrees which produce scientists within the field of sport psychology.
Today, there are two main paths a person can take to become a sport psychology practitioner, and two types of credentials that exist in North America. One is the registered psychologist, who has the broadest scope of practice when they have acquired the training and experience to declare a specialty in sport and exercise or performance psychology. The other is a professional called the ‘mental performance consultant’ (MPC). Those are people with science-based degrees who have done some applied training but have a limit in the scope of their practice defined by the application of psychological knowledge within that performance or sport setting.
Dr. Zarina Giannone has taken both those paths. A registered psychologist with a specialization in sport and performance psychology, Dr. Giannone did her graduate training in counselling psychology, but pursued applied training within sport psychology (the MPC). She says,
“Sports psychology is one field within the broader sports science domain. Even my own work as a sports psychologist is just one slice of a larger pie, in that it covers the application of performance psychology. It involves taking science and theory and applying it to real-life situations.”
The mental health of athletes has never been in the spotlight to the degree it is today. Elite athletes are talking about their mental health, stepping away from their sports to take care of it, and being fairly public about their struggles. Naomi Osaka, Simone Biles, Calvin Ridley, Clara Hughes, Andy Robertson, the list of athletes who have publicly started speaking about mental health is growing longer by the day. This is a trend that excites Dr. Giannone.
“Even through my seven years of grad school, I’ve noticed some changes which have been really exciting. In the early 2000s, the field focused more on traditional mental skills that were taught to teams, athletes, and coaches. Imagery, arousal regulation, attentional control, that sort of thing. These are important skills that, if mastered by athletes, can enhance performance. They are also transferable skills that can enhance general well-being and life functioning. In the last little while, personal psychologists and MPCs have been more highly sought. This is, among other things, because of the fact that athletes feel more comfortable disclosing mental health challenges. The stigma around these things has been reduced. And that means that the role of psychologists in sports clubs and organizations is more in demand.”
The Indianapolis Colts, for example, have launched an initiative called Kicking The Stigma, and the face of the campaign is their standout linebacker Darius Leonard, who opens up about his anxiety attacks and depression. But for every team that embraces mental health issues and tries to tackle the stigma around them, there seems to be a story about another group that has yet to catch up. The Canadian Hockey League recently came out with a devastating report about a culture where a “code of silence” enabled off-ice misconduct to become the norm. Says Dr. Giannone,
“I’m aware of some organizations and teams that do take mental health very seriously, and there are sport psychologists who are involved in working with problems from a social justice perspective. For example, those working with sexual abuse or misconduct cases. Those psychologists have had an impact in terms of creating systemic change in some organizations. You’re seeing more mental health policies being implemented, or diversity and inclusion policies. Hopefully people will experience the impact of those things, and it will be a matter of time before all major sport organizations get on board.”
This year at the Olympics is the first in a long time where NHL players are not there. That means that the hockey teams competing against one another fall into two categories – either a group of players who have been playing together in one situation or another for a long time, or a roster cobbled together from the best players available who have little experience playing with each other. How do you build team dynamics and trust? Dr. Giannone says this is currently becoming more the domain of sport psychologists and MPCs.
“Sport psychologists are doing more than offering traditional mental skills training and assessments. My work today focuses on optimizing performance, but it also extends into helping with other sport-specific challenges including interpersonal team dynamics, training leadership, and supporting diverse mental health challenges experienced by athletes like burnout, depression, anxiety, or disordered eating. In many ways, the role of the sport psychologist has been reimagined and now involves addressing both the psychological health and performance needs inherent in sport.”
Dr. Giannone’s main job is in private practice at the Vancouver Psychology Centre, where she sees both general psychology clients and others in her specialty practice in sport and performance psychology. In that space, she sees a wide range of athletes and performers – anyone from youth to professionals. On occasion she’ll take a contract with a team where she’s implementing a mental skills program or providing other group-based services. She also works with the Canadian Centre for Mental Health in Sport (CCMHS), where she provides mental-health-based services to athletes and performers.
“Since 2013, federal funding for services has really expanded, and quite rapidly. There are now a few federally funded services for national-level athletes. For example, there’s Game Plan, which offers a wide range of services to carded [elite level] athletes in Canada. My work with the CCMHS is for any level of athlete, coach, or administrator where certain people can access funding for that. Other countries are a bit behind on this stuff, making Canada a leader in this space.”
As with all major events in the past two years, COVID is a central issue at these Olympics. It has disrupted training, hampered team-building, and caused many athletes to miss their shot at competing on the world stage. It has even cost some athletes a chance at competing after they got to the games, when a positive test ended their Olympic journey early. Dr. Giannone has seen all the ups and the downs the pandemic has created for athletes of all levels.
“Near the beginning, sports were on pause. Major tournaments were postponed. At that time, it was really about modifying and shifting psychological services to an online delivery. We did some team-based things where there were more than 25 people on Zoom! Over the past year, a lot of athletes have returned to sport, and there are new types of challenges we’ve never faced before. The content of the work has shifted – like think about a youth athlete, where they haven’t been in a high school competition in two years. They were in grade 8 and now they’re in grade 10. What that means for them developmentally and in terms of sport-specific skills development is interesting.
A focus of my research is around identity development in sport. What happens to it when someone experiences injury, or retires, and the identity loss that comes with that. A lot of identity threat has come about as a result of COVID, from kids all the way up to Olympians. These people who derive such self-esteem and value from sport are involuntarily forced to put it aside for some time. That can be very disruptive for people.
I’d say, conversely though, COVID has provided athletes a unique opportunity for people to engage with their sport in a new and different manner. Maybe someone never had the time before to watch video of themselves, and they’re able to learn about themselves differently now. Maybe they’re able to do a bit more weight training. It has been striking to me how people have been so resilient and creative throughout this.
Something that really stood out to me at the beginning of the pandemic was a shift from physical and mental skills training to fostering new conceptualizations of team culture. I remember stepping into teams and helping to facilitate goals, helping to cultivate team values and relationships. Not that I wouldn’t do that during a regular season, but the pandemic really placed the spotlight on that because there wasn’t much else to do when everything was so up in the air.”
Athlete mental health is a rapidly expanding field. The role of psychologists in tackling some of the social and systemic challenges like athlete misconduct, mistreatment in sport, abuse and harassment, cultural inclusion and diversity, are really coming to the forefront. Psychologists are involved in helping to create support, but also in trying to promote systemic change within systems and organizations, and all of that trickles down to athletes. But their influence and involvement no longer end at the locker room door. Says Dr. Giannone,
“Sport psychology professionals have now gone outside of the traditional sport and exercise setting. They’re working with performance issues in other domains. It’s common to have sport psychologists working in the military, with performing artists, first responders, or with high-ranking business executives. Pretty well anyone in high-pressure scenarios. I would anticipate seeing more psychologists with these specialized skills making their way into diverse settings.”
The Olympics are on right now, presenting a series of high-pressure scenarios for elite athletes for public consumption, all day every day. We can share in the joy of the Canadian women’s speed skating pursuit team pulling out an improbable gold medal performance, while also empathizing with the heartbreak of the Japanese team whose stumble in the last turn gave that gold medal to Canada. Our eyes, the eyes of the world, add a pressure that doesn’t exist at any other time for these athletes. It can be a difficult situation, and one where a psychologist can help them navigate through it. Whether you’re Jennifer Jones, competing in your second Olympics at age 47, or you’re a 16-year-old snowboarder who is about to go back to geography class.
 Dr. Kofi-Len Belfon
Dr. Kofi-Len BelfonFebruary is Black History Month, and the CPA is spotlighting contemporary Black psychologists throughout the month. Dr. Kofi-Len Belfon is a clinical psychologist who works with children, adolescents and families. He wears many hats, one of them being as the Associate Clinical Director at Kinark Child and Family Services.
“Are we actually thinking about programming itself in an anti-oppressive way? Are we considering the content?”
Dr. Kofi Belfon is a clinical psychologist who works with children, adolescents and families. He’s the Associate Clinical Director at Kinark Child and Family Services, has a private practice called Belfon Psychological Services, is a member of the board of trustees for Strong Minds Strong Kids (formerly the Psychology Foundation of Canada), and sits on the Equity, Diversity, and Inclusion (EDI) Committee at the College of Psychologists of Ontario. He is a measured speaker, and thinks carefully about his answers to every question. The theme of “thinking” comes up quite often in our conversation.
Born in St. Lucia, Dr. Belfon immigrated to Canada when he was about five years old. His family moved to live in the Caribbean when he was about 15, and he stayed with friends of the family to finish high school in Canada. His parents emphasized education, and encouraged him to go to university. His brother is a physician, and at first he went to McMaster for his undergrad intending to follow the same path and become a medical doctor. Soon though, he discovered that not only did he do extremely well in his psychology classes, he really enjoyed them. A new career path beckoned.
After his undergrad, Dr. Belfon went to work at a paint factory. While there, he wrote his GRE test (Graduate Records Examination – a general, standardized test to measure graduates’ academic abilities) and applied to grad school for psychology. What he didn’t do, which may have made a difference, was take the specific GRE exam for psychology. Every grad school rejected his application – every school but one.
“The only place I got in was Guelph. I had a really great supportive, nurturing supervisor in Dr. Michael Grand. But I always had this sort of impostor syndrome, doubting myself. ‘I didn’t get in anywhere else, why did I get in here, are they just trying to fill a quota? Am I getting in because I’m Black and male and they want to increase the diversity in their program?’ I had all these doubts about myself and they lingered for a long time. It was a fairly small cohort, maybe five or six of us, and I was the only one without a scholarship. I applied year after year, and never got a scholarship, and that fueled some of that imposter syndrome and the feeling I didn’t belong.
The silver lining for me was a couple of things – one, it forced me to work because I didn’t have a lot of money! I worked a ton in the field. I worked at the Toronto District School Board throughout my PhD and I got a lot of experience doing that. I worked at a private practice, I worked at Syl Apps Youth Centre, and I got lots of really neat clinical experience. I was also always really happy about my research. One of the things I appreciated about Dr. Grand was that he didn’t get in the way of me doing what I wanted to do.
My research was in chronic community violence in the Scarborough region, and then for my PhD it was about the mental health needs of kids in custody and detention. At the time at least 50% of those kids I was working with were BIPOC. Some of that research was because in university I had a close friend who died as a result of gun violence. That was the impetus for me starting that research, and even today I wish I had more time to do research and that sort of thing because it really means a lot to me.”
With all the different positions Dr. Belfon holds, and all the hats he wears, there is precious little time for research – or anything else for that matter. Especially now, when he says the pandemic has increased the workload significantly. Wait lists are getting longer and longer, and more and more children, youth, and families are reaching out for mental health help. He says this increase in demand predates the pandemic. Anecdotally, he says he’s seen more young people seeking help for depression, anxiety, and mental health disorders over the past five years. It’s not clear whether that is because more youth are suffering, or because work to destigmatize these conditions has made them more willing to reach out for help.
Those who reach out to Dr. Belfon are often Black families who are looking to connect with a psychologist who looks like them, and presumably shares many of their experiences. Often, they are willing to wait for a very long time, more than eight months on occasion, in order to see a Black psychologist. He thinks this is not ideal – it’s a really long time to wait when you’re having serious difficulties, and there’s no guarantee that you will connect with a professional. As Dr. Belfon says, “we confound race and culture all the time”.
The rarity of Black psychologists remains a difficulty in communities of colour, and is keenly felt in Southern Ontario. At one point, Dr. Belfon says, he thinks Belfon Psychological Services employed 60% of the Black psychologists in the region – there were three of them. Another reason EDI is so important going forward in the field of psychology.
He brings an EDI lens to all his ventures, working to make programming more inclusive at Strong Minds Strong Kids, at Kinark, and in his own practice. Dr. Belfon says that it’s good to make an effort to use more inclusive language, and to choose images and examples that feature a more diverse group of people. These things are helpful in terms of access, and get more people through the door. But doing those things are still ‘on the surface’. Once you get people through the door, is the programming itself delivering for their needs? Is the program they’re accessing as inclusive as the messaging that brought them there in the first place?
“I don’t necessarily know what the answers to that are going to be. These are still early days for psychology in thinking this way. But we need to evaluate these things while thinking about diversity, and how different families might think about these things differently. For example, a parenting program where we’re talking about parenting practices and what we view in North America as healthy practices. That might be totally different for a family whose parents didn’t grow up in North American society and maybe don’t hold the same types of values.”
This is when Dr. Belfon comes back to the theme of ‘thinking’ – what matters most in Equity, Diversity, and Inclusion efforts is that they are top of mind when a program is designed, a committee is set up, or a policy is implemented. If we all start to look at those things through an EDI lens, and start from that place, it is more likely that the end result will be truly inclusive and more than window-dressing.
“We think systematically in agencies, about all the inward-facing things. Executive structures, hiring practices, policies and procedures, thinking about how we treat one another. Maybe we’ve changed some language, and done a better job with basic stuff like not having binary language related to gender on our forms. Once we establish a framework with those sorts of things – and we’re doing some of that work at Kinark right now – the next step should be getting down to the actual clinical practice, and thinking about that more carefully. That will take some time, and maybe nothing changes! Maybe we look at a program and decide ‘the content is what the content is’. But did we think about it? Did we think about whether the content is relevant or not, instead of assuming that all these constructs are culture-neutral? I think that matters a lot.”
With the College of Psychologists of Ontario, the EDI committee is not on an island, but is rather a group of people who are there to influence all the other groups that can benefit from their input. Dr. Donna Ferguson is the Chair of the committee, and Dr. Belfon is working with her and the others to make EDI part of the overall culture at the College.
“We’ve done some work learning about the experiences our membership has had with EDI and the college, starting off with some questionnaires and collecting some data from the membership. We’ve done some training in EDI with the other committees – like discipline, quality assurance, my own committee which is Client Relations – so we have some language with which to think about EDI as a starting point. What we’ve asked is that following that training, members on those committees are challenged to think about how EDI might be related to their work.”
Dr. Belfon, Dr. Ferguson and the rest of the EDI committee are going to each other committee, one by one, to discuss how EDI is related to their work.
“For example, if the registration committee is responsible for our oral exams, in the oral exams are there things we have to be thinking about from an anti-oppression or inclusion perspective that might have to be rethought?”
Thinking. It is the central theme of everything Dr. Belfon does – and it is the key to moving organizations, companies, groups, and even psychology itself in a more inclusive direction. It’s all well and good to do something – but before you did, did you think about it? Did you consider it through the lens of inclusion? And how are you ensuring that your programming is inclusive, rather than just looking inclusive?
It’s something worth thinking about.

Dr. Amir Sepehry

Dr. Diana Velikonja
Dr. Amir Sepehry and Dr. Diana Velikonja, Psychopharmacology Section
At the intersection of psychology and medicine is psychopharmacology. Psychologists who can prescribe medication like a psychiatrist, but with a psychologist’s training in behaviour and therapy-based interventions. Dr. Amir Sepehry and Dr. Diana Velikonja tell us more.
It generally takes about ten years of schooling in Canada to become a psychologist. It’s one of the longest, most intensive fields of study there is as it generally requires a PhD or PsyD, those programs are quite small, and it takes longer to complete a psychology doctoral program than most others. Imagine going through all that, and then deciding ‘you know, I could really use a little more school’. What kind of keener do you have to be to take on MORE education when you’re finally done?
This is the decision made by those who choose to follow the path of psychopharmacology. Dr. Diana Velikonja is a neuropsychologist by training. She is a clinical psychologist, and has a masters in clinical psychopharmacology – that allows her to do consultations with regard to psychotropic medication. She has worked with people who have had head trauma, is the Past President of the Ontario Psychological Association, and has led initiatives to advocate for the scope of practice for psychologists in Ontario to include prescribing psychotropic medication. She explains psychopharmacology this way:
“For a lot of emotionally-based or cognitively-based challenges, there are specific types of medications that are used called ‘psychotropic’ medications. They’re primarily used to treat conditions like anxiety, depression, hallucinations. For mental conditions or addiction issues, they help manage the symptoms. Psychopharmacology is really prescribing medications in conjunction with other evidence-based treatments. The reason psychologists are involved in this is that we’re trained in behaviour and therapy-based interventions, and those of us who have sought additional certification with regard to prescribing psychotropic medication are able to integrate the two – the behavioural and the medication in order to help guide patients toward the best strategies to manage the symptoms they’re experiencing.”
Prescribing medication to treat mental illness has, at least in Canada, long been the domain of psychiatry. Psychopharmacologists are some of the very few psychologists who have that level of knowledge when it comes to those medications. Dr. Amir Ali Sepehry is the Chair of Psychopharmacology Section at the CPA. He has a PhD in neuroscience, post-doctoral training in neurology, a masters in psychiatric science investigating medications, and other training in spinal cord injuries, and counselling psychology. Dr. Sepehry is currently teaching at the Adler University (Vancouver) and collaborates with UBC, and working with forensic neuropsychologists on medical legal cases. He says the field of psychopharmacology is both very old, and very new.
“It goes way back to when people with a variety of specialities used substances, herbs, and so on for the treatment of mental illness. However, there has been an incredible acceleration in the past five years, because much has happened. One part of that is the SARS-COVID-19 we have experienced. There are minor developments happening, as many of us are trying to repurpose medications.”
A person’s normal anti-viral immune response requires the activation of the inflammatory pathways of the immune system. ‘Cytokines’ are produced as part of that immune response. An unchecked and outsized immune response is known as a ‘cytokine cascade’ or ‘cytokine storm’. This can lead to tissue damage, and has been seen in many severe cases of COVID-19. It comes about as a result of an overabundance of pro-inflammatory cytokines. Dr. Sepehry says this is one of the ways psychopharmacologists are looking at the repurposing of existing medications.
“Anti-depressants have shown anti-inflammatory properties, so they could be used toward the cytokine cascade that is evolving as a result of COVID. We are still at a stage where we have to see the long-term effects of COVID on the brain and behaviour, on personality changes and mental illness, and the potential recovery. There is more need for psychologists to get involved. We know that there is an increased rate of mental illness, particularly among older adults, who contracted COVID. So the involvement of psychopharmacology is crucial.”
Dr. Velikonja suggests that there are other ways medications can be studied, especially as we learn more about the effects of COVID, both short-term and long-term.
“Medications may be able to be repurposed to deal with things like the fatigue, what people talk about as the brain fog, the stuff that comes with what they call ‘long COVID’. When people have a lack of energy or physical motivation to do things, there’s probably some targeting that can be done in that domain.”
These past two years have seen a mobilization of scientific expertise the likes of which the world has rarely, if ever, seen. Experts from virtually every scientific discipline have come together to deal with every aspect of the pandemic, and interdisciplinary and cross-disciplinary work is at an all-time high. Psychopharmacologists are used to working in an interdisciplinary way, and bring an enormous breadth of expertise to that scientific table. Dr. Velikonja sees their involvement in this enormous effort as essential.
“I think it’s crucial from many perspectives, in that everybody’s talking about the next big wave, which is the mental health wave. We know that there are a lot of challenges in the field of psychiatry, in terms of the number of practitioners who are available. I think psychologists are well-positioned to be in that role, to work with psychiatry to look at prescribing and the integration of behavioural strategies. We will need all hands on deck as the wave of mental health issues is unfolding.”
That wave is unfolding now, as we see more instances of domestic violence, an increase in rates of depression, anxiety, and trauma, and more problems with substance use. What this wave will look like a few months or a few years from now is anyone’s guess. But when that time comes, it will remain an “all hands on deck” situation. And we can feel a little better knowing that some of those hands will belong to the people who have spent years becoming experts in their various fields. The scientists for whom learning just one thing is not enough, who want to learn more and more. You know - the keeners.

Dr. Kerry Mothersill

Dr. Kelsey Collimore

Dr. Stephanie
Greenham
Dr. Kerry Mothersill, Dr. Kelsey Collimore, and Dr. Stephanie Greenham, Psychologists in Hospitals and Health Centres
Many psychologists work in the public health system. Some in hospitals and others in different health centres as part of interdisciplinary teams seeing patients of all kinds. Drs. Kelsey Collimore, Stephanie Greenham, and Kerry Mothersill give us some insight into the work they do.
Psychologists in Hospitals and Health Centres
“My suggestion to my friends, family, and people on the street, is to drive carefully. Look both ways before you cross the street. Eat your Wheaties and take your vitamins.”
I’m speaking with Dr. Kerry Mothersill in September 2021. Alberta is still in the middle of their fourth wave of COVID, the Delta wave. Omicron has not yet been discovered by scientists in South Africa, and Alberta ICUs are already at their limit. Dr. Mothersill is issuing this warning because he doesn’t want anyone to get into a car accident, show up at the Emergency door of the nearest hospital, and be turned away because they are at capacity.
“ICUs and other hospital-based services are under a significant crunch, and though I tend to be optimistic I’m not so optimistic to think that within 18 months we’ll be out of a pandemic situation. The difficulties we’re experiencing at the moment tend to get lost down the line. It’s important to be informed and to base our decisions on the best evidence we have. It’s important that we all be mindful right now of the challenges in the healthcare system.”
It is now February 2022, and Dr. Mothersill’s comments seem particularly prescient. Alberta is now putting together field hospitals in Calgary and Edmonton in preparation for an expected surge. Although this will mean additional beds, health-care workers are unsure they will have enough staff to manage them. Dr. Mothersill is mainly in private practice now, but is still heavily involved with the public health system, training residents within Alberta Health Services.
The pandemic has been stressful on everyone, but no one has been affected more than health care workers in hospitals. Many psychologists who work in hospitals have been working overtime trying to help their colleagues cope with the overwhelming and unending toll the pandemic has taken on them. But not all hospitals are the kind that are being overwhelmed with COVID patients.
Dr. Kelsey Collimore is a psychologist working in the Mood and Anxiety Disorders Program at the Royal Ottawa Mental Health Centre and a Clinical Investigator with The Royal’s Institute of Mental Health Research. The Royal is a specialized mental health centre that provides tertiary care to individuals with complex and treatment resistant mental illness and/or substance use issues. Dr. Collimore says the pandemic has affected her program much differently than many other general hospitals – mostly in the shift to virtual services.
“Virtual care was something that was in place at The Royal prior to the pandemic. Of course it has really been propelled forward across all of health care as a result of COVID. I think the shift toward telemedicine has been somewhat helpful, in that now we have a better understanding of where we might want to continue with some of those services. I think there’s a real place for them going forward. As of now, we have returned to some in-person services, but most are still primarily virtual.”
Dr. Stephanie Greenham, the Chair of the CPA’s Psychologists in Hospitals and Health Centres, is a clinical psychologist working at CHEO – a pediatric health and research centre in Ottawa, where she is the professional practice leader and coordinator for psychology. She is also a psychologist and clinical lead with the inpatient mental health unit. With so many children experiencing the pandemic in ways that affect their mental health, CHEO has certainly been busier over the past two years. So what kind of services does CHEO provide, and how do psychologists factor in? Dr. Greenham gives an example.
“We have a specialty service that provides outpatient care for children and youth with complex chronic pain that integrates care from the physical, psychological, and pharmacological perspectives. Psychologists play a key role in program development and evaluation. The multidisciplinary team involves physicians, nurse practitioners, psychiatrists, psychologists, social workers, physiotherapists, occupational therapists, and pharmacists. They work collaboratively with children, youth, and families to provide a multidisciplinary assessment and interventions. That could be individual or group interventions run by psychologists or other members of the team, family therapy, follow-ups with physicians, and medication management. It’s very much a team offering!”
The Royal provides a much different type of care, primarily geared toward adults. They work with a particular client population or a particular group of clinical disorders, for assessment and treatment. They also place a large focus on evaluation and an increasing focus on clinical research integration. The people Dr. Collimore sees are often those for whom traditional treatments haven’t worked.
“I work with adults with a range of depressive disorders, bipolar and related disorders, traumatic stress or anxiety and related disorders. Most often I work with individuals who historically haven’t responded to various treatments and have had their symptoms for quite some time. Often I work with clients who have a more complex clinical presentation – meaning that they have more than one difficulty with a lot of stressors to consider within the context of service delivery.”
Psychologists who work in hospitals have a certain kinship with one another, which is why the CPA created the Hospitals and Health Centres Section. Dr. Mothersill, who practiced in hospitals for about 40 years in Ottawa and Calgary, is one of the founding members of the section.
“There were a number of us who felt there were particular challenges and opportunities for psychologists who were working within the publicly funded health care system. People working outside of industry, outside of private practice, outside of government. We created the section to discuss issues that were pertaining specifically to practice within hospitals and various health care clinics.”
Today’s Chair, Dr. Greenham, explains that while initially the section was made up predominantly of psychologists working out of hospitals, that makeup has changed over the years.
“Members of this section include psychologists working in rehab centres or other types of treatment centres affiliated with public health. They’re clinical psychologists, health psychologists, neuropsychologists – who happen to be working in the public health system.”
Dr. Mothersill says there are a few reasons this shift has happened.
“Things have evolved in publicly-funded healthcare over the last several decades, so as much healthcare as possible is being delivered outside hospitals – in urgent care centres, clinics and the like. There is a continuum of care that’s provided from very intensive in hospitals to less intensive outside with which psychologists are involved.
Up until maybe ten years ago, most emerging psychologists coming out of grad school, especially those who specialized in clinical psychology, neuropsychology, or health psychology, had a desire to work in a hospital setting or a publicly funded health system of some sort. I think in the last decade, and increasingly so, this is no longer the case. A growing percentage want to enter directly into the private practice field. There has been a growing number of large private practices, where many psychologists can work and consult with one another. I think this poses some challenges for publicly funded systems to attract and hold onto psychologists within that system.”
Dr. Greenham points to another place that is attracting psychology grads – primary care.
“I think there are increasing opportunities for psychologists in communities to get involved at the primary care level, where they’re becoming embedded within primary care practices with primary care physicians and interdisciplinary practices within the community.”
The more psychologists are involved with primary care, and with clinics and therapy centres and multidisciplinary teams across Canada, the more involved they are in every facet of public health. And the stronger their voice will be when they give advice like;
“Drive carefully. Look both ways before you cross the street. Eat your Wheaties and take your vitamins.”

Dr. Jude Mary Cénat

Dr. Helen Ofosu

Anita Shaw
Dr. Jude Mary Cénat, Dr. Helen Ofosu, Anita Shaw, Kafui Sawyer, Dr. Erin Beettam, and Dr. Monnica Williams, Black Psychology Section

Kafui Sawyer

Dr. Erin Beettam

Dr. Monnica Williams
One of the two new sections at the CPA is the Black Psychology Section, which looks to increase the presence of Black professionals in psychology and to increase access to mental health services for the Black community.
“What field can be more anti-racist than psychology? We are here to promote human beings, human development, and human well-being! There is no field that can address racial issues better than psychology.”
Dr. Jude Mary Cénat is passionate about making psychology anti-racist, and inviting his colleagues in the mental health field to join the movement. Dr. Cénat is an Associate Professor in the school of Psychology at the University of Ottawa, and the director of the Vulnerability, Trauma, Resilience and Culture Research Laboratory (V-TRaC Lab).
Canada’s racialized populations experience unique traumas and mental health concerns. Black Canadians are no exception. In addition to the things that affect everyone – the pandemic, work stress, family issues – they must contend with societal racism and workplace hostility/microaggressions that remain a fact of everyday life in this country.
“We cannot continue to perpetrate and encourage racial discrimination. We cannot continue to be ‘colourblind.’ People who experience high levels of racial discrimination are thirty-six times more likely to present with severe symptoms of depression.”
The effort to make sure psychology leads the way it can, and should, in addressing racial issues is one of the principals that led five CPA members and affiliates to become the driving force behind the creation of a new Black Psychology Section at the CPA. Kafui Sawyer, Anita Shaw, Dr. Helen Ofosu, Dr. Monnica Williams, and Dr. Erin Beettam see the mission of the section as promoting and advancing practitioners, educators, students, and scientists of psychology who identify as Black and who are concerned about psychology-related issues that impact Black people. Each of them has seen that impact, some personally, in their own careers.
Dr. Helen Ofosu is an Industrial/Organizational psychologist, Executive Coach, and HR Consultant in Ottawa. She works with organizations including government departments, to improve organizational culture and inclusion. Over the past two years, during the pandemic, she has noticed a lot of racialized employees choosing to find work within more inclusive organizations, as they are realizing that working from home, they are no longer subjected to the everyday indignities they experienced in a physical workplace. “These things have been happening for years, but now people are removed from that environment, and they have the peace of mind that comes from doing their work without worrying about microaggressions, or getting the side-eye, or being excluded from lunches, coffees, and conversations. When all of that is gone, people feel so much more relaxed because they can just focus on doing their work.
I think the real trigger was in the summer of 2021, when a lot of organizations were planning their return to the physical workplace. It was only when people started to realize ‘oh my goodness – I might have to go back to the office’ that they started thinking ‘wait a second – I don’t think I can go back to the office. I don’t want to go back to the office! I don’t want to go back to the way things were.’
During all that reconsideration, a lot of people figured it was a smart time for them to find a different place to work, where there’s more representation, more inclusion, more diversity, and just a better workplace culture. From what I’ve seen, people are reflecting on a lot of things during the pandemic. So, they’re looking for a way to find employment where they can just be themselves, and focus on doing their work instead of focusing on self-protection from all these emotional assaults.”
Anita Shaw is a PhD student at the University of Northern BC in Prince George. She says,
“While I’ve been doing my PhD, I’ve also been really thinking about decolonization. Not only decolonizing my own thinking, but about how psychology has contributed to colonization, and how it could contribute to decolonization. I’ve been working with a mentor who is an Indigenous scholar, and we’ve developed a template for a course curriculum for decolonizing psychology.”
Kafui Sawyer is a psychotherapist, a trauma consultant for Health Canada, and the Clinical Director for Joy Health and Research Centre. She helps families through traumatic experiences, assists government employees who have suffered as a result of experiences (such as racism) in their workplace, and much more. Often clients will ask to work with her specifically, because she is Black and shares a lived experience with those clients. She says that the most rewarding thing for her is working with complex cases like personality disorders, as clients transition from a disordered personality to a more grounded place.
Ms. Sawyer notes that the Section founders’ hope is “to create a space where people with similar values and beliefs can make things work. We hope it brings like-minded people together so we can have a home in the CPA.” For the founders, the Section is an opportunity to create a space where people can bring common their interests and experiences together in a way “that empower us to be better.”
The Black Psychology Section is an important space for allies of Black members, students, and affiliates as well. Dr. Erin Beettam identifies herself as a Child & Adolescent Clinical Psychologist. While she trained in School Psychology, her work has primarily been in hospitals, pediatric psychiatry, and the public mental health system. Erin specializes in treating adolescents and young adults in anxiety, depression, emerging personality disorders, and eating disorders. Presently she works in a school board and has a private practice. She notes her growing awareness “of the lack of available and effective services for people of colour, for Black communities, in the workplace, and in educational settings”. This awareness has led her to examine what she “can give and do to provide support in the changing landscape.”
Dr. Monnica Williams is a researcher at the University of Ottawa who has long been an advocate for inclusivity in research. For too long, people of colour have been excluded from research of all kinds, notably in a variety of psychological fields.
“So much of the research we see is exclusionary, and it not only perpetuates the problem but it’s also a symptom of the problem. Part of the issue is that we don’t have enough researchers of colour to do the research for people of colour.
I do a lot of research bringing these issues to light – how treatments might need to be adapted for people of colour, how therapists who are getting trained now can learn more about how to treat people with a more inclusive lens. Everybody needs to understand best practices when working with race, ethnicity, and across cultures.”
It is these best practices when working with race, ethnicity, and across cultures that Dr. Williams’ colleague at the University of Ottawa, Dr. Cénat, is promoting as well. He and his colleagues have created a course called ‘How To Provide Antiracist Mental Health Care’, approved for Continuing Education credits by the CPA. Dr. Cénat hopes that all mental health professionals, and Canadians by and large, become committed to anti-racism.
“As Ibram Kendi said, there is no ‘racist’ and ‘non-racist’. There is racism, and anti-racism. If you are just ‘non-racist’, you aren’t taking actions that can push back against racism. And you have to take action against racism because that is how we can create an anti-racist society.”
The Black Psychology Section, approved by the CPA Board in November 2021, is now accepting members. Once membership is established, the Section will propose its Terms of Reference to the CPA Board for approval and then go on to elect its Executive; all steps which should be completed in 2022. The Section’s purpose will include working with others to increase the presence of Black professionals in psychology and to increase access to mental health, wellness, organizational, and consultation services for the Black community; especially those who experience unique barriers to accessing appropriate mental health care and other psychological services (e.g., training, leadership, organizational interventions, basic and applied research, etc.). The Section may ultimately become a community space for CPA members, students and affiliates interested in these issues and, especially for Black students, educators, researchers and practicing psychologists. For more information about joining the Section, go to https://cpa.ca/sections/black-psychology/
 Dr. Monnica Williams
Dr. Monnica WilliamsFebruary is Black History Month, and the CPA is spotlighting contemporary Black psychologists throughout the month. Dr. Monnica Williams is a researcher at the University of Ottawa, dedicated to making research more inclusive for people of colour. In particular, at the moment, research into psychedelic medicine.
Dr. Monnica Williams is a therapist, author, and researcher at the University of Ottawa (among many others in a very long list of credentials). She has a long history of advocacy, activism, and social justice work, and has specialized in racial disparities in health, research, and elsewhere. An expert in anxiety disorders, she is currently one of very few researchers focused on the inclusion of people of color in psychedelic medicine.
“A lot of my research has been around the experience of trauma, and particularly trauma for racialized people – trauma that comes about from experiences of racism, and how we can best help people who are suffering. When it came to my attention 6 or 7 years ago that this research was going on into MDMA for the treatment of PTSD, I was really interested. Number one – does it work? Looking at the clinical trials and the research that was coming out it seemed to be very effective. And number two – will it work for people of colour? It was quite clear that while the research was promising, it was not inclusive.
Seeing millions and millions of dollars being poured into this novel treatment approach, which I think is really going to be a game-changer for mental health, and at the same time realizing that people a colour aren’t a part of it, that made me concerned – a little angry, actually. This is good enough for white people, why aren’t we getting any of it?
So I set out to research this so we could quantify the degree of exclusion we were experiencing. I was also hoping this could act as a call to action – to bring awareness to the fact that we need to be included and our voices need to be heard, and that treatment approaches have to be tailored to our communities. Not just what we might think of as a generic white middle class client, but there’s a whole spectrum of people who might benefit from these treatments.
It’s also important to note that not only have a lot of these psychedelic medicines been stolen from Indigenous cultures, and some of the methods have been stolen from Indigenous cultures as well. So we have to be cognizant of that when we approach this research.”
Dr. Williams has long been an advocate for inclusivity in research. For too long, people of colour have been excluded from research of all kinds, notably in a variety of psychological fields.
“So much of the research we see is exclusionary, and it not only perpetuates the problem but it’s also a symptom of the problem. Part of the issue is that we don’t have enough researchers of colour to do the research for people of colour. Certainly, there are a lot of white people who do research on these populations, but we have to be included too. As the saying goes, ‘nothing about us without us’. So the research community has to represent us, and we have to be included in it.
One of the big things that I’m advocating is more inclusion – opening the doors to our educational establishments to therapists of colour, and underscoring the need for us to be included. I also do a lot of research bringing these issues to light – how treatments might need to be adapted for people of colour, how therapists who are getting trained now can learn more about how to treat people with a more inclusive lens. Even the few therapists of colour who are coming through are being taught how to treat white people. So everybody needs to understand best practices when working with race, ethnicity, and across cultures.”
Dr. Williams says that through school and afterward she was unable to find a Black mentor in her institution, and for this reason it’s very important to her to mentor as many students as she can who find themselves in the same position as she was in school.
“I do a lot of mentoring of students of colour, because I have not had that kind of mentorship. When I was a junior psychologist, when I was first starting out, the person who was supposed to be mentoring me was actually quite abusive. So I went outside the institution and found my own mentors in the Delaware Valley Association of Black Psychologists. I worked with someone there, and it was good – it wasn’t exactly a fit in terms of the work that I did and the things they did – but I was just so happy to have Black people who were supporting me, encouraging me, and who believed in me. It was so different from my actual environment, and that made a big difference.”
Unfortunately, to this day not every institution has an environment that is inclusive of Black students or professionals. This is why Monnica turned elsewhere when she was a junior psychologist, and it’s why people of colour often look to turn elsewhere today. Creating those inclusive spaces is part of her life’s work, and something toward which the rest of Canada – in institutions and out – can strive.

Dr. Vinay Bharadia

Dr. Kristina Gicas
Dr. Vinay Bharadia and Dr. Kristina Gicas, Clinical Neuropsychology Section
Your brain and your body have a relationship – sometimes it’s a harmonious one, other times it’s contentious. This is the domain of clinical neuropsychology. We spoke to Dr. Vinay Bharadia and Dr. Kristina Gicas to learn more.
The word “neuropsychology” is a mouthful. It feels like one of those words you might use when you want to seem smart. Like “nomenclature”, or “cumulative”. Because it takes so much time to say, neuropsychologists have come up with a clever way to shorthand the term – they say “neuropsych”. Leaving out the last two syllables has, over the decades, undoubtedly saved countless cumulative hours in university department conversations across Canada.
Add the word “clinical” and you’re in a whole new world of nomenclature. One which Dr. Kristina Gicas, Chair of the CPA’s Clinical Neuropsychology Section, is happy to unpack. Dr. Gicas is a clinical neuropsychologist and an assistant professor at York University, where she trains clinical neuropsych students. She teaches, does research, and also does some clinical work in Toronto. She says,
“Clinical neuropsychology is the study of the relationship between your brain and your behaviour. We look at the structure and function of the brain, and study how that relates to thinking abilities. This includes things like attention, memory, language, visual skills, processing speed and even emotional functioning.”
Neuropsychologists are experts in investigating these brain-behaviour relationships, and using that information to do a number of things. The number one thing they do is diagnosing things like injuries or diseases that are affecting the brain (concussion, stroke, tumors, dementia). They also seek to understand normal human development and aging. Another area of specialty of neuropsychologists is in designing and implementing interventions to improve peoples’ day-to-day functioning.
The CPA calls the section Clinical neuropsychology because all neuropsychologists are trained as clinical psychologists first. The neuropsych part is a specialization, where practitioners take additional courses – for example, doctorate courses in neuroanatomy (another mouthful of a word – only this one has no convenient contraction). They learn about assessment tools and cognitive tests – what they mean, how they’re used. Most psychologists can administer these tests, but it’s neuropsychologists who can link them to brain functioning – that brain-behaviour relationship.
Maybe you’ve noticed that one of your parents is starting to become more forgetful, and is less able to pay attention to tasks than they once were. You might take them into the doctor, who might then administer a test to them – like the MoCA (Montreal Cognitive Assessment) test. This is a preliminary screener that can help determine the degree to which intervention is needed. If your parent meets a certain threshold, they might be referred to a clinical neuropsychologist like Dr. Vinay Bharadia.
Dr. Bharadia splits his time between a private practice, as Lead of Neuropsychology at TELUS Health Care Centres in Calgary and the University of Calgary where he trains PhD and Masters level psychologists.. He works mostly with brain injuries, dementia, Parkinson’s, Multiple Sclerosis, and other neurological conditions that affect cognition. He says,
“If you get referred to us, we do more robust testing of memory and attention and other cognitive areas, after a screener from your GP like a MoCA. We also look for depression and anxiety, as those can affect cognitive ability as well. We then relate the tests we do to the hippocampus, or the thalamus – brain parts that we know are related to memory, or other areas and neural networks. We look at your medical history, your MRIs and CT scans and so on, and we put it all together and look to get a diagnosis or treatment moving forward.”
A lot of the research done by cognitive scientists – like Jonathan Wilbiks in the Brain and Cognitive Sciences Section (see earlier Psychology Month piece) informs the work done by clinical neuropsychologists. The cognitive scientists come up with research and data, and it’s then up to clinical neuropsychologists to apply that knowledge in a clinical setting to enhance the lives of their patients. And those patients vary a great deal depending on their condition, their symptoms, and their age. Says Dr. Bharadia,
“If you’re a 25-year-old presenting with symptoms of depression, you’re probably not going to see a neuropsychologist. You’re more likely to see a clinical psychologist, or a counselor, and maybe a general practitioner (GP) for medication. But if you’re a 55-year-old with depression, hopefully the GP is thinking ‘what else could this be? What else looks like depression in your 50s?’ With a few other factors in your medical history and things you might see on an MRI, it could be a symptom of Frontotemporal Dementia, which can look like depression in certain age groups. At which point they might be a good candidate for testing with a neuropsych to refine the diagnosis.”
This means neuropsychologists work a lot with GPs, psychiatrists, neurologists who are doing MRIs, and many other professionals in the world of brain science all of whom have overlapping expertise. If the 55-year-old with symptoms of depression meets with this team, they may determine that the cause is neurological – in which case they will suggest one treatment path. If, however, they determine the cause is psychological, a neuropsychologist is trained (remember – they are clinical psychologists first) to work with the person to heal.
Neuropsych as a formal field is 70 years old. The seminal work of Dr. Brenda Milner at McGill in the 50s with patient H.M. was groundbreaking in our understanding of memory. This revolutionary work was done alongside neurosurgeon Dr. Wilder Penfield. Dr. Milner is STILL PRACTISING at McGill at age 102. Some other pioneers set up a neuropsychology program at the University of Victoria, where Dr. Gicas did her undergrad. This, (along with her fascination with the brain and fervor for science in general) led her down this path. She says,
“I remember reading a book by Oliver Sacks, called The Man Who Mistook His Wife For A Hat (1985). It’s a series of neurological kinds of cases and I was just hooked after that.”
In an episode of Parks and Recreation, Ben can’t understand the relationship between Jerry (Jim O’Heir) and his noticeably better-looking wife Gayle (Christie Brinkley) and speculates that it is as a result of a neurological disorder (“one of those Oliver Sacks disorder thingies – like maybe she thinks Jerry is a friendly hat?”). It may not be the best example of neuropsychology in popular culture, in that it gets it quite wrong – but it isn’t that easy a study to get right! That is, unless you can circumvent the cumulative effect of all the difficult nomenclature.

Dr. Karen Blair

Dr. Rhea Ashley
Hoskin

Bre O’Handley
Dr. Karen Blair, Dr. Rhea Ashley Hoskin, and Bre O’Handley Sexual Orientation and Gender Identity Section
The field of Sexual Orientation and Gender Identity in psychology has come a long way in the last few years, from securing same-sex marriage rights to banning conversion therapy. We spoke to Dr. Karen Blair, Dr. Rhea Ashley Hoskin, and Bre O’Handley about that progress, and about a term you may not have heard before – “femmephobia”.
Sexual Orientation and Gender Identity
“I don’t like beer anymore”
There’s a commercial running on TV where a guy confesses to one of his buddies, in an ashamed whisper, that he no longer enjoys the taste of beer. There is an implicit understanding between us, the viewers, and the guys in the commercial, that disliking beer is affecting that guy’s sense of masculinity. That enjoying beer with the boys is a part of his male identity that he is ashamed to lose. And that disliking beer makes him more ‘feminine’, and therefore less worthy, than the others.
Dr. Rhea Ashley Hoskin is an AMTD Global Talent Postdoctoral Fellow at the University of Waterloo, where she is cross-appointed to the departments of sociology and legal studies and also sexuality, family, and marriage studies. She is the secretary/treasurer of the CPA’s Sexual Orientation and Gender Identity Section (SOGI), and her work broadly looks at sexual and gender diversity – more specifically, societal treatment of femininity and “Femmephobia”.
“Femmephobia is about the way society devalues and regulates femininity, which can target anybody. It can target a cisgender man who orders a salad, or is seen somehow as being feminine – because femininity is often viewed as a social demotion. We also see femmephobia targeting women in science who might be seen as ‘too feminine’ and might be treated as though they are incompetent because they wear too much makeup or because they ‘don’t look like a scientist’.”
In the commercial, the guy’s buddy treats his announcement of no longer liking beer with a shrug and doesn’t seem to think this makes Guy One any less of a man. Then, of course, he offers him something in place of the beer – a hard liquor that we, the viewer, can infer to be an adequate replacement and equally manly in the eyes of society.
Femmephobia affects both gay and straight people, both men and women, and even those who identify as non-binary – the push and pull of defining your public persona through what is seen as feminine is something we all carry with us, mostly subconsciously. Every one of us is touched by it in some way, whether it’s men who order a regular beer instead of a light beer, for fear of seeming too ‘feminine’, or women who wear less makeup to appear more intelligent or ‘professional’.
Dr. Karen Blair is an assistant professor of psychology at Trent University, and has been the Chair of SOGI since 2014. She says,
“One of the neat things about Femmephobia is that once it clicks, you begin to see it everywhere. You start noticing all the different ways we devalue femininity. With men, we have a pretty narrow range of “acceptable femininity” – and in most cases, we prefer they have none. In the football locker room when a coach wants to insult a team, he might say they played ‘like a bunch of girls’. That’s meant to sting, and the players get the message that the coach is unhappy. If a man walks too ‘feminine’ or talks too ‘feminine’ or talks with his hands, we take him down a notch for it. We use femininity in our society as a weapon or an insult.”
With the occupation in Ottawa getting under way a couple of weeks ago, attacks on the Prime Minister increased notably – both within the group of insurrectionists and also on social media. Dr. Blair and Dr. Hoskin track this sort of thing. What do attacks on public figures and politicians look like, and how is Femmephobia so often a part of them?
“When people want to attack Justin Trudeau, they do a few things – one, they tend to call him by his first name. When we were upset at Stephen Harper, we still called him Harper. But when we’re upset with Trudeau, we use his first name – and some even call him Justine. Why should it be an insult to call someone by a woman’s name? Why is it insulting to feminize another person? The answer is misogyny and femmephobia. It’s not just politicians like the Prime Minister, we’ll do this across the spectrum. When people want to make fun of Putin, or Trump, one of the common memes on the internet is to add makeup to their faces to make them look like an overdone woman. No matter how you feel about Trudeau, Trump, or Putin, they’re all taken down with this same attack of ‘femininity’. It’s used to say they’re lesser, they’re stupid, they’re silly, they’re frivolous, or they’re extreme. All these things can be conveyed just by making them feminine. Which leaves you wondering – what are we actually saying about people who are feminine? It’s kind of like when people used to say ‘that’s so gay’, when what they meant was that something was stupid, or silly.”
‘We’ (society) have come a long way in the last few decades. When the SOGI section started it was the early 2000s, and one of the big pressing issues at the time was same-sex marriage. The extension of civil rights in Canada to same-sex couples was top of mind for many psychologists, and there is a policy statement from the CPA at that time stating our support for this notion of same-sex couples having the right to marry one another. It seems a little quaint today – like, of course we support that – but Dr. Blair says that at the time it was quite a novel and exciting statement.
“A lot of the research at the time, the early 2000s, was showing that same-sex relationships were the same as mixed-sex relationships in that they’re good for people, and healthy, and that love is love. These were the kinds of things researchers were focused on. They were trying to support policy-makers in understanding that when people are cut out of an institution like marriage, it changes the relationships they have with their family, their friends, and their coworkers. For instance, consider something as silly as holiday parties at a company where invitations are extended to include spouses. If you were a same-sex couple in 1999, it would be really unclear as to whether your partner was included, and in some cases it would be quite explicit that they were not.”
Many people at that time felt like they couldn’t talk about their partners at work or couldn’t have a photo of them on their desk. Psychologists working in this space were able to point out how things like that took a toll on peoples’ mental health and their well-being over time. Dr. Blair continues,
“A lot of research showed that families of LGBTQ people didn’t really ‘get it’. And that they really didn’t get it right up until the moment they were at the wedding. At a wedding there are social scripts that tell us when to get up, when to clink our glasses, when to applaud, and so on. Being able to put same-sex relationships into this social ritual that people understood created a situation where family and friends could understand the relationship – which then led to greater support from the inner circles of many LGBTQ individuals – which then led to greater mental well-being for the whole community.”
That mental well-being has taken a hit during the pandemic, for a variety of reasons. Bre O’Handley is a Master’s psychology student at Trent with Dr. Blair as her supervisor. She is working on a thesis that looks at LGBTQ well being during the pandemic and how supports might play a role in that.
“I’m looking at the trajectories of well-being for LGBTQ people during COVID. There’s a lot of research all over the world that has found that LGBTQ people are faring worse during this pandemic. Their mental health has been affected more, they’re reporting higher levels of depression, anxiety, and stress. Everybody’s experiencing COVID and social isolation, but there are additional factors that could impact LGBTQ people. They could be living in an unsupportive environment, especially if they’re younger. They’re being separated from affirming communities – like if you had a group of friends at school who supported and accepted you, but now you’re not going to school. The pandemic reduced access to LGBTQ resource centres. For a long time, trans people were unable to get hormone replacement therapy (HRT) and gender-affirming surgeries, as those were deemed non-essential at the beginning of the pandemic and supply chain issues delayed shipments of important drugs and hormones.”
There were even discriminatory COVID policies in a number of countries. In Peru, a rule was instituted that said men could leave the house only some days, and women could leave only on other days. This left trans people, and people who didn’t identify as either male or female, in a significant bind. Many experienced harassment and hate crimes while they were out of the house. Bre’s research doesn’t tackle the discrimination, so much as the supports that are needed for those who are on the receiving end of that discrimination.
“How do we foster resilience in these circumstances, and how are LGBTQ people coping in this pandemic? If I feel connected to the LGBTQ community, that should buffer some of the issues that affect mental health. But how do we separate that out from more general social supports? Is just having supportive people and family around you enough, or do you need that social connection with others in your peer group to truly maintain resilience? This circumstance now, with COVID, gives us a little bit of an opportunity to tease that apart.”
There is always more work to be done, and always new challenges that arise. Same-sex marriage has now been the law of the land in Canada for sixteen years. Adoption by same-sex couples has been legal in all Canadian provinces and territories for a decade. Conversion therapy is now banned, and many members of the SOGI section were actively involved in discussions with policy-makers to make that happen. Today, the focus on gender identity is catching up to the fight for equal rights for gay and lesbian couples. Says Dr. Blair,
“You can know a lot about sexual orientation and sexual minorities and still manage to know nothing about gender identity or gender minorities – and vice versa. The two came together as a CPA section when the topic of gender identity was less prevalent, and the focus was probably more on sexual orientation at that time. Over time, gender has become an equally important topic to sexual orientation within the section.”
All of us in Canadian society are learning a little bit more about sexual orientation and gender identity, just as the scientists are learning more and telling us about it. Dr. Hoskin frames this in terms of Femmephobia.
“Our ability to see femmephobia comes from the study of sexual and gender diversity. Femmephobia is illuminated by our ability to tease apart gender identity from sex assigned at birth, and gender expression. When we can see those things as different, we can see how gender expression comes into play and how it’s regulated by society.”
We all form part of that society, and how we regulate our attitudes toward the LGBTQ+ population is an enormous part of preserving and enhancing their mental health. It could be using the correct pronouns to address someone, embracing your lesbian daughter, or something as simple as stating with firm confidence,
“I don’t like beer anymore.”

Dr. Shahnaz Winer
Dr. Shahnaz Winer, Psychology Careers and Professionals Section
One of two brand-new sections at the CPA, the Psychology Careers and Professionals Section is a place to network and collaborate for those who have a psychology degree but work in an area other than clinical practice or academia.
Psychology Careers and Professionals
In June of 2014, ISIS invaded Kurdish-held territory in Northern Iraq, capturing Samarra, Mosul, and Tikrit in quick succession. Dr. Shahnaz Winer was a young single working female teaching psychology at a Middle Eastern university in the region, the place where she was born, and her family insisted she get out. She was quickly on a plane back to Canada as Kurdistan descended into turmoil and violent bedlam.
Dr. Winer reminisces fondly about her time teaching in Iraq, and says it was one of the best times she’s had in her career. She is obviously very sad about the fact that this chapter had to end, and especially sad about how it ended, but she didn’t stay down for long. She began a string of jobs dedicated to the one thing that has driven her throughout her career - the application of psychological science and knowledge to enhancing the everyday lives of…well…everybody! Through a series of jobs, in and out of academia, she ended up starting her own business. And it was as the owner of that business that she presented to students at last year’s CPA Career Fair.
Some of the most well-attended and highly-anticipated events at the CPA are the Career Fairs we have held the last few years. At these events, students have an opportunity to learn about various career paths and positions for psychology graduates outside of the health services delivery and academic settings. They were able to meet with individuals in those positions to explore the vast job possibilities available to someone with a psychology degree.
People like Sophie Kenny, who works with eye capture technology at VPixx Technologies. Or Anne-Marie Côté who coordinates virtual field trips for students in remote northern Indigenous communities with TakingITGlobal. Or even our own Deputy CEO Lisa Votta-Bleeker, whose work at the CPA certainly falls outside the realms of academia and clinical practice.
These events allow students, professionals, and other interested individuals to network with one another in a setting designed to expand the options available to psychology graduates and, indeed, to all those interested in a less conventional career path. But what if those like-minded people could network with one another year-round, instead of a few times a year at these one-off events? That was the thinking behind the creation of the new Psychology Careers and Professionals Section at the CPA.
Dr. Winer has partnered with Dr. Votta-Bleeker to launch this section. Dr. Winer has a PhD in Cognitive Neuroscience from the University of Waterloo and is one of the people in psychology who took that non-traditional career path. The business she created, Vibrant Minds, is an online education platform where Dr. Winer takes principles of psychology and combines them with other interests. She creates digital products that help people plan, set, and achieve their career and life goals.
“The one thing that I love is that I’m able to reach an international audience of students with this. I can connect to so many different people, and to help them apply what psychology teaches us and what academic research has discovered.”
Dr. Winer did spend some time in a traditional academic role, as a professor. She says that when she taught, she noticed the students gravitated much more toward one particular type of lesson.
“The sections students were really excited about were the ones where they could apply what they were learning to their own lives. For example, if we were learning about memory, we would do an entire section about applying the knowledge so they could study better and remember things for tests more effectively. So it was that application that got me really excited, and I felt like that was something that was largely missing between traditional psychology and all the other professions and fields. That bridge between the academic side and then reaching everyone else with that information.”
When this new Careers and Professionals Section starts filling out its membership, most of those members will be people who bridge that gap. They are the people who take psychological science and principles and apply them to every conceivable industry across Canada. They’re the ones making air travel safer, workplaces more inclusive, and creating high-performance buildings that minimize environmental impact. Having this new place to collaborate will bring all those diverse people together.
“This section was really inspired by the need to provide a home for those of us who, like me, have psychology backgrounds but didn’t follow a traditional path. I became a member of the CPA when I was a student, but when I left academia, I left the CPA because I thought there was nothing there for me any more. And it was actually very lonely! It had been wonderful to have that kind of community, the support, and the resources that the CPA offers. So when I was approached with this idea of a new section geared specifically toward those interested in fields outside the typical psychology fields, it sparked my interest right away!”
The Psychology Careers and Professionals Section is at the stage right now where the section has been approved, and their next task is to recruit the founding members. With 90 new members in only the first few weeks of registration, the section is off to a sprightly start. Dr. Winer has a vision for who she hopes those initial members might be, including a diverse mix of established professionals, those early in their careers, as well as students.
“We want to create a welcoming space for students who are exploring their options. This is such an important group to me because I feel like I was very privileged. When I was in grad school completing my PhD, for the first year or so all the information provided to me, all the workshops and seminars and career fairs, were all geared toward the steps to take to get into academia, or the steps to get into clinical practice. I wasn’t sure at that time what I wanted to do, but I wanted to know what options there were.
My supervisor, Dr. Myra Fernandes, really thought we should explore all the options available to us. So within our own lab, she created a seminar series where she would bring in different speakers. For example, someone with a psychology background who was working for the pharmaceutical company Eli Lilly came to speak with us. The exposure to these other options inspired me and gave me a lot more knowledge, but my friends who were in grad school at the time weren’t being exposed to this or given this other information.”
Some of the other people who have expressed interest in the section are professionals interested in networking with each other, those keen to mentor students, along with those who have gone the academic or clinical route but who have other interests. Others are doing something many psychology grads do, like research, but they’re doing it in a hospital, government, private sector, or start-up setting instead of a university and, as such, don’t feel as connected to the traditional academic side of things. Says Dr. Winer,
“There are many individuals who fall into the in-between, and that’s the great thing about this wide spectrum. We’re welcoming anyone from anywhere who wants to join and connect with this group of people who have a variety of interests.”
Dr. Winer felt lucky and grateful to have had those experiences in grad school, and to have taken a non-traditional career path as a result. In addition to serving as Dean of Social Sciences and a variety of teaching jobs and her current business, she spent some time as a curriculum developer and educator, the principal of a coding school for youth, as well as a facilitator and coordinator for the Memory and Aging Program at a group of senior homes across Ontario.
It's experiences like these that Dr. Winer wants to share with the other members of the new section – with the like-minded individuals who have chosen a different career path, and with the students who could benefit greatly from being exposed to these options they might not otherwise see. The idea is one big, long, ever-evolving and ever-growing career fair. One that creates a home for psychology graduates who might otherwise feel like they are on an island, and one that runs, collaborates and networks not just for 48 hours at a time, but 365 days a year.

Dr. Marvin McDonald

Dr. Tanya Mudry

Dr. Jessica Van Vliet

Dr. Houyuan (Hy) Luo

Dr. Janet Miller
Dr. Marvin McDonald, Dr. Tanya Mudry, Dr. Janet Miller, Dr. Houyuan (Hy) Luo, and Dr. Jessica Van Vliet, Counselling Psychology Section
Counselling psychology has many facets and many different practitioners. We spoke with five of them about what it is they do, and how it affects the lives of everyday people.
Syd Barrett created Pink Floyd in 1964, and was the driving force behind their seminal 1967 album The Piper at the Gates of Dawn. He lasted for only one more album, A Saucerful of Secrets, before drug use and mental illness led to his departure from the band. He then hid from public life, obsessively guarding his secrecy for 35 years until his death in 2006.
Counselling Psychology might well be the Pink Floyd of CPA sections, in that they insist on having five members on stage at all times. A collaborative and inclusive discipline, it makes sense that when I asked to interview the CPA’s counselling section, a full five-person panel showed up.
Dr. Marvin McDonald is a professor at Trinity Western University in BC. He’s the Syd Barrett of the group (in that he was there from the start – he has lasted far longer than two albums), the Past Chair who helped get this section to where it is today. Dr. McDonald has a little more experience than the others, and has certainly seen the evolution of the discipline. He says,
“When I went through my doctoral studies in the US in the 80s, the ethics course was an option! It was not a required course - just to give you a very concrete example of how things are different today. The good thing about this transition over the years is that the professional standards have corresponded with empirical evidence. When I started my early psych pathology course, the data from community-level surveys for mental health needs had not yet been pulled together. There was still an active question in the literature about gender differences in mental health needs. It wasn’t until the late 80s and early 90s that the data demonstrated clearly that more women than men sought help, and that men had higher rates of substance use and addiction. These are the kind of understandings that have advanced counselling psychology in recent decades, and they affect practice greatly, not just on the research side.”
Dr. Tanya Mudry, professor of psychology at the University of Calgary and a counselling psychologist with a few clients in private practice, is the new Section Chair. She is the David Gilmour of the group, in that she replaced Dr. McDonald – and in the sense that she keeps the group moving forward with a definite sense of purpose. She describes Counselling Psychology as
“A pretty diverse group. We tend to work in communities with families, children, and couples. We often work with people who might be struggling with life transitions – maybe having family problems or marital problems – and with people who have mental health issues or substance use disorders. We tend to take a diverse perspective – many psychologists will lean toward a particular method of doing therapy, whereas counselling psychologists are more all over the map. Some like to think about your past, and how you grew up. Some like to think about your social context or what’s happening inside your brain, and still others are focused on social justice issues and advocacy.”
Dr. Janet Miller is the Richard Wright of this Zoom call (Wright was the keyboardist for Pink Floyd, known for his skill with a variety of instruments and for the syncopated jazz rhythms and melodies he brought to the music). Dr. Miller works at Mount Royal University in Calgary, but not as an instructor. She’s a full professor in Student Counselling, and also has a private practice in the city. She brings an improvisational jazz style to the conversation, when asked how counselling psychology might affect the everyday life of someone who is not, themselves, in counselling.
“Maybe you’re walking up to the till at the grocery store, and you are unaware that the clerk had just come from a counselling session where they had processed their social anxiety so they could have that job and be front-facing and manage public interactions! They learned how to be in their body, they were able to be centred, and they were able to put anxiety to the side for a little while so they could experience people. Maybe they had some coping mechanisms that they employed so that when you arrived to pay for your groceries you had a smooth interaction. You were able to enjoy the process of buying groceries, and they were able to enjoy their work and go home with some energy to their beautiful family.”
Nick Mason is the only member of Pink Floyd to appear on every one of the band’s albums. The percussionist, he is emblematic of the Floyd sound throughout the band’s history and wrote some of their greatest songs. The Nick Mason of this group is Dr. Houyuan (Hy) Luo, the classic definition of a counselling psychologist. He has a private practice in Toronto and is the Chair-Elect of the Counselling Psychology Section. Dr. Luo says that while the pandemic has made providing counselling more challenging in certain ways, many of his clients are embracing the new delivery method.
“I have been providing 100% virtual counselling since March of 2020. I work in downtown Toronto, in among the skyscrapers, and a lot of people were not yet back at their offices. They actually preferred online counselling because it was easy, and convenient for them. Now that more people are vaccinated, they are slowly returning to the office and the expectation is that we will gradually start offering in person counselling too.”
Dr. Luo is interested in expanding the field of counselling psychology to include more people of colour, as there is a real shortage of psychologists who can share lived experience with their clients who may come from different backgrounds.
“In Toronto where I work, it’s a city with so much diversity. When clients want to work with a psychologist who shares the same ethnic background, they struggle to find one, even in Toronto. We really need to help BIPOC undergrad students, as soon as they get into University, to make sure they’re being supported along the way.”
Also very interested in social change, also an advocate for social justice, is Dr. Jessica Van Vliet, the Roger Waters of the group. Roger Waters, the bassist and primary songwriter for Pink Floyd, is the member who moved the group in a more explicitly socially conscious direction (think The Wall). Dr Van Vliet, a professor at the University of Alberta in Counselling Psychology, says the biggest shift recently in counselling psychology is toward social justice.
“Social justice has always been important in counselling psychology, but now more than ever. It’s now really in the forefront of what we do. We’ve always had a focus on diversity, but now more than ever I think our discipline is taking a leadership role in the area of working across cultures and with diverse peoples, issues and methodologies. I also think leadership and advocacy are becoming more highly valued and more in focus in our field.”
For the time being, the biggest issue in Counselling Psychology – and in virtually every other industry, profession, and psychological discipline in the world – is COVID. It has increased the demand for counsellors who can help people with burnout, depression, hopelessness, and all the other mental health issues that have arisen as a result of the pandemic. We recorded this Zoom call in October of 2021, and Dr. Mudry’s thoughts at that time seem prescient.
“One of the areas where counselling psychologists are going to be instrumental is in the recovery from COVID. I’ve recently been involved in some work around burnout among critical care workers, and I think that’s going to be huge. In Alberta in particular and across Canada, our health practitioners are super burnt out. Also families and individuals struggling with having to work from home, a lack of social interaction, our kiddos are struggling with going into and then out of school. Counselling psychologists are going to be super busy in the next couple of years.”
How will Counselling Psychology, specifically, help with burnout and all these other issues? Dr. Van Vliet sums it up thusly,
“Part of what we do is we change the dialogue in peoples’ minds. We help shift that dialogue from ‘what’s wrong with me?’ to ‘what’s right with me?’ That strength focus, that positive piece of counselling psychology is a huge strength of our field. I think it has had a major contribution to how people regard themselves, other people, and their world.”
Very few, if any, people know what Syd Barrett did for the final 35 years of his life. In the late 70s, Roger Waters saw him in the department store Harrod’s in London. Barrett noticed Waters, dropped his bags, and ran out of the store. It was the last time any member of Pink Floyd saw their founder. We know that he became an avid gardener, and dedicated himself to painting, but that’s about it. One hopes he was mostly okay for those final years, and that he was able to work through some of his turmoil with a professional who could help make things a little better. A professional like, for example, a counselling psychologist?

Dr. Jenna Boyd

Dr. Rachel Langevin
Dr. Jenna Boyd and Dr. Rachel Langevin, Traumatic Stress Section
Traumatic Stress shows itself in more than just PTSD, and can be caused by more than just major single events. Dr. Jenna Boyd and Dr. Rachel Langevin are working to help those affected by trauma, and working to learn more about traumatic stress as they do.
“In the 80s and early 90s, there was nothing known about the victims of child sexual abuse. Now, there are volumes of research on the subject.”
Dr. Rachel Langevin is an assistant professor of counselling psychology at McGill University, as well as a clinical psychologist who does a bit of private practice. She is currently the Chair-Elect of the CPA’s Traumatic Stress Section. She says her PhD advisor was one of the pioneers in researching the sexual abuse of children in Quebec and Canada. At the time she decided to work on this, it was a reality that many people didn’t even recognize existed. The first step had to be acknowledging, socially, that the sexual abuse of children DID exist, and that often it happened within families. It may seem difficult to imagine now, but it took a very long time for this kind of abuse to be recognized as real in the public at large.
“In the early 80s, some researchers in the States, like David Finkelhor, started trying to really understand child sexual abuse and the specific impact it had related to other traumatic experiences. One of the first to start working on it here in Quebec was Martine Hébert, who was my PhD advisor. Her advisor had been a specialist looking at perpetrators of sexual abuse, but not victims – and Dr. Hébert was the only one looking at that side. She did her research with a lot of autonomy, because no one else had that expertise!”
Today, child sexual abuse is one of the most-studied types of child maltreatment. Research into traumatic stress has come a long way in a short time. Dr. Jenna Boyd is a psychologist at an anxiety treatment and research clinic at St. Joseph’s Healthcare Hamilton, and an assistant professor in the department of psychiatry and behavioural neuroscience at McMaster University. She is the current Chair of the CPA’s Traumatic Stress Section, and specializes in the treatment of Post-Traumatic Stress Disorder (PTSD).
“Cognitive Behavioural Therapy (CBT) is my main area of practice. A little more than 20 to 30 years ago, the main therapies that we’re using now were just emerging. From the perspective of treating PTSD, there was almost a thought that we couldn’t really treat it, but we could kind of help people cope with it. Today, we do have some really effective treatments.
Potentially traumatic experiences are pretty common. Over the course of their lives, most of us will be exposed to a traumatic event. It could be the death of someone close to us, a serious injury, sexual or intimate partner violence, or a frightening near-death experience. For some of us, it’s part of our jobs – a first responder or someone in the military could be exposed to a traumatic event more than once in a day. ‘Traumatic stress’ is what comes about as a reaction to that trauma.
It’s quite normal to have a stress-based reaction to a traumatic event or series of events. Most people who are exposed to one will have some kind of stress-response as a result. Many people will recover over time through a process of natural recovery, but others may go on to develop PTSD. This is where the symptoms related to the trauma persist over a longer period of time. Dr. Langevin says those symptoms can be multiple, complex, and varied.
“We encounter many different symptoms in this line of work. Re-experiencing symptoms, like nightmares, intrusive memories. Someone might be doing something and suddenly an image pops into their head causing distress. Every time they’re exposed to something that might resemble the trauma they endured, or something that makes them think about it, they will have a stress reaction, and anxiety will rise up. That might lead them to the second category of symptoms, which is avoidance. People start avoiding things that remind them of the trauma because it’s too stressful and uncomfortable.
The third big category of symptoms is a change in cognition, mood, and self-image. This includes things like self-blame, taking an overly large share of responsibility over what happened, feeling disconnected from others, or feeling no emotion whatsoever. And finally, there are arousal and reactivity symptoms. This is a more physiological response, and includes things like always being on your guard and looking over your shoulder, being very easily startled, difficulty sleeping, irritability, and possibly self-harm behaviours.”
When a clinical psychologist specializing in trauma sees someone who presents with a cluster of these symptoms, that persists for a month or longer after the traumatic event, and those symptoms are affecting that person’s life, that’s when they start talking about something like PTSD. At that point, it is no longer a normal reaction, and it requires attention. As Dr. Boyd says, there are now many ways that attention can be delivered.
“We now have Cognitive Processing Therapy, Prolonged Exposure Therapy, Eye Movement Desensitization and Reprocessing (EMDR) to name just a few. These treatments have had a lot of research supports behind them over the past 20 or 25 years. We now know they’re really effective for many people, and we have tools where we can say ‘let’s try this and see if we can get you to a place where you’re functioning better’. Many people can return to some of the things in their lives that have been taken away from them.”
Treatments are always improving, clinical psychologists are always innovating, and researchers are continually expanding our understanding of trauma, stress, and the interaction of the two. Dr. Langevin’s current research is looking into the intergenerational continuity of family violence, including child maltreatment and intimate partner violence.
“We know that a parent who was maltreated in their childhood is at increased risk of having a child that will also experience trauma and maltreatment – whether or not it’s at their own hands. Sometimes the mistreated parent becomes a perpetrator of abuse, and other times that doesn’t happen but the child still ends up being mistreated by someone else in the environment. There’s this continuity that we see in the data and in clinical practice, but the mechanisms that are responsible for this – the protective factors, the risk factors that are involved – are still trying to be understood. What makes one parent end up in a cycle where there is repetition of their own maltreatment history with their child, versus parents who are able to break those cycles? We’re looking to help parents who have been in this situation end the cycle, and foster resilience and positive adaptation in their children and themselves.”
Dr. Langevin is quick to point out that treating traumatic stress, and the problems that come along with it, go far beyond PTSD. She says,
“Everything can be associated with trauma, including behaviour problems, emotion regulation, depression, anxiety, bullying, difficulties with attachment and relationship. There are a host of different areas where we can see the consequences of traumatic events. PTSD is just one part of it, there’s a lot more. And we’ve come a long way in learning about it!”
 Dr. Jude Mary Cénat
Dr. Jude Mary CénatFebruary is Black History Month, and the CPA is spotlighting contemporary Black psychologists throughout the month. Dr. Jude Mary Cénat is the director of the Vulnerability, Trauma, Resilience and Culture Research Laboratory (V-TRaC Lab), and the director of the Interdisciplinary Centre for Black Health.
“What field can be more anti-racist than psychology? We are here to promote human beings, human development, and human well-being! There is no field that can address racial issues better than psychology.”
Dr. Jude Mary Cénat is passionate about making psychology anti-racist, and inviting his colleagues in the mental health field to join the movement. Dr. Cénat is an Associate Professor in the school of Psychology at the University of Ottawa, the director of the Vulnerability, Trauma, Resilience and Culture Research Laboratory (V-TRaC Lab), and the director of the Interdisciplinary Centre for Black Health.
The V-TRaC Lab has three axes. The first is working on family, social, and cultural aspects of trauma and resilience. The second axis is global mental health – the lab has a project on different countries in Africa to document mental health problems related to infectious diseases like the Ebola virus and COVID-19. This axis also looks at gender-based violence and mental health in the Caribbean. The third concerns racial disparities in health and social services.
“We have some projects on Black mental health, and we conducted the first survey on Black mental health in Canada, as part of a major project funded by the Public Health Agency of Canada to document Black mental health and to develop and implement programs related to that. We are looking at the over-representation of Black children in the child welfare system to try to understand all the factors that create that situation and propose solutions.” In December 2021, The V-TRaC Lab revealed 13 recommendations to reduce the over-representation of Black children in the Child welfare system.
Involvement with child welfare is the number one predictor of youth ending up homeless, as well as for a multitude of other problems later on such as poverty and poor education. The over-representation of Black youth in that system means that they experience those outcomes more often than other groups, leading to a perpetual cycle
“The first factor is that professionals in the child welfare system are not trained to take into account the cultural aspects of Black families. We gather a lot of focus groups with stakeholders, and one of the things they point out is that they’re not trained enough to address cultural issues. We conducted a study that showed that more than 48% of social work programs in Universities and colleges in Ontario did not have a mandatory culture related course in 2020. There are also systemic factors such as poverty related to Black communities, and racial discrimination experienced by many in the child welfare system.
But it’s not just the child welfare system itself, it’s also the larger society. In schools, for example, teachers are more likely to call childrens’ protection services for an issue with a Black kid than they are with a white one. In Canada we have a ‘colourblind’ society, where we say ‘I don’t see your skin colour, I see your problems and I try to address those’. When you have a child with a problem in school, you can call the parents to address that. But often for white kids, teachers will address a problem directly with the parents, whereas they might call child welfare directly for a Black child.”
The idea of a ‘colourblind’ society is akin to having a ‘non-racist’ society. It is a passive way to approach race, where just not laughing at the racist joke, or not participating in a discriminatory hiring practice, is enough. But this does not go far enough in terms of redressing the racial inequities that already exist. Dr. Cénat hopes we can move beyond ‘non-racist’ and ‘colourblind’ to becoming a truly anti-racist society in Canada.
“As Ibram Kendi said, there is no ‘racist’ and ‘non-racist’. There is ‘racist’ and ‘anti-racist’. Because if you are just ‘non-racist’, you can see someone be racist, and you can satisfy yourself by telling yourself you’re not a part of it. You haven’t taken an action that can push back against racism. And only by taking action against racism can we create an anti-racist society.”
It is with this ethos in mind that Dr. Cénat and his team have created the course ‘How To Provide Antiracist Mental Health Care’, approved for Continuing Education credits by the CPA. If mental health practitioners, academics in higher learning institutions, and leaders across the country can embrace the principals of anti-racism, then we can truly start to move toward an inclusive Canada where everyone feels welcome, discrimination and profiling are not tolerated, and all of us share in the same opportunities on a level playing field.
Dr. Cénat published an article in The Lancet where he explained that anti-racist mental health care is proactive – in the sense that it addresses racial issues without waiting for clients or patients to bring these issues forward. Anti-racist care goes beyond cross-cultural care. It incorporates both cultural aspects and elements that provide a way to account for the damage caused by racial discrimination, racial profiling, and racial microaggressions. It is a way to create spaces in a society free of racism.
“The problem with the ‘colourblind’ approach is this. You might have someone in your office who is Black, but you say ‘I don’t see his skin colour, I assess him and provide care without seeing his skin colour.’ But the fact is that his skin colour might be a part of his problem. You might have a Black man who’s depressed, and one of the factors which explains that depression is the racial discrimination he experiences at work. Or because his children are experiencing discrimination and he does not have enough power to stand up for his children and that reminds him of the fact that as a kid he experienced the same discrimination from other children and teachers. When you say you don’t see his skin colour, you are not addressing his problem, because the colour of his skin is very much part of his problem.”
This is not just a hypothetical situation that might confront a mental health professional, it is backed up by data. Dr. Cénat’s team published an article that shows Black Canadians between the ages of 15-40 who experience high levels of racial discrimination are thirty-six times more likely to present with severe symptoms of depression than those who experience lower levels of discrimination.
“If you receive someone from the Black communities with depressive symptoms, you have to ask them about their experience with racial discrimination and trauma. So that is what our training ‘how to provide anti-racist mental health care’ provides to clinicians. To know how they can first learn about themselves and their own biases, then also how they can assess racial issues and trauma in a clinical practice. And how they can provide anti-racist care to children, adolescents, and families.”
From October 26-28 this year, Dr. Cénat and his team will be organizing the first conference dedicated solely to Black mental health. It will be called “Black Mental Health in Canada: Overcoming Obstacles, Bridging the Gap”. As Dr. Cénat says, no profession has greater tools to address racism than does psychology. And he’s committed to putting as many tools in that toolbox as he can.
Psychology Month Profile: Dr. Andrew Hyounsoo Kim and Dr. Nassim Tabri, Addiction Psychology Section

Dr. Andrew Hyounsoo Kim

Dr. Nassim Tabri
Dr. Andrew Hyounsoo Kim and Dr. Nassim Tabri , Addiction Psychology Section
Addiction Psychology covers a lot of ground, from substance use to video games. Today’s Psychology Month feature talks to Dr. Andrew Hyounsoo Kim and Dr. Nassim Tabri about the work they’re doing in the field of addictions, and about combatting the stigma that remains around the subject.
“I’ve never had a client when I ask them what brought them in here today say ‘I wanted to become addicted, so here I am’. That has never happened.”
Dr. Andrew Hyounsoo Kim is an assistant professor in the department of psychology at Ryerson University and the Chair of the Addiction Psychology Section at the CPA. A clinical psychologist (Interim autonomous practice), Dr. Kim completed a residency at Royal Ottawa Substance Use and Concurrent Disorders unit. He points out that no one starts out using substances or engaging in a behaviour with the goal of doing it to the degree that it’s going to interfere with their functioning.
Almost everyone has tried alcohol and other drugs. There are few Canadians who have not placed a bet or played an online video game. Some folks end up doing these things in an excessive sort of way, or engage in them more often and for longer periods of time than do others. But very few people develop an addiction. We all make the choice to try some of these things and might make the choice to continue doing them to some degree – but no one chooses to become addicted.
Addiction is one of the most highly stigmatized mental health conditions. In an effort to move away from that, and to create a greater understanding among the public, there has been a real shift over the past decade to move away from stigmatizing language. Researchers and clinicians in this field no longer use the words ‘dependence’ or ‘abuse’ but rather refer to ‘substance use’. Dr. Kim says,
“We no longer use the word ‘addict’. Instead we say, ‘a person experiencing an addiction’. We don’t use the word ‘junkie’, and even ‘clean’ is no longer in our vocabulary because those words are laden with negative meaning.”
The word ‘addiction’, in and of itself, is widely used – and widely misused – in society in general. We tend to use it to describe anything that people will engage with for a long period of time.
“Think of all the ads you’ve seen that say something like ‘this TV show is really addictive’ or ‘I’m addicted to this game’. People use the term a lot, without really knowing what it means. Addiction has a very specific meaning that is far more nuanced than just an activity someone engages in for long periods of time. It encompasses not just the biological (the brain) but also behaviour, emotions, thoughts, and the consequences that come about as a result of it.”
In addition to misuse of the word, there remain a lot of misconceptions about addiction itself – that it is a moral failure, or a personal choice, and that becoming addicted is an indication of a lack of character. Dr. Kim continues,
“At the very beginning when you’re starting to engage in an addictive behaviour there is of course a personal choice. But over time, it becomes a lot more complex than just lack of free will. There are changes that occur in the brain and to a person’s emotional and psychosocial context and it really moves away from being something a choice to a compulsion – that they engage in it even if it is no longer pleasurable. If all it took to stop was for us to say ‘stop using’, clinical psychologists who specialize in addictions wouldn’t have a clinical practice. Addictions are much more complex than just stopping.”
Dr. Nassim Tabri is an assistant professor of psychology at Carleton University. His research is focused on addiction and mental health, particularly the transdiagnostic factors that are present across a range of problematic behaviours such as gambling and disordered eating.. He says,
“In thinking about what constitutes an addiction, and how one can potentially develop an addiction, think of it this way. You try alcohol for the first time, or you pick up a video game and start playing. It doesn’t necessarily mean that a person who tries these things that have high addiction qualities will end up developing an addiction. Addiction happens when they persist in these behaviours, even though the fun has been taken out of it. Now it’s about doing it because you need to do it to function more so than because you’re enjoying it, and because not doing it makes you miserable.”
Addiction psychology is a vast science, touching on virtually every aspect of our connected lives. Ads, games, phones, and more are designed using principles derived from that science. But there is a definite threshold to behaviours that constitute addiction – it’s not an exactly defined threshold, in that it might be a little different for each individual experiencing addiction, but it is a pretty high bar in terms of the activity, or substance use, or behaviour affecting that person’s life. Dr. Tabri says,
“’Addiction’ is a term that should be reserved for an extreme condition. When you see ads, or gamble, in a way they’re nudging you to engage in a certain behaviour. Whether someone develops an addiction or not really depends on their risk profile (biopsychosocial risk factors). Milder engagement in these activities, even though you’re being influenced, doesn’t merit the term ‘addiction’.”
I haven’t touched my phone in about two hours. I pick it up and scroll through the notifications – CBS Sports wants me to know that the Denver Broncos have hired Green Bay’s offensive co-ordinator Nathaniel Hackett as their new coach. The Flipp app would like me to see the new deals available this week at Loblaws. My little mobile game wants me to know my lives have been refilled, Shoppers Drug Mart is very worried that I might miss out on my chance to get 10,000 Optimum points by spending $40 in their store, and Twitter has sent me eight notifications about eight new followers I’ve picked up today.
While not necessarily the work of psychologists who specialize in addiction, all these notifications are informed by addiction psychology. All are designed to provoke a response from me, to get me to interact with the app, the store, or the content in a way that maximizes my time on my phone and (by extension) minimizes my time doing other, presumably more productive but less immediately engaging, things. While these things are created and informed by addiction psychology, the fact that they influence me does not mean that I am “addicted” – there is a certain threshold for the use of that term, and until I forego sleep, skip meals, and leave work four hours early to play Words With Friends, I have likely not crossed that threshold.
Dr. Kim says,
“There are principles being used that increase the likelihood of addictive type behaviours on your smart phone. Things that increase the time on the device. Making it more engaging, sending notifications. With video games in particular, things like leader boards, or ‘here’s a special offer today – for only $1.99 you can get extra lives’. Gambling is another example - psychological knowledge and principles have been used to develop slot machines, to make it more likely that people will stay on the device for longer periods of time.”
While the psychological principles of addiction can, and have, been used to create addictive behaviours that sometimes result in an addiction, psychologists who specialize in this field tend to work on the other side of things. They’re focused on prevention and treatment. They’ve created the low-risk drinking guidelines, low-risk gambling and cannabis guidelines, the theories behind Smart Serve certification, and harm-reduction initiatives like safe injection sites. It’s here where psychological knowledge is applied directly to reduce the harms that some of these substances or behaviours may have. Says Dr. Kim,
“Psychology is the scientific study of the human mind and behaviour. So Addiction Psychology in that sense is using psychological scientifically sound methods to better understand why some people may use substances to the point of addiction, why some people may become ‘addicted’, if we use that word. It’s also trying to better understand the effects of substances and other addictive behaviours on the brain, and for me – what I find most interesting – is how we develop interventions, treatments, and preventions so we can reduce the harms and suffering for people who are living or have lived with addictions.”
When we hear the word ‘addiction’, we tend to think of addiction more in relation to substances than to behaviours. Cigarettes, alcohol, the opioid crisis are all top of mind when it comes to addiction – but are those type of addictive behaviours the same as, say, gambling or video gaming? Dr. Tabri says…not necessarily.
“One thing we focus on is the brain. I have a whole lecture talking about the dopamine reward system. I think there is an understanding in the general public that addictive behaviours have similar influences on the brain in terms of hijacking the dopamine reward system. The idea is that you’re no longer engaging in other activities that are meaningful and make you feel good, instead you’re doing this one thing that makes you feel really good at the expense of all the other things in your life.
But are all addictions one and the same in the brain? Not necessarily. The lay theory was once that it’s all dopamine, and that underpins everything. That started with research with rats in the 50s, and the story took hold because it was an attractive one. It grew into the idea that dopamine can explain all kinds of addictive behaviours. But when you look at the literature, what it says is that dopamine is really good at explaining something like alcohol, for example, or nicotine to some extent. But other addictive behaviours like cannabis, not so much. There’s more nuance and complexity going on than just dopamine. It may play a role, but it’s not the end-all and be-all in the brain.”
The science of addiction, and the psychology behind it, is ever evolving as we learn new things and approach them in a different way. Just as we have evolved in the terminology we use around mental health, substance use, and people experiencing addiction, we have instituted many programs, campaigns and initiatives to reduce harms and reduce stigma. Through it all, many things remain true – the most important being:
No one chooses addiction.

Juanita Mureika

Dawn Hanson
Juanita Mureika and Dawn Hanson , Psychologists and Retirement Section
Even after retiring, many psychologists have ongoing professional responsibilities. Today’s Psychology Month feature talks to Juanita Mureika and Dawn Hanson about the work they’re doing in this space.
Many psychologists get into the profession with a goal of advocacy – advocacy for their clients, for the advancement of psychological science, for knowledge mobilization and for ending the stigmas surrounding mental health. Whether this advocacy is explicit or implicit, it is a universal impetus for people who dedicate their lives to helping others.
That motivation to be of service to others does not end when a career ends. Retirement from the profession of psychology does not necessarily mean retirement from advancing good causes. In fact, it might provide more time to tackle those challenges, or even illuminate new causes to champion.
Such is the case for Juanita Mureika and Dawn Hanson, Co-Chairs of the Psychologists and Retirement Section of the CPA. Juanita retired as a school psychologist in 2011, but remains active in the New Brunswick political arena. She spent much of 2021 pushing against Bill-35, which included a decision by the New Brunswick government to take student assessments out of the hands of school psychologists and allow teachers to perform those assessments instead.
Dawn recently retired as the Chair of the Manitoba Association of School Psychologists, but stays active and involved with the recently proposed Bill-64. The bill would do away with all school boards, to have more of a central authority in government in Winnipeg. She says,
“We, as an organization [the Manitoba Association of School Psychologists], are always tracking anything that could impact psychological services in Manitoba, particularly as it pertains to school children and families. I can’t imagine – retired or not – not being involved in these burning questions and issues. We’ve been very involved in trying to shape a new College of Psychologists in Manitoba. Our school psychologists have not been part of the regulatory body before now. So now with the opportunity of a new college coming in, we’ve been working for many years trying to create representation within that college.”
For Juanita, Dawn, and the Psychologists and Retirement Section as a whole, advocacy does not end with retirement. And retirement itself actually creates further areas where advocacy can be very important. Retired psychologists across Canada are very concerned about regulations in their respective provinces for how long files are to be kept. In one province the rule is that files must be kept secure for fifteen years – but if your client is a school-aged child, then those files must be kept secure for fifteen years after the year when that child reaches the age of majority. Dawn says,
“This is very onerous for psychologists who have to somehow find a way to store and maintain these files securely, sometimes for decades! For Juanita and I, most of our practice has been within a school setting, so when we retire from our job, it’s not our problem any more. The school must keep those files safe and secure in line with what is required either by the regulatory body or the province.”
Neither Dawn nor Juanita are affected by this issue, but here they are championing the cause nonetheless. The Psychologists and Retirement Section has sent out a survey to all other regulatory bodies across Canada, including the Territories, to determine what the issues were regarding confidentiality, file retention, informed consent, and more. As of the writing of this article, the responses from those groups are still coming in – slowly. So far, the one thing that is clear is that the regulations, policies, and practices governing file retention vary wildly from one province to another.
Imagine you’re closing your psychology practice and retiring. In addition to a massive number of electronic files, you also have reams of physical paper files that you must keep secure for a further fifteen years. It is likely impractical, not very secure, and possibly illegal for you to keep them in your basement. Are you going to pay for 15 years at a storage locker, on what is now a fixed retirement income? What are your options and how can you go about doing this? And who, depending on where those files are stored, will insure them?
Dawn and Juanita are on the case. It may take a while to procure answers, as every step along the way there is another wrinkle thrown in. Says Juanita,
“Another thing we now have to consider is that many provinces require a professional will if you’re going to retire. So those files will become someone else’s problem if you retire, or if you die. But not all provinces require that. There’s always something new. But if you think about medical or dental records, those are kept for a very long time and so should psychological records be kept a long time. It’s just a little overwhelming for people who think ‘how long will this go on?’”
Juanita, Dawn, and the Psychologists and Retirement Section may be retired as psychologists, but are increasingly involved in advocacy. Within school boards, provincial policies, and the section itself there are multiple opportunities to shape systems for the better. They are going to keep pushing forward on the issues that are important – for retirees, for school psychologists, and for everyone else.
 Dr. Eleanor Gittens
Dr. Eleanor GittensDr. Eleanor Gittens is a professor at Georgian College in the Police Studies degree program. She helps students confront their biases before they graduate and go on to become police officers – by taking them to Barbados!
The national dish of Barbados is fried flying fish (try saying that six times fast) and cou-cou (a cornmeal-okra concoction) with a spiced gravy. Barbadian cuisine is also known as “Bajan” cuisine, and the fish cakes and fried delights have influenced food all over the globe. As with food, Barbados itself has had an outsized cultural impact compared to its tiny size. Barbados has a population of fewer than 300,000 people.
The town of Barrie, Ontario is, on its own, half the size of Barbados. It counts a little over 150,000 inhabitants, one of whom is Dr. Eleanor Gittens. Dr. Gittens was born in Barbados, and is now a professor at Georgian College in the Police Studies degree program. The key courses she teaches at the moment are in research methods, cyber crime, mental health issues in policing, and contemporary social movements. She says,
“My passion is research. I love to do research with policing agencies – especially if they have a question or concern but are unsure how to go about getting the evidence or the data from what they have already. I can help them answer those questions.”
One of those questions was regarding calls from local long-term care facilities in Orillia. The OPP service in the area approached Dr. Gittens because they were concerned that they were getting too many calls for service from those facilities that didn’t require police presence. Because research opportunities are also teaching opportunities, Dr. Gittens and a few of her students created a research team to examine the issue. They looked at all the calls over a period of time to determine what the evidence showed.
They found that the OPP were correct – that 60-70% of the calls they were getting from long-term care facilities did not require police presence. In many of the cases it was residents calling 9-1-1 directly from their rooms for something trivial like having misplaced their remote. Dr. Gittens and her students presented their findings to both the police service and to the long-term care facilities (and at the CPA Convention that year).
Their recommendations led to changes at both the police service and the care homes themselves. The long-term care organizations made changes to how their residents accessed telephones, and the processes by which staff contacted emergency services. The police changed policies beyond just when to respond, but also altered the way they responded to calls at these facilities to ensure the response was appropriate for the situation.
Most of the students who go through Dr. Gittens classes go on to become police officers. In recent years, a much greater focus has been placed on implicit bias in policing, and the ramifications that result from that implicit bias – most particularly, for communities of colour. Says Dr. Gittens,
“Often, police officers have a view of who the criminals are, and where the criminal activity takes place, based on their own personal biases and the feelings you’ve developed over time from working in the field. One of the things we’re trying to do when it comes to human rights and social justice is to break down some of those biases so that people can start to see things for what they are rather than seeing them through the lens of their bias.”
So how, then, to deconstruct some of that bias before these students graduate and go on to become police officers throughout Canada, serving vastly different communities with very different needs and systemic issues? Dr. Gittens says that although it is impossible to get rid of bias entirely, she figured the best way to move future officers in that direction would be to take her students – who are predominantly white – to a place where they would be the minority, removed from their current social environment. The students are in Orillia, a city with very little diversity. Dr. Gittens is the only Black professor at Georgian College. So where to take those students?
Barbados. She takes them to Barbados.
“Barbados is 95% Black. They get to explore the food, and the culture, and also to tour police stations and the prison. [Yes, there is only one prison in Barbados.] We’ve done a Supreme Court tour, where they got to sit in on a case. They got a chance to see some of the intricacies of how culture plays into peoples’ behaviour, how people think, and also how they are percieved. It’s only one opportunity for them, but I think it’s better than no opportunity at all.”
It’s hard to understand the impact of culture and heritage until you’re smack in the middle of one that is not your own. The students, of course, love these trips.
“Not only does every student love it, it’s one of the things police services are looking for now. When I have to do a reference for students going into policing, one of the questions they ask is ‘what do you know about their views on diversity?’ For the students I take on trips, I can speak to how they behaved during their visit. What set them apart from some of the other students? How did they embrace, for example, the food? There are people who refuse to try new food, simply because they don’t know it or understand it! Fear is an emotion that can really debilitate people.”
Dr. Gittens loves helping her students reach a higher level of cultural competency in her professional life, and loves to travel in her personal life. Unfortunately, the student trips, and her travel, have had to be put on hold to a large degree during the pandemic. One day, these things will be possible again. When they are, Dr. Gittens looks forward to bringing more students to Barbados to experience the culture, the atmosphere, and – of course – the cuisine. One word of advice to anyone who goes.
“Try the fish.”

Dr. Jonathan Wilbiks
Dr. Jonathan Wilbiks , Brain and Cognitive Science Section
Researchers in the realm of the Brain and Cognitive Science are interested in how our brains work, and how they perceive and sort external stimuli. Today’s Psychology Month feature delves into this subject with Dr. Jonathan Wilbiks about his work – and that of Snoop Dogg and Angela Hewitt.
“With so much drama in the LBC
It's kinda hard bein' Snoop D-O-double-G.”
You’re in the audience for the Super Bowl halftime show. Dr. Dre, Eminem, Mary J. Blige, Snoop Dogg and Kendrick Lamar are performing, and you’re grooving to the music. On the big screen you can see Snoop rapping and the music hits your ears. The crowd around you is roaring and cheering. You are lost in the moment so you’re not really thinking – how do I know? How do I know that it’s Snoop Dogg’s voice that I’m hearing? How am I certain that the crowd noise around me is being made by my fellow fans? You don’t have to answer that because your brain is putting it together for you. Snoop’s lips are moving on the big screen, and they seem to match the lyrics you’re hearing. The crowd noise is coming from behind, in front, and all around you and your brain sorts that out for you so you know it’s thousands of people shouting thousands of different ways, and you need not pay attention to any one voice in the crowd.
How your brain performs these tasks is the realm of cognitive science, studied by researchers like Dr. Jonathan Wilbiks, an associate professor in psychology at the University of New Brunswick Saint John. Dr. Wilbiks is the Chair of the Brain and Cognitive Science Section at the CPA, and studies audio-visual integration and multisensory processing – how our brain takes various sensory inputs and makes an implicit decision as to whether those things came from the same source. (Your lips are moving, and I hear singing – it is likely your voice I hear.)
Recently, some of Dr. Wilbiks’ work has been around perception and musical abilities. His lab found that musicians perform much better than non-musicians at tasks when audio and visual are congruent – that is to say the image matches, and happens at the same time, as the sound. But musicians perform worse than non-musicians when audio and visual are not congruent. People who have been trained in music, more than those who have not, use auditory information to help them make sense of something they see.
When Angela Hewitt sits down at a piano and places the sheet music for the Goldberg Variations in front of her, it all makes perfect sense. Each note on the paper indicates a note she must play on the piano, and the two things are congruent – this is something she has done her entire life and it’s easier for her than it is for…well, everyone else in the world. But if, instead of sheet music, she was presented with a cuneiform tablet that represented a musical notation, she might be completely lost – in fact, someone with no ability to read music at all might be able to perform the task better than she could. (The first musical notations ever discovered were from about 1400 BC on a cuneiform tablet in what is now Iraq.)
In the years following the Second World War, the big trend in psychology was behaviourism. You put a rat in a box and expose it to a stimulus, then you measure how it reacts and how those reactions change over time with repeated exposure to that same stimulus. We didn’t really pay a lot of attention to what was actually happening in the brain. Dr. Wilbiks says this was because science is all about observable fact, and there was no way to observe what was happening in the brain at the time. Where this began to change was in the late 60s, when German-American psychologist Ulric Neisser published Cognitive Psychology, which suggested that a person’s mental processes could, in fact, be measured and analyzed. Dr. Wilbiks says,
“The cognitive researchers who showed up in the 60s said ‘there’s a whole lot happening in the brain’. Sure, we don’t know exactly what’s happening there – but something is, so to ignore it completely is a mistake. So they would try to hypothesize about what might be happening, and to try to measure using secondary observations. A simple example would be something like a reaction time task. I give you a button and tell you to push it every time a light flashes on the screen in front of you. People are generally pretty fast at that – maybe 200 milliseconds. But if I give you two buttons and tell you to press the left one when a green light flashes and the right one when a red light flashes, it will take longer. Maybe 400 milliseconds. You can’t see what’s happening in the brain, but you can surmise that if task one takes 200 milliseconds, and task two takes 400 milliseconds, that tells us very basically that processing information in the brain takes time.”
Over time, of course, things moved way past red-light-green-light as experiments became more sophisticated and technology allowed us to actually see what is happening inside our heads. We can see the electrical voltage created by neural impulses in the brain. fMRI (Functional Magnetic Resonance Imaging) machines allows scientists to observe and measure changes in the oxygenation of blood which indicates differing levels of brain activity. We can now tell which areas of the brain are active, when they’re active, and then correlate that with the behavioural information we see.
The field of the brain and cognitive sciences is vast, and has effects that can be seen in our everyday lives in a myriad of ways. Right now, there is a ton of stuff going on where you are. You might be sitting down on a chair. There is other furniture in the room, maybe decorations on the wall. There is traffic going by outside, maybe the dishwasher is going in the background and someone is watching TV in another room, all while you’re reading this article. You can’t possibly pay attention to all of it at once, so your brain filters all of those external stimuli before you even perceive them, so you aren’t overloaded.
Your brain decides, for you, what is consequential. That traffic you hear outside? It can be ignored because it doesn’t present a threat. As Dr. Wilbiks says, cars rarely crash into houses so, while sitting in your house you are free to be unconcerned about the sound of cars. But when you’re walking down the street, the sound of cars is very important to you – if you hear the sound of a car accelerating as you enter a crosswalk, you should certainly turn your head toward that sound to see what’s happening, because now there is a real possibility of danger.
The brain creates these shortcuts to get maximum efficiency with minimum effort, something called “cognitive economy”. Because we use these shortcuts, and we process only the most pertinent information and take the most important cues, we are susceptible to “nudges”. These are little things cognitive science has created to make us behave a certain way. One example is being a safer driver. Dr Wilbiks gives an example:
“You’re on the road in your car, and you know you’re driving on a small residential street. You know the speed limit is 40 km/h, so you’re driving rather slow, and you’re paying attention. Looking for kids running out into the street, a dog running loose, a basketball rolling toward the road. If you’re driving on the highway, you’re paying attention to many other things, but you’re not looking for an errant basketball. Where we can use cognitive understanding and nudges is in a situation where, for example, people tend to be driving too fast on a residential street. We can do things to slow them down. You’ll sometimes see little islands, with a tree on them or something, that make the road a tiny bit narrower. It doesn’t get in the way of traffic, but the average person wouldn’t feel comfortable driving through that narrow gap at a speed greater than 40 km/h.”
The one thing that my brain focuses on, whether I’m in my car or working on my computer, is music. Anywhere it’s playing, in the background or from my neighbour’s garage way down the street, I can’t ignore it. Dr. Wilbiks says one of his favourite classes to teach is The Psychology Of Music, because it encompasses so many aspects of psychology in general, not just of cognitive science. He says,
“I usually scare students in the first few lectures because we start out with physics. The physics of sound, and sound waves, and how that works. Then it’s about how the vibrations get into your ear, how that translates up into your brain and how you perceive it. Then we get into developmental psychology – how do we develop our musical ability, the close parallels between musical development and linguistic development. We talk about treatment – there’s some really cool work being done using music (Melodic Intonation Therapy) to help people who have experienced a stroke recover some linguistic ability.”
We all have two hemispheres in our brain, and there is a part in the right hemisphere where we process music. There is a part in the left hemisphere that mirrors the music part almost exactly, and that’s where we process language. When people who have had a stroke sing the words they are trying to speak they can, over time, train the other hemisphere of their brains to process language again. Eventually they might regain up to 70-80% of their speaking ability as a result. People living with dementia are often able to connect with music in a way they can’t with language, as music can trigger memories that might otherwise be inaccessible.
Perhaps you’ve seen the meme going around that says, ‘my ability to remember song lyrics from the 80s far exceeds my ability to remember why I walked into the kitchen’. This might actually be true, as music from our youth remains a powerful trigger for memories which is why dementia support groups often sing songs together from their youth – Beatles and Beach Boys and traditional folk songs from the country where they were raised. In a few years, things might be a little different – in 2054, those support groups might be singing ‘Gin and Juice’ by Snoop Dogg. Will rap songs produce the same kind of memories and enhance language abilities in the same way? Only time will tell – but when we do have the answer to that question, it will be provided by cognitive psychologists and others in the field.

Dr. Gilla Shapiro
Dr. Gilla Shapiro, Health Psychology and Behavioural Medicine Section
Health Psychology and Behavioural Medicine covers a lot of ground, from encouraging people with diabetes to take their insulin to nudging people toward healthier eating habits. Today’s Psychology Month feature talks to Dr. Gilla Shapiro about the work she’s doing in the areas of cancer and vaccines.
Health Psychology and Behavioural Medicine
“We know that vaccine uptake varies depending on the vaccine. Even before COVID-19, certain vaccines like MMR [Measles Mumps Rubella] had higher uptake rates than the flu vaccine. There is also a difference between childhood and adolescent vaccines. You could see that with HPV [human papillomavirus] which was administered in schools to adolescents.”
Health Psychologists and Behavioural Scientists have expertise that spans a very wide variety of specialties and disciplines. Many are also clinical psychologists, licensed to provide psychological services and therapies. Clinical Health Psychologists help people through medical issues, diseases, and chronic conditions. Behavioural Scientists study all of this, especially when it comes to preventative behaviours and behaviours that can affect the progression of a medical diagnosis. What helps a person with a heart condition maintain a strict diet? What affects the consistency with which a diabetic takes their insulin? And – very importantly of late, what factors influence a person’s acceptance and willingness to be vaccinated?
Imagine you have just been diagnosed with cancer. You probably have hundreds of questions and even more fears suddenly thrust upon you. There may be other factors that compound that stress, like the possibility of infertility, the loss of income, or the need to arrange childcare while receiving treatment. You might also now have a whole bunch of new doctors and specialists you never had before – oncologists, oncology nurses, patient navigators, genetic consultants. It’s a lot to handle, on top of trying to come to grips with the diagnosis itself.
One of the people who might help you through this difficult time is a psychologist, like Dr. Gilla Shapiro at Princess Margaret Cancer Centre in Toronto. Dr. Shapiro is a clinical and health psychologist, a behavioural scientist, and a psycho-oncologist (a specialist in cancer). She works with people who have received a diagnosis, with those who are undergoing treatment, and also with people receiving end-of-life care.
“There are many people who experience elevated distress [related to cancer and its treatment] so having a specialized treatment team to support them and their loved ones is really important.”
Some of this takes the form of supportive therapies, and some of it has to do with decision-making. If a person experiencing cancer must make a decision as to whether to begin a chemotherapy regimen, given the devastating toll that takes on the body and a certain percentage chance of it working, talking that through can be very helpful in the process. Trying to decide whether to join a clinical trial can be an overwhelming choice a person with cancer has to make. A psychologist like Dr. Shapiro approaches this in a few ways ̶
“People need support in different ways and have different concerns that could be social, practical, psychological, or emotional. Some may wonder, how am I going to approach cancer with my children? Others may require support with symptoms like pain, insomnia, anxiety, or depression. There are some types of cancer for which there is a genetic predisposition. So if genetically tested, some people wonder who should I tell, and how do I tell them?”
A team at Princess Margaret is working on developing evidence-based interventions to reduce distress and improve patients’ cancer experience. For example, an intervention called CALM (Managing Cancer And Living Meaningfully) is designed to help patients adjust to living with advanced cancer. It draws from a number of theories in psychology and mental health – relational, attachment, and existential theories – the goal being to address a number of different domains in an individualized way. Symptom management, changes in a patient’s relationship with themselves as well as their loved ones, a sense of meaning and purpose in life, and hopes and concerns relating to the future are all factors that are considered in CALM therapy and are all experienced differently by every person who receives a terminal cancer diagnosis.
One of the reasons Dr. Shapiro chose to come to Princess Margaret was that her supervisor, Dr. Gary Rodin, along with his colleague Dr. Sarah Hales, had developed CALM. Dr. Rodin and his colleague Dr. Madeline Li were also doing interesting work in understanding what factors impact individuals in make difficult health decisions. One big decision in cancer care, one that has come about much more recently, is medical assistance in dying, or MAID. Dr. Shapiro wanted to bring a health equity and policy lens to this work. Dr. Shapiro didn’t start her work in psycho-oncology and behavioural science there though, she began her work in psycho-oncology in cancer prevention and working on vaccines. Vaccines like the HPV vaccine, and how we can prevent viruses that cause cervical and other cancers by supporting individuals in making behavioural choices, like getting vaccinated.
Less than two years before COVID-19 was declared a pandemic by the World Health Organization (WHO), Dr. Shapiro completed her PhD on human papillomavirus (HPV) vaccine hesitancy in Canadian parents. With colleagues at McGill University, she developed scales to measure vaccine attitudes and conducted research to understand the behavioural and social drivers of vaccination in the Canadian population.
. In 2019, she began working with the WHO developing tools for routine childhood vaccination and to measure the behavioural and social drivers of vaccination globally. When the pandemic hit, that work pivoted to understanding adult vaccine acceptance and intention to the COVID vaccines, as they became available
During the COVID-19 pandemic Dr. Shapiro has been a member of Ontario’s COVID-19 Science Advisory Table’s Behavioural Science Working Group and she and her colleagues at the COVID-19 Science Advisory Table for Ontario (many of whom are also members of the Health Psychology and Behavioural Medicine Section of the CPA) published the brief ‘Behavioural Science-Informed Strategies for Increasing COVID-19 Vaccine Uptake in Children and Youth [link]’ in October.
While understanding the behavioural and social drivers that impact COVID-19 vaccine acceptance, she has also developed an interest in another cascading impact of the pandemic: missed or delayed routine vaccinations. Dr. Shapiro and colleagues at the WHO and elsewhere have recently completed a study looking at missed routine childhood vaccinations in 26 countries during the pandemic [link - COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: An observational survey].
Imagine you have been through a cancer diagnosis, have been through surgery and radiation, and are now on the other side with a (relatively) clean bill of health as a result. A clinical health psychologist may have helped you through that process, but now there is another, out-of-your control existential threat – a global pandemic. Your continued safety, in your immunocompromised state, relies on those around you getting vaccinated against that pandemic. It’s not an easy place to be, but it is nice to know that Health Psychologists and Behavioural Scientists like Dr. Shapiro are out there, working on that as well.

Ann Marie Beals

Dr. Natalie Kivell

Ramy Barhouhe
Ann Marie Beals, Dr. Natalie Kivell, and Ramy Barhouhe, Community Psychology Section
Community Psychology is a little more “community” than “psychology” and is heavily involved with social justice issues. Today’s Psychology Month feature talks to Ann Marie Beals, Dr. Natalie Kivell, and Ramy Barhouhe about the work they’re doing in this space.
“People who are engaged in social change in their communities – community organizers, grassroots social movement folks – have equally rigorous theories about how change works as we might have in academia.”
Dr. Natalie Kivell is an assistant professor at the Wilfrid Laurier community psychology program. She says there are “two…and a half?” community psychology programs at Canadian universities, and that those who work in the field tend to be a lot more involved with the ‘community’ part than the ‘psychology’ part of that job description.
Ann Marie Beals is one of those people. Ann Marie is a graduate student in the community psychology program at Wilfrid Laurier. They are L’nuk of Mi’kma’ki - African Nova Scotian and Mi’kmaq descent, and their work focuses on the erasure of mixed-blood Indigenous-Black communities historically and in the context of today’s society, Truth and Reconciliation, and the ongoing marginalization of both Indigenous Nations and Black communities in Canada.
Natalie’s student Ramy Barhouhe is originally from Lebanon and lived in the United States before coming to Wilfrid Laurier for the community psychology PhD program. His work is focused on colonialism and coloniality – how these power structures have shaped the development of whole community systems in North America and Southwest Asia. How this guides the way people perceive, feel, and experience the world in terms of time, space, morality, power, education, health, justice, politics, economics and more.
Ramy, Ann Marie, and Natalie have come to community psychology via very different paths, but all have similar outlooks in that they all put ‘community’ before ‘psychology’. They are all heavily invested in ways to dismantle our current systems – and they are all keenly aware that they themselves are working within some of those systems. Ramy is studying ways to decolonialize as part of academia, itself a structural vestige of colonial practices. Ann Marie is a member of the CPA, and the Treasurer of the CPA’s Community Psychology section, both institutions that are shaped by the legacy of colonialism. Natalie is a professor in psychology – a field of study that has long been complicit in not only colonialism but also the marginalization of minority populations.
Says Ramy, “the academic world is so intertwined within the neoliberal capitalist system that it’s really difficult to manage the disconnect. The power discrepancy between those who control the flow of knowledge and those that don’t is too big. For example, an academic is getting a grant in order for them to do some research, then they go use a community to get information from that community. But they don’t get approval from that community afterward with regard to knowledge distribution and mobilization. They get the credit, the acknowledgement, and the funding, but the community itself gets nothing from it. They’re just supporting and serving the academic. So that’s one problem with the structure of colonialism within academia that we still need to talk about further and to overcome.
We talk about this a lot in our program, and we acknowledge that we’re part of the problem as well. If we’re doing that research, we’re not absolved from the structure, and the impact it has on the community – we’re still part of that problem. We’re trying to find a way to reimagine this, and it involves a certain amount of respect and humbleness toward the community in which we work. Making sure they get their due, their respect, and even funding to serve their community’s needs. That’s where the shift is – how can we take the resources that are unfortunately part of a corrupt system and use them to benefit those communities? And, how to use their knowledge as their own, and not mine just because I did a survey.”
Ann Marie looks at the current situation, informed by the COVID-19 pandemic, as a window into the work that needs to be done. They say, “one of the things that’s been revealed from this pandemic is how neoliberal austerity policies and practices have affected our health care systems, and how precarious workers in minimum- and low-wage jobs – predominantly Black women, racialized peoples, newcomers, and Indigenous peoples, are disproportionately affected by a lack of compassion, care, and adequate safety nets that were dismantled by neoliberal governments.
As an example, our current Ontario government, within a capitalist system, legislated limited pay increases of 1% for public sector workers like health care workers, as inflation is looming over 4% [4.1% August 2021]. In our community psychology program we have student and faculty researchers who come from and live in communities that are directly affected by neoliberal and colonial practices, such as this one, that continue to widen the gaps in health care and economic stability. At the same time basic human rights such as housing, education, clean water, and quality of life remain not only unfulfilled but purposefully denied. So as a student researcher, I and other critical community psychologists examine the intersections of how power structures such as white supremacy, colonialism, neoliberalism and patriarchy intersect with human beings and with Mother Earth through myriad interconnecting identities.
We look at these power structures, through control of resources on stolen Indigenous lands, anti-Black racism, and colonializing policies. And by that I mean the people who support and hold up these power structures. Sometimes we speak almost abstractly or theoretically about power structures, but we have to be cognizant of the fact that people hold up and maintain these structures. They try to dictate how we live our lives, and systemically oppress anyone who does not fit the able-bodied white cisgendered heterosexual man dominated perception of what is ‘Canadian’. For me, it’s always about dismantling the power structures that oppress people in my communities.”
There are several words Ann Marie, Ramy, and Natalie all use quite often – intersection, dismantling, neoliberal, colonialism. Another word they all use, maybe even more often, is “collaboration”. Ramy speaks about working in collaboration with communities, so that the work done there is not extracting, but rather enhancing, the knowledge, the health, and the success of that community. Ann Marie speaks about collaboration in the sense that credit for the work done is not only not the end goal, but antithetical to the process of self-determination in communities. And Natalie talks about dozens of other community organizations, grassroots activists, and scientific disciplines with whom she works to advance the myriad causes of social justice. In fact, the very first word she uses to describe community psychology is “interdisciplinary”.
“Community psychology is an interdisciplinary, values-driven, action-oriented, community-engaged social science. It addresses social justice at the intersections of racial, climate, immigration, gender, prisoner, and disability justice. We work at the intersections of the complexities of how social justice issues touch each other in an interconnected way. Community psychology is guided by a set of theories. We approach these complex social issues from places of prevention, ecological theory, critical perspectives, and decolonial perspectives. We look to situate relationships between individuals, communities, and societies. If we have equitable and just communities, we have healthier people. And therefore the target of community psychology is figuring out how to rebuild, re-imagine, and co-create equitable school systems, health systems, prison systems and so on.”
Because Community Psychology tackles such a wide array of systems and structures, their work crosses many boundaries into other aspects of psychology – criminal justice, environmental, educational, and more. Although they are small in number, their collaborations across disciplines, sciences, community groups and activist organizations ensures that they will continue to have an outsized impact.

Dr. Milica Miočević

Dr. Rob Cribbie
Dr. Milica Miočević and Dr. Rob Cribbie, Quantitative Methods Section
Quantitative Methods is a science that works with nearly every branch of psychology. All researchers use different methods to analyze data – but all of them analyze data. Today’s Psychology Month feature talks to Dr. Milica Miočević and Dr. Rob Cribbie about the work they’re doing to make that data collection and analysis easier, more consistent, and more accurate.
In the very broad field of psychology, Quantitative Methods is the indie college radio station of the group. The one who played U2 and R.E.M. in the 80s before ‘Sunday Bloody Sunday’ and ‘Man on the Moon’ became ubiquitous. The one who “discovered” the Red Hot Chili Peppers in the early 90s before Blood Sugar Sex Magic and the Grammys. Or who, more recently, broke the Black Eyed Peas before the addition of Fergie and all that commercial success.
Quantitative Methods is the kid with the nose piercing and the plaid shirt who was into Structural Equation Modeling, Bayesian Statistics, or Hierarchical Linear Modeling, before it was cool. The one who spent months in their room, poring over the catalogue, learning every facet of this statistical method, before letting go and sending it out into the world to be used by psychological researchers. Most of these methods were studied in depth by a very small group of Quantitative Methods Psychologists at one time but are now used widely throughout the discipline.
They’re also, in another way, the Rick Rubin of psychology. You know how the Red Hot Chili Peppers made the big time with Blood Sugar Sex Magic? Producer Rick Rubin. Slayer’s magnum opus Reign in Blood, Adele’s 21, the Beastie Boys breakthrough Licensed to Ill? Rick Rubin. And for psychological researchers doing in-depth work – whether that be on depression, or vaccine confidence, or PTSD in military couples – the producer working behind the scenes to ensure scientific rigour is Quantitative Methods. The Quantitative Methods Psychologists help them craft their study to determine the best way to collect that data, to account for unforeseen wrinkles, and the sample size that is required to detect relevant effects.
Dr. Rob Cribbie is the Chair of the Quantitative Methods Section at the CPA, and a Quantitative Methods Psychologist in the Department of Psychology at York University. He says,
“It’s about research methods and the analysis of data. People who work in Quantitative Methods do everything from consulting on sample sizes, research designs, and the analysis of the data to researching new or improved methods for analyzing data. We also go into the psychometrics of the tools we use and how well they work.”
So what does this kind of work look like, on a day-to-day basis? What exactly does a Quantitative Methods Psychologist do? Dr. Milica Miočević is the Secretary/Treasurer of the Quantitative Methods Section, and a Quantitative Psychologist in the Department of Psychology at McGill. She gives an example:
“I recently published a paper with a co-author from biostatistics on power prior distributions. We were trying to find a way to use historical data from a study that’s related to the current study, but conducted using a sample from a slightly different population. We thought of ways we could quantify the differences between the participants in the previous study and participants in the current study, and tested whether using our method with data from a previous study can improve inferences in the current study. The article that we published will allow researchers in psychology to rely on historical data to improve statistical inferences of new research studies without requiring prohibitively large sample sizes.”
The field itself is, in a way, rather new. The Quantitative Methods Section of the CPA is celebrating its tenth anniversary this year, and the discipline, while widely recognized today, was much less familiar ten or twenty years ago. Says Dr. Cribbie,
“I remember when I was interviewing for jobs, around 2000, most of the interviewees were asking ‘what’s your area of psychology?’ And I would answer ‘quantitative methods’, and they would say ‘no, we mean – is it depression, is it clinical, cultural – what do you study?’ And I would say ‘well…quantitative methods’. They didn’t see this as a discipline. There’s been quite a shift. Now it’s totally mainstream to say ‘I’m a quantitative psychologist’. The area of Quantitative Methods is so broad now, and there are so many tools that we use, that you really need people who specialize in the different methods.”
With the growth of the field has come a sea of change in the ways psychologists analyze and interpret data. The advent of software programs like R and others have opened up a world of possibilities that were a lot more difficult, even inaccessible, 20-25 years ago. And it is constantly changing. As a new method becomes popular and widespread throughout the world of psychology, quantitative methods psychologists have already moved on to something else entirely. Dr. Miočević says,
“We go through waves of what’s interesting and what we think needs to be developed more. When I was in grad school, Bayesian methods were becoming the popular topic. Now, it seems like it’s Machine Learning, and we’ll see what the next thing is. I feel like every few years we add something new to the quantitative methods toolbox in psychology. Sometimes the novel approaches are coming from statistics, sometimes they are coming from other fields like economics. There has been a lot of change in my ten years!”
You know that one pop song you really like? The one by Taylor Swift or Dido or Alicia Keys or Imagine Dragons with the guest rapper? That guest rapper is Kendrick Lamar. Quantitative Methods is, in a way, the Kendrick Lamar of psychology, though they will likely never get the solo recognition that he did when he won the Pulitzer Prize. They will collaborate with anyone from any discipline, any time – so much so that after a while you barely notice they’re there. Every facet of psychology, every individual discipline, is informed by the latest tools for data analysis, the most up-to-date research methods and practices, and the scientific rigour provided by Quantitative Methods. Says Dr. Cribbie,
“Quantitative Methods span all the areas of discipline. So, if you were to take every section of the CPA, Quantitative Methods play a role in every one of those sections. It’s great that there is this section that allows people with this interest to discuss new and different methods, and ways in which people apply these tools.”
It is for this reason that Psychology Month 2022 kicks off with Quantitative Methods – it is the one section that informs all other sections. Dr. Cribbie, Dr. Miočević, and their colleagues are the cool kids on the block who were way into that research method long before you’d even heard of it. You can follow the Quantitative Methods section on Twitter - @cpa_qm – on their website https://canadianquantpsych.wordpress.com/ or through their section newsletter https://cpa.ca/sections/quantitativemethods/newsletter/ so you, too, can be one of the cool kids who knows things before anyone else!

Dr. Elena Antoniadis

Dr. Steve Joordens
Dr. Elena Antoniadis, Dr. Elizabeth Bowering, and Dr. Steve Joordens , Teaching of Psychology Section
The Teaching of Psychology is a science that never happens in exactly the same way. Different groups in varied settings approach learning in a multitude of ways. Today’s Psychology Month feature talks to Dr. Elena Antoniadis, Dr. Elizabeth Bowering, and Dr. Steve Joordens about the work they do in this field.
Dr. Steve Joordens, psychology professor at the University of Toronto, has an analogy to explain the Teaching of Psychology:
“I think of teaching as a craft. Like a craft beer – if you want to be a good brewer of craft beer, you need to know the science behind the recipes and the way you put things together. In addition though, there’s also a subjective element. The mix of ingredients that really works for you might, for one reason or another, not work for somebody else. So, there’s a mix of knowing the science – knowing the ingredients that could make for a powerful educational experience – but then the professor themselves have to find what works for them, and their class, and the context in which they’re teaching. That’s where the craft comes in, merging the science with the human to create a great educational experience for our students.”
Whiprsnapr Brewing Company in Bells Corners, Ontario has a craft beer called OK Lah. It’s a southeast-Asian inspired cream ale made with coriander and ginger. It is certainly not to everyone’s taste, and when I sent some to my sister it sat in her garage for two years as ‘that beer no one wants’. That said, it remains one of their best sellers year after year. It’s a tried-and-true formula that works for many people – but not most people. As in the Teaching of Psychology, inspiration can come from anywhere, but perfecting the formula for success is up to the individual.
Dr. Elena Antoniadis is a faculty member at Red Deer Polytechnic in Alberta and also adjunct faculty with U of Calgary. She is the Chair of the Teaching of Psychology Section at the CPA, and does research on ways to integrate basic neuroscience applications into teaching in order to promote and facilitate learning for students in higher education. She says,
“Teaching of Psychology is about research-based approaches to enhance teaching and learning in classrooms. Some of the research comes from laboratories doing studies in cognitive science that will inform our teaching. Other forms of research occur in the classroom itself. We’re collecting data in the classroom, and that data can inform our teaching practices. The goal is to effectively design and deliver curricula in post-secondary education by using these research-based studies in order to further inform our theory and our practice.”
In 2016, Beau’s All Natural Brewing Company in Vankleek Hill, Ontario made every employee of Beau’s a co-owner of the company. In 2011, they partnered with a local community organization called Operation Come Home to hire youth experiencing homelessness to deliver their beer. Not only are they a fixture in the community who buys their beer, they are involving the community in every step of that process, which has led them to enormous local success. This kind of approach informs a lot of the Teaching of Psychology, and that community involvement is called “service learning”.
Dr. Elizabeth Bowering is a professor in department of psychology at Mount St Vincent University and the Past Chair of the Teaching of Psychology Section. She teaches a range of courses like introductory psychology and developmental courses. Some of her research is in the area of service learning. She says,
“In my adolescent development course, I have my students carry out service learning in the community. So they’re working with youth who may be at risk for dropping out of high school. They work with them, doing academic tutoring and mentoring, as a way to encourage them in their own academic pursuits. There are so many ways we’re trying to broaden the teaching/learning process not only for the ones who are already in our classrooms, but to make that accessible for other people.”
The Church Brewing Company in Wolfville, about three blocks from Acadia University, has a terrific gose called Saltwater Joys. A gose made with salt water makes sense – after all they’re right on the ocean and how much more local can you get? But just because something is there, and accessible, and sounds neat does not mean it is necessarily going to work. Dr. Joordens knows this well, as his specialty is in the effective use of technology to enhance learning. He says that in the past decade, universities have been more cautious about jumping on that latest bandwagon.
“Right from the level of procurement, universities are a lot more careful today about thinking in terms of educational practices and making sure they’re evidence-based. There’s got to be research to support this flashy new thing that they’re buying, and we’re not going to have people using it just because it’s cool. One of our big roles is to create that evidence base and support it. You can have the best technology in someone’s hands, but if you don’t support it well, it might not work for them and it might be a failure.”
The Teaching of Psychology involves that research, those supports, and the measuring of the evidence that goes into teaching – but not just of psychology. Although a lot of the work originates in labs, or in psychology classrooms, the hope for all of the research is that it can be applied to other classrooms, in other ways, and by other people to enhance the learning experience for all students. Dr. Antoniadis gives an example:
“A practical application could be enhancing social interaction in the classroom. Social interaction between students, but also between the student and the professor. Or an application could be used to enhance student motivation, or to direct and inform the use of assessments.”
Says Dr. Bowering, “I think regardless of how long you’ve been teaching, you’re always learning something new, and get surprised by the experiences you have inside and outside the classroom. Our section offers support and encouragement for people at all stages – the beginning academic getting their feet wet, the mid-career professor who’s taught a course dozens of times and wants to bring something new to it, or even somebody further along in their career mentoring others. Teaching of Psychology is really quite broad!”
The Lake of the Woods Brewing Company has locations in Kenora, Ontario and in Winnipeg. Much like virtually every other craft brewery, they have recently expanded their repertoire to include craft sodas – for example, their Hockeytown Root Beer. While it seems like a departure from their standard offerings, this expansion to soda has been universally successful for breweries across the country, and has provided them with another product to sell to folks cooped up in their houses amid COVID lockdowns. Just like how, in the Teaching of Psychology, the pandemic has created an opportunity for something that can be universally applied with success across Canada. Particularly, for students who might struggle with the financial burdens of obtaining a higher education. Dr. Antoniadis elaborates:
“In the last year I’ve been doing research on open educational resources. I also found the Diener Education Fund – it was created by two psychologists who happen to be married, who raised funds to pay for course releases for faculty members who are experts in specific subdisciplines. So, they’ll find a person who’s an expert in evolutionary psychology, and ask them to write a chapter on evolutionary psychology. Then an expert in statistics, or in development, and they fund a course release for that person to write that chapter. They designed a website called The Noba Project where faculty members can go in and customize their own textbooks. I can go in and take the chapters that I want, that cover the same material that exists in publisher-based textbooks. So, I’ve built my curriculum to align with learning outcomes. It comes with royalty-free images, power point slides that I design myself, and I’ve integrated this open educational resource into my learning management system. Our study looked at whether this could create a similar experience for a student who would otherwise have purchased a publisher textbook, and the results show that it did. The students had a positive experience, and did meet the learning outcomes in the course. I had an email from a student who said that he had just lost his job, and if he had had to pay for textbooks he wouldn’t have been able to stay in the course.”
Says Dr. Joordens, “I think of us as the ‘how’ people. Society continually brings up issues of things we’re not doing as well as we could: Providing an equitable education experience, providing a high level accessible educational experience, trying to up-skill all our students so they graduate as great critical and creative thinkers and so on. Making sure Indigenous pedagogies are represented in our educational experience. We hear a lot of these desires from society, and the question is – how do you do that? And we’re the psychologists who try to answer that question. It’s a little like they’re describing heaven, and we’re the ones building the stairways to heaven.”
There’s a Stairway To Heaven English Bitter brewed by the Burton Bridge Brewery in Burton-on-Trent in England. At least, until the inevitable Led Zeppelin lawsuit. Steve continues,
“I’ve recently been introduced to the word ‘intrapreneurs’ – those people working within an organization who are always trying to find a different way, an innovative way, to do things within that structure. And I think a lot of us in the Teaching of Psychology area are those kind of intrapreneurs, who are continually saying ‘how can I do this better? Is there something I could do differently that would make my class more engaging?’ that kind of thing.”
In 2015, Brewmaster, Co-Owner (with former Ottawa Senator Chris Phillips) and Intrapreneur Lon Laddell of the Big Rig Brewery in Ottawa changed the formula and ingredients of Iron Arse Ale. Iron Arse is the special-edition beer Lon creates every year for the motorcycle prostate cancer fundraiser Ride For Dad. There was some consternation at the time, as the previous formulation was well loved in Ottawa. But the new formula proved to be even more successful, and the beer even tastier, than it had previously been. I’ve got no further analogies here, just a suggestion that if you’re ever in Ottawa around the months of May-June, you could do worse than an Iron Arse Ale at the Big Rig.
 Dr. Helen Ofosu
Dr. Helen OfosuDr. Helen Ofosu helps businesses move toward equity, diversity and inclusion as an Industrial/Organizational Psychologist. She says that employees of colour who are staying at home during the pandemic are realizing that their workplace may not have been a very welcoming one when they were there in person.
Dr. Helen Ofosu is an Industrial/Organizational psychologist, an Executive Coach and HR Consultant who founded I/O Advisory Services Inc. in Ottawa. She has extensive experience working with organizations and tackling structural racism at many levels.
“Generally speaking, I work with organizations – it could be government departments, private sector companies, or non-profits – often they bring me in to help with more inclusive hiring or to help improve their workplace culture. Over the past couple of years, I’ve done a lot more training in terms of equity, diversity, and inclusion with a splash of anti-racism and anti-oppression mixed in.
This winter what has me most excited is doing some work with a large government department on a mentorship program that’s quite different. We’re doing some training upfront with the mentors to make sure they understand some of the issues the racialized employees they’re trying to mentor have been experiencing. The idea is that with better awareness and understanding, mentors won’t be contributing to some of the issues with which racialized employees have been struggling. Equally important, with a more realistic perspective, the mentors can focus their interventions more effectively. It’s training for the mentors, but also offering some coaching for mentees above and beyond the support the mentors are providing.
Speaking more broadly, it’s all about supporting individuals and even organizations that are grappling with issues related to bullying, harassment, and of course various forms of discrimination.”
Dr. Ofosu has recently written and spoken about the “Great Resignation.” Over the past two years, during the pandemic, she has noticed a lot of racialized employees choosing to find work elsewhere, as they are realizing that while working from home, they are no longer subjected to the everyday indignities they experienced in the physical workplace.
“These things have been happening for years, but now people are removed from that environment, and they have the peace of mind that comes from doing their work without worrying about microaggressions, or getting the side-eye, or being excluded from coffees, lunches and conversations. When all of that is gone, people feel so much more relaxed because they can just focus on doing their work.
I think the real trigger was in the summer of 2022, when a lot of organizations were planning their return to work. It was only when people started to realize ‘oh my goodness – I might have to go back to the office’ that they started thinking ‘wait a second – I don’t think I can go back to the office. I don’t want to go back to the office! I don’t want to go back to the way things were.’
During all that reconsideration, a lot of people figured it was a smart time for them to find a different place to work, where there’s more representation, more inclusion, more diversity, and just a better workplace culture. From what I’ve seen, people are reflecting on a lot of things during the pandemic. So, they’re looking for a way to find employment where they can just be themselves, and focus on work instead of focusing on self-protection from all these emotional assaults.”
To some extent, Dr. Ofosu is shielded from this kind of thing, personally, by being self-employed. It is a good thing that she will be continuing to do her job, as she is one of very few Black psychologists doing this work in this space – work that is more top of mind than ever, and is more important and impactful now than it has ever been.

Dr. Nasreen Khatri

Dr. Colleen Millikin
Dr. Nasreen Khatri and Dr. Colleen Millikin, Adult Development and Aging Section
The psychology of adult development and aging is the study, assessment and management of the physical, psychological, cognitive, emotional and social functioning of people 18 years and up and includes aging in all its forms, milestones, joys and challenges. Today’s Psychology Month feature talks to Dr. Nasreen Khatri and Dr. Colleen Millikin about the work they do in this field.
“This isn’t your fault. Your brain is letting you down.”
There is still, to this day, a lot of stigma associated with memory loss. That’s why Dr. Colleen Millikin uses this phrase when she talks to older adults experiencing mild cognitive impairment or dementia.
“You don’t take it personally when you’re walking along and your knee gives out. But people respond differently when it’s their brain. If your brain lets you down and you can’t think of that word, or you can’t conjure up that name, you tend to blame yourself much more than when it’s your knee letting you down.”
Dr. Millikin is a clinical neuropsychologist with the Winnipeg Regional Health Authority Clinical Health Psychology Program and assistant professor in the Department of Clinical Health Psychology, Rady Faculty of Health Sciences, at the University of Manitoba. She is the Chair of the CPA’s Adult Development and Aging Section. She works mainly in the public system, assessing older adults where there is a possibility of Mild Cognitive Impairment or dementia. Mild Cognitive Impairment (MCI) is a term that is used to describe memory problems that exist between normal aging and dementia. Compared to others of a similar age, people with MCI are at higher risk of developing dementia over time.
“There are so many things that can interfere with memory that aren’t Alzheimer’s Disease or brain problems. Chronic pain and the medications for it, sleep problems, stress, PTSD, all kinds of things. Even thinking that you might have dementia can be a source of anxiety, and being anxious can make it harder to attend to information and remember it.”
The field of Adult Development and Aging Psychology is a wide-ranging one. It's the study, assessment and management of the physical, psychological, cognitive, emotional and social functioning of people 18 years and up and includes aging in all its forms, milestones, joys and challenges. Dr. Nasreen Khatri is an adult lifespan psychologist and neuroscientist at The Rotman Research Institute, a cognitive neuroscience institute fully affiliated with The University of Toronto. She is registered both as an adult clinical psychologist (18-65) and a gerontologist (65 years and up). She is the Treasurer of the Adult Development and Aging Section of the CPA.
“Specifically, I study the impact of depression and anxiety on the brain, beginning around age 30 and continuing all the way into old age. The biggest misconception about aging is that it is a static category or a state. It is not. It begins at conception and is a dynamic, ongoing process. Aging is simply another word for living!”
Dr. Millikin speaks a lot about the breadth of the field, and the variety of work psychologists in this space are doing. In her field of cognitive impairment, she says,
“Age is the biggest risk factor for developing cognitive impairment, but I have seen people in their 90s with very good brain health and people in their 50s who are living with dementia. There is no single cause for cognitive impairment. In most cases, there is an interaction between a person’s genetics and other health issues.”
Those health issues have begun to be understood a lot more in recent years, thanks in large part to psychologists working in this field.
“We now know that exercise actually grows new cells in the part of the brain that impacts mood and memory. The best thing you can do for your brain and to age well is physical exercise. We have also learned that individuals with an untreated history of depression in mid-life have almost double the risk of developing dementia in later life, compared to those who do not share that untreated history. Depression is eminently treatable with a variety of evidence-based treatments. Dementia is currently incurable. Therefore, we do not want anyone to go down the cognitive path from untreated depression to cognitive impairment and dementia. Timely assessment and treatment of depression today may stave off dementia later on. In other words, taking care of your mental health today could save your brain tomorrow!”
Ideally, interventions to promote brain health should begin as early in life as possible. However, there is evidence that making lifestyle changes can reduce risk of progression to dementia even in people who already have mild cognitive impairment. This is what Dr. Millikin and her colleague Dr. Lesley Koven, a clinical geropsychologist, were seeking to address when they set up their Early Cognitive Change Clinic for Older Adults in 2013. They provide assessment to identify people who have mild cognitive impairment as well as an interview to evaluate the mental health needs of the person’s spouse or other close family member or friend.
“We run a psychoeducational program for people with MCI and their family members to help them learn about MCI, strategies to get around some of the memory difficulties, and lifestyle habits that assist brain health. Exercise and diet are important of course, and we’re also learning that sleep is a big one. Sleep is very important for brain health, but older adults tend to have difficulties with sleep at a higher rate. One of the challenges is that a lack of sleep is not good for your memory, but also that a lot of the prescription or over-the-counter medications people take for sleep can interfere with a brain chemical that is important for memory. Fortunately, there are behaviour changes that help with sleep and psychological treatments for insomnia!”
Family members of people with mild cognitive impairment can also experience significant stress. Again, Dr. Millikin stresses the impact early intervention can have.
“We’re increasingly recognizing the needs of caregivers. We’ve known for a long time that family members of people with dementia can experience significant stress. Even when a person has mild cognitive impairment, family members or close friends can still have some stress related to the situation, although they may not identify themselves as “caregivers.” So if you’re going to do some intervention to help the family member with stress management, that really needs to start as early as possible.
There are many other facets of the psychology of aging and adult development, each as important as the last. Dr. Millikin provides a few examples.
“Dr. Kristin Reynolds, an assistant professor in the Departments of Psychology and Psychiatry at the University of Manitoba, started up a telephone-based program to help people with loneliness during the pandemic. The Past Chair of the Adult Development and Aging Section, Dr. Marnin Heisel, does research at Western University looking at ways to reduce risk of suicidality in older men. Dr. Norah Vincent, a colleague in my department, has developed online cognitive behaviour therapy treatment programs for insomnia.”
Dr. Khatri says the pandemic has had a profound impact on older adults, from mental health (e.g., depression and anxiety) to exacerbating longstanding systemic issues in long term care.
“It has shone a light on how we treat our elders and how we should treat our elders. This is a time for reflection to reconsider clinical, governmental and social policies that impact aging Canadians. Canada is an aging nation and as we go forward we will need to apply systemic policies that optimize our brain health (combination of mental and cognitive health) and allow us to grow older with dignity, autonomy and meaning. The future of brain health in Canada is in our hands, and one of the best ways to predict our future is to create it.
Last, the pandemic has taught us that we need to focus on lifestyle factors (diet, exercise, rest, social connection) at every age to keep us physically, emotionally and cognitively healthy and flourishing.”
In other words – there are many ways you might be able to keep your brain from letting you down. That said, it may happen anyway. And if it does, it’s important to know it is not your fault.

Abbey Horner
Abbey Horner is the CPA Campus Representative at the University of Western Ontario. She is also an entrepreneur, a tutor, an avid reader, a mentee, and the owner of very cold hands.

Joanna Collaton
Joanna Collaton is the CPA’s Student Representative at the University of Guelph, the Past President of the Student Section, the editor of the student publication MindPad, and over the past three years has been involved with the CPA in just about every way a student can be.
Gina Ko is a psychologist in Alberta who has been working in anti-racism for a while. She realized many of her colleagues in that space had great stories to share, so she started the podcast Against The Tides Of Racism. You can find her podcast on Spotify, or at the website here:
www.againstracismpodcast.com/

Dr. Melissa Tiessen and Dr. Karen Dyck created the Intentional Therapist network to help female mental health professionals (themselves included!) stay healthy and happy through intentional and playful self-care.

Dr. Mari Swingle wrote the book ‘i-Minds: How and Why Constant Connectivity is Rewiring Our Brains and What to Do About it’. We discuss the revelations from Facebook research that shows Instagram’s negative effect on young girls, in particular – something Dr. Swingle has been writing about for years.

Dr. Adrienne Leslie-Toogood and University of Manitoba psychology student (and Olympic swimming medallist) Chantal Van Landeghem discuss the mental health of elite athletes in the wake of Naomi Osaka’s withdrawal from Wimbledon.

Caryn Tong

Rohit Gupta
Last year Caryn Tong mentored Rohit Gupta through the CPA Student Mentorship Program. While both were looking for experiences that differed from their own, they found many similarities in one another.


Lauren Trafford and Mattia Gregory have never met in person. This Zoom meeting, with some guy from the CPA, while they happen to be in the same province might be the closest they ever come to actually meeting one another. Their shared experiences, and their shared interests, and their passion for their chosen field makes it certain that they will run in the same circles for a long time to come.
 Dr. Justin Presseau
Dr. Justin PresseauPsychology Month has been extended two days, so we can bring you the work of Dr. Justin Presseau, who is co-Chairing a working group of behavioural scientists advising Ontario healthcare executives and government representatives on best practices during the COVID-19 pandemic.
Justin Presseau
Dr. Justin Presseau is going to welcome a new baby in about a month. His wife Leigh is eight months pregnant, which means this new child will be born in the middle of a global pandemic.
This adds one more job to Dr. Presseau’s portfolio, which also includes Scientist at the Ottawa Hospital Research Institute, Associate Professor in the School of Epidemiology and Public Health and in the School of Psychology at the University of Ottawa, and the Chair of the Health Psychology and Behavioural Medicine Section of the CPA.
As with many researchers, much of Dr. Presseau’s work had to pivot because of the pandemic. He leads a team co-developing new ways to support new Canadians with diabetes to be comfortable taking an eye test. Retinopathy is a manageable issue for people with diabetes when identified through regular screening but attendance rates could be improved, and so Dr. Presseau and his team are building relationships with different communities and community health centres virtually.
Another thing that’s difficult to do from a distance is blood donation. Dr. Presseau and his team are working with Canadian Blood Services and local communities to develop approaches to support men who have sex with men who may want to donate blood plasma, as screening and deferral policies continue to change to allow more MSM to donate if they want. Part of that work involves addressing the historic inequities that led to the exclusion of these men in the first place. But then – there was a pandemic, and his team like so many others have pivoted to continuing to develop key community relationships and campaigns virtually.
In addition, Dr. Presseau is tackling a lot of COVID-related projects, like for example a national survey of to understand what factors are associated with touching eyes, nose and mouth. The research is changing as we continue to develop an understanding of how COVID-19 is transmitted.
Maybe the most important of these COVID-related projects is the , a group of behavioural science experts and public health leaders who summarize behavioural science evidence in the context of COVID-19 and identify actionable guidance for Ontario’s pandemic response. Dr. Presseau is the co-Chair of this working group, which also involves CPA President Dr. Kim Corace.
“We sit within the larger Ontario Science Advisory Table. We’ve brought together expertise in behavioural science and particularly psychologists across Ontario, based both in academia and within government, to work alongside public health experts and ministry representatives.”
Dr. Presseau says that because the working group contains representatives from all these different areas and the team can communicate directly in this setting with decision makers and policy creators, it is the most direct form of knowledge transfer and knowledge mobilization of behavioural science in which he has been involved in his career.
“From an impact perspective, we get to translate our science to people who can make use of it right away, and they can also provide feedback to us – what are they looking for? What’s helpful to them? Of all the things I’ve done in my career this feels among the most impactful. One of the hats I also wear in the hospital where I’m based is Scientific Lead for Knowledge Translation [in the Ottawa Methods Centre], so I think about knowledge translation a lot. The ability to connect directly with those in the field that are making a difference is excellent. It’s also such a validating experience for me, as a behavioural scientist and a psychologist, to see that there’s recognition of our science and a need for an understanding of how we can draw from the behavioural sciences to support Ontarians and Canadians.”
The Behavioural Science Working Group is currently focused on vaccine confidence and uptake among health care professionals. Over 80% of Ontario health care workers say overwhelmingly that they intend to receive a COVID-19 vaccine when it is available to them. The working group is looking to communicate behavioural science approaches to support healthcare organisations across the province to optimise their vaccine promotion programs – for instance, by clarifying that despite having been created at record speed, these vaccines have been shown to be safe and effective and it’s important that those in the healthcare field get one.
Part of this is modeling good behaviour for the rest of the population. And within the healthcare field, modeling good behaviour is one way the working group is hoping to reach those who may be undecided. It’s one thing to have politicians and celebrities get vaccinated publicly, it’s another far more effective thing for your peer group, and hospital CEOs, and team leaders, to do so in front of your team.
Much of this work involves drawing on the literature from around the world to inform hospital policy or public policy. But some of it happens directly, and goes in two directions. For example,
“Our co-chair Dr. Laura Desveaux and her team did surveys with healthcare workers that not only ask if they intend to get the COVID vaccine, but also ask questions that are drawing from behavioural science and psychological principles around the specific constructs or factors might be associated with greater or lesser intention. So they were able to identify key predictors in healthcare workers in January of 2021, the most current data we have. So it’s kind of exciting to be able to quickly draw from on-the-ground data, iterate principles, and push that out to the field to support those who are doing this.”
We have asked most of our Psychology Month participants if they see a ‘silver lining’ in the pandemic. Something that is good, but that would not otherwise have happened absent the pandemic. Dr. Presseau says one silver lining is that it has highlighted just how important and relevant health psychology and behavioural medicine are to understanding and supporting health behaviour change and health and well-being during pandemics.
“After all, behaviour underpins most if not all the public health measures and vaccination activities that are key to seeing the other side of this pandemic.”
When Leigh and Justin’s baby is born, the pandemic will still be ongoing. But that baby will be born into a world that has a much greater understanding of pandemic science, of the behavioural science that accompanies it, and with more and more diverse teams of interdisciplinary experts working together to solve problems – locally, provincially, nationally, and globally.
One day, this baby will grow into a person who can take pride that Dad had a lot to do with that.
 Silver Linings in the Pandemic
Silver Linings in the PandemicPsychology Month has focused on dozens of aspects of the pandemic, a global catastrophe that is deeply tragic. To close out Psychology Month, we focus on a few positives that have come about as a result of COVID-19.
Silver Linings in the Pandemic
It has been a tough year for everyone, and so Psychology Month this year has been tough as well. No matter how many innovative, creative, dedicated psychologists are doing incredible things, it’s tough to forget the reason why. A pandemic that has ravaged the globe, caused untold economic damage, mental health issues, and more. Above all, we can’t forget the two and a half million people who have died as a result, which makes the subject of this year’s Psychology Month deeply tragic.
It is for this reason that we want to end on a high note, in as much as such a thing is possible. We asked many of the psychologists who were profiled for Psychology Month to tell us something good they saw come of the pandemic. A personal or professional observation of a way things had improved despite the global catastrophe. Here is what many of them had to say:
“Across hundreds of universities, dozens of countries, many languages, many disciplines, from the virologists to the immunologists to the mental health practitioners – all these people are working together over months. And doing this work under pandemic conditions, doing this work in labs that themselves could cause a super-spreader event. It’s an amazing human accomplishment that we’re already talking about how to get it under control.”
- Andrew Ryder
“One thing that amazed me was how quickly our field – psychology – was able to pivot to online services and mostly remote delivery of therapy when beforehand it was more of an exception to the rule to see people online or over the phone. Seeing that in-person visits can sometimes be adequately replicated via Zoom, or the phone, or other technologies, has been a really interesting experience for me as a trainee.”
- Chelsea Moran
“It wasn’t on the radar at all to offer virtual group psychotherapy for chronic pain, or for psychologists to have virtual appointments. The way Quebec is set up, we cover people who live seven, eight hours away from our centre. For them, being able to have weekly sessions with a psychologist is something that’s very precious. And for others in chronic pain where even thirty or forty minutes driving in the car to the hospital brings their pain level from a three to an eight, not having to come in on some days can be helpful as well. It’s a door that opened that wouldn’t have opened as fast had it not been for the pandemic.”
- Gabrielle Pagé
“There are certain people who, pre-pandemic, were super-productive and making amazing contributions at work. But because they weren’t bragging, and because they weren’t charismatic, they didn’t get the attention of their bosses and they were kind of overlooked. But now when everyone’s at home, it’s easier to track who’s contributing stuff, who is sending in work product. So all the ‘do-ers’ are getting their chance to shine.”
- Helen Ofosu
“I think the move toward virtual care is something that many many patients find very positive. In the capacity that they’re able to receive care from their home, rather than having to work to get themselves or their children or their family over to the hospital. Parking, and having to sit in a waiting room to come to your appointment – to know that you can do it from home is a huge advantage for a number of patients. This has really pushed us to advance in this area that is a real advantage for many of our patients.”
- Ian Nicholson
“For me, it’s being able to spend time on things I really enjoy. I really like to bake, and I really like to read non-academic books. I love murder mysteries! Being able to give yourself permission to actually engage in the activities that you enjoy, that are non-work-related, that are just for you, to me has been my silver lining.”
- Joanna Pozzulo
“Now that the pandemic has gone on for a long time, I don’t really miss the things like international travel – those were perks. But the things I do miss are seeing my family more, my friends more. Some of these things were clarifying, that the things I thought I was missing were perks but not necessary. As soon as I started giving up on my expectations and the things I was missing, it became easier to deal with them, and easier to reach out to other people for connection.”
- Vina Goghari
We also asked our members to point out some ‘silver linings’ in a poll question we included in our monthly newsletter. Here are some highlights of the responses we received:
“The involuntary aspect for many people to slow down as they were laid off or take time to quarantine and are forced to take time off from vacations and traveling is an opportunity to reflect on goals, and "reset" intentions coming out of the pandemic.”
- Charlene F.
“I have seen increased accessibility to services for people with disabilities.”
“I have seen distance barriers disappear - people are able to access learning, support, and other services virtually no matter where they are (assuming they have access to reliable internet!).”
- Gillian S.
“One positive thing for me was that I left my office and started to work virtually from home. It is much easier for me not to have to drive and find parking, and I don’t have to pay rent. The clients are really happy with that option, too, because it is a lot easier for them not to have to take a half day off work to come to the office.”
- Sharon Z.
“More people enjoying the great outdoors!”
- Julie B.
“One positive thing that I have seen come out of the COVID-19 pandemic is an increased societal focus on the importance of both mental health and social justice.”
- Danial A.
“I'm a third-year undergraduate psychology student at Ryerson. I've really been struggling with adjusting to an online semester, work from home, and volunteering and researching from home. This time has really challenged my mental health, but something positive that has come out of this pandemic is that for the first time in my life I am actually putting my mental health first and prioritizing my own wellbeing. I think I'll come out of this pandemic with so much self-growth, and I truly believe if I did not have so much time alone with my own thoughts, I would not have gone through this self-care journey.”
- Giselle F.
“I have noticed that staying at home has increased my focus on family life. Learning new and fun activities to keep the family busy while staying away from everyone we used to visit. For example, we have discovered new trails in our local area which is difficult because we are already active hikers so know most of the trails. Also, we have taken up painting rocks and searching for others' painted rocks on the more common trails.
As a student I have noticed a high increase of togetherness among students. There is a massive use of discord in the psychology department at VIU. This has helped to stay on top of school work and have discussions about our projects or simply to figure out how to get onto the zoom link the teacher put in a funny spot we can't find. Also on the psychology discord site, students are looking at common interests like gaming that they can do together and discussing various interesting novels that they enjoy.
I have never felt so connected to other students while walking around campus. Now I can log on and ask about test topics or paper ideas.
It's been tough distancing from everywhere, but I realize family life is the most important thing in my world and will not disappear from my life. School is a long term goal and I know one day I will be done with it, COVID is just a bump in the road.”
- Donna S.
“The pandemic has been grounding in the sense that many people have suddenly recognized and remembered the most important aspects of life. When faced with a universal threat to health and livelihood, the superficial details of a day become recognized as such, and the aspects with the most weight and meaning to our lives become clear.”
- Kathryn L.F.
“I believe that this pandemic has taught most individuals the importance of well-being. Seeing as we are no longer under the extreme pressures of traveling from day to day events, we now have more time for self-reflection, personal examination, questioning, and learning. It takes a certain level of resilience to shift perspective from uncertainty and anxiety to gratitude. However, with the pandemic disrupting what we knew as our normal lives and continuing to do so, those who are fortunate enough have been able to embrace this shift. Despite what may be happening in the world the most important thing we can focus on and should focus on moving forward is our overall well-being.”
- Emily T.
“A personal silver lining of the pandemic was having the time to finish my research and apply for residency a year earlier than anticipated. I also had more time to spend with my fiancée since both of us were working from home.”
- Flint S.
“More slowing down. A chance for children to play and be.”
- Jen T.
“Something positive I have seen from the pandemic is a newfound appreciation for in-person interactions, particularly in the younger generations. With so much screen time and so little face to face interaction, not only is in-person socializing of higher value, it’s become higher quality. I’ve noticed people are more likely to put their phones away and live in the moment. Interactions are limited, and we need to make the most of what we get. In my own life and for many of my friends, family, and classmates, it’s been something we’ve come to stop taking for granted.”
- Genevieve J.
“Psychologists being forced to become familiar with providing telehealth services, and the increased access that has provided.”
- Janine H.
“Nonobstant la dure réalité de la pandémie, beaucoup de réalités positives ont émergées. En premier lieu, l’esprit d’entraide et communautaire. Deuxièmement, la créativité, que ce soit dans toutes les formes d’art en tant que telles, mais aussi dans l’adaptation, la réinvention et la recherche de solutions. Troisièmement, toutes les nouvelles habitudes acquises, que ce soit le jardinage, l’exercice, l’apprentissage d’une langue, d’un instrument de musique ou d’une habileté ou encore de connaissances en général. Pour ce qui est de la psychologie, en particulier, la création de portails sécuritaires pour offrir des services en ligne.”
- Elisabeth J.
“Something positive in the pandemic- people have slowed down and reassessed their priorities, needs, and desires.”
- Heather P.
“The negatives from a global pandemic have been catastrophic. The most damaging effects being the crippling of the economy, deaths of millions of loved ones world wide, and an extreme toll taken on people's mental health in so many different ways. Keeping children away from school and their friends, forcing families to remain in abusive situations under the radar, allowing small business's to close down permanently day by day... this damage will take years to repair, and maybe won't be repairable at all.
This cannot be forgotten; however, in order to keep my head above the waters of these unforgettable events, I choose to remain optimistic and seek the positive in a sea of negative.
I remind myself that I have been given a chance to spend quality time with the most important person in my life - myself. People tend to neglect themselves daily, and I believe this pandemic has allowed us to check in with ourselves and take the time to look after our needs and self care. I also think that we often neglect the loved ones in our life. This time of isolation has encouraged me to pick up the phone and call people that I have not spoken to in a long time. I have called my parents more than ever before. I even call my friends instead of just sending them silly photos back and forth on Instagram. These conversations are meaningful. When we are allowed windows of social gathering, these windows are so meaningful also.
Besides these main points, I think that there are some little positive outcomes as well such as cooking more meals at home that are healthier for our bodies and mind, spending more time in nature and trying new activities we never would have tried otherwise, and of course, saving money if you are lucky enough to keep your job.
Negativity will drown you if you let it and positivity will keep you afloat. “
- Sacha H.
“Since COVID, I have become closer with my roommates. We spend more time together instead of doing our own thing all the time.”
- Laura J.
“1] a lot of children may be spending less time on screens by going outside tobogganing, building snow forts, and snowmen.
2] parents are actually spending more time with their children that they did before such as helping and supervising homework but also playing like colouring together and even playing non-screen table games like the good old days, monopoly, snakes and ladders etc.
3] couples like myself with my wife spend more time having coffee together and talking about all things which there may not have been time for before when people ran off to work for the entire day.”
- Jack A.
“I work in education, and I see teachers paying more attention to their own mental health. We bend over backwards for the kids we work with, but it is rare for a teacher to step back and say "I am not okay", and I have seen more of that this year than ever before. They are getting the help they need and taking time off to rest and heal. I hope this continues as teacher burnout is a real thing.”
- Danielle F.
Thank you to everyone who followed along with Psychology Month in 2021. This past year has been difficult, and it has been hard to put into words. Thankfully, there are psychologists all over Canada willing to try. We salute them all, and we salute the resilience of Canadians who have weathered this storm with diplomacy and aplomb. Take care of yourselves, and those around you.

Psychology Month has focused on dozens of aspects of the pandemic, a global catastrophe that is deeply tragic. To close out Psychology Month 2021, we focus on a few positives that have come about as a result of COVID-19.
 Dr. Karen Cohen
Dr. Karen CohenThe CPA has been adjusting, like everyone else, to working from home and embracing the new normal. Our work has been guided by our CEO, Dr. Karen Cohen.
CPA’s Communications Specialist, Eric Bollman talks to CPA’s CEO, Karen Cohen
“The tail of COVID is going to be a long one. It’s going to be psychosocial, and financial. Long after we get vaccines, long after we achieve population immunity, we’re still going to be addressing the psychosocial and financial impacts of living through a pandemic this long.”
Shortly after the NBA announced the suspension of their season on March 11, 2020, there was an all-staff meeting at the CPA head office in downtown Ottawa. The realization was dawning on everyone, and fast, that we were about to enter a different world – both in terms of our own work lives, and in terms of the role of psychology in the world at large.
We knew things were changing – if the NBA could shut down, the rest of the world was not far behind. We knew we’d all be sent home, and we spent that meeting discussing how that would work. Who needed a laptop? Who needed a refresher on Microsoft Teams, having slept through the training session less than a week before? What we did not know was that this would be the last time we saw each other in person for more than a year.
Our CEO, Dr. Karen Cohen, does not follow basketball. For her, the realization was more incremental. But she reached it at the same time, if not a little before, the rest of us. She made the decision to shut down the office and send everybody home.
“We were trying to make the decision that not only would best take care of our workplace, but that would make us a good corporate citizen. It was clear that if the world was going to be successful in managing the pandemic, we had to put in a community effort. “
As the world changed, and the CPA started working from our homes across Ottawa and connecting with people across the country, we realized that psychology was going to have an outsized role to play in helping people and communities manage the pandemic. CPA wanted to help in that effort. Dr. Cohen credits the staff at the CPA for making this transition work, almost seamlessly.
“Everything CPA has been able to contribute to managing the pandemic is to the credit of the association’s leadership, its membership and its staff. From the outset, our goal was to listen and respond to what people needed; what staff needed to work efficiently from home, what individuals and families needed to support each other, what members needed to face disruptions in their work, and what decision-makers needed to develop policies to help communities.
At first though, those lockdowns were not extended – we truly thought we’d be back at work in a few weeks, maybe a couple of months. Karen and the rest of the management team made sure to check in, and to cover their bases early on.
“One of the things we did at the outset was to survey staff – asking what’s keeping you up at night? How can we make things better? What are you most concerned about? And not just to ask the questions but to try to do something about them. We developed policies and made decisions that considered the things staff were worried about and responded to what they needed. We realized that psychology had some tools and suggestions to help them cope so we developed a webinar for staff on coping and resilience. We also reached out to staff one on one and really tried to hear them so we could help make things easier for them.”
We then thought that the survey and webinar might be helpful to the staff of other of CPA’s not for profit association partners and we delivered them to about a dozen of them. The survey enabled leaders to better understand the needs of their workplaces and psychology had some tools and suggestions to help workers cope. Something that was created internally, for the use of our own staff, ended up being of value to other organizations and an unforeseen contribution our team has been able to make.
While we didn’t know how long the pandemic would last, or what the long-term effects would be, the one group we knew for sure would be affected long-term were frontline health care workers. We were already seeing reports from Italy and Spain of overflowing hospitals, a health care system in crisis, and doctors and nurses overcome with exhaustion and despair. So what could we do?
The first major effort of the CPA during the pandemic was to ask our practitioner members if they would be willing to offer their services to frontline healthcare workers, on an urgent basis, as they faced the stressors of delivering health care services during a pandemic. It seemed essential that the people who were out there fighting against this scourge of a virus had every support possible as they took care of everyone else and, because of their work, faced heightened risk of contracting the virus and bringing it home to their families.
“Hundreds of psychologists came together to do that. It was good for CPA, it was good for psychology, and most importantly, it has been good for the health providers psychologists helped.
From there, it was a question of developing and delivering information, and getting as much of it out to members, decision-makers and Canadians as possible. Psychologists across Canada answered the call to help create more than a dozen COVID-specific fact sheets for students, psychologists, faculty, people working from home and more. Our team developed webinars, started a podcast, and undertook the herculean effort of moving the CPA annual convention online with just a few months notice.
The CPA team has been collaborating with innumerable other organizations and agencies, commissioning surveys and public opinion polls, and advocating for mental health to be front and centre in every governmental pandemic-related decision and policy across Canada. The work is ongoing, and it is not likely to stop any time soon.
“We know that rates of anxiety, depression and substance use have gone up as people cope with this prolonged chronic stressor. We can see the impact managing the pandemic has had on our work, relationships, and wellbeing. Maybe the pandemic has shown us that a pandemic takes as much of a psychological toll on our lives as a biological one. Maybe the pandemic has shown us that managing a critical health event successfully is as much about psychological and social factors as it is about the biological ones. Maybe, governments, workplaces, and insurers will fully realize that mental health matters and that it is time that making investments in mental health care matters too.”
 Dr. Jenn, Dr. Laila, and Dr. Mary
Dr. Jenn, Dr. Laila, and Dr. MaryFriends since they did an internship together at the Children’s Hospital of Eastern Ontario, child psychologists Dr. Laila Din Osmun, Dr. Mary Simmering McDonald, and Dr. Jenn Vriend are trying to reach as many kids and parents as they can during the pandemic with the Coping Toolbox podcast.
Laila Din Osmun, Jenn Vriend, and Mary Simmering McDonald
Everyone is swamped. Kids, learning virtually for the past year and dealing with constant uncertainty. Parents, looking after those kids and trying to work remotely or cope with being out of work. Psychologists, whose services are more in demand than ever but who don’t have any spots available for new clients.

Dr. Laila Din Osmun is a parent and a psychologist, dealing with two young children learning from home and an increasing demand for her professional services. She started spending time with her two children, aged five and seven, throughout the week and moved her practice to the weekends. She found she was turning people away because she just didn’t have the availability to see the number of people seeking services. And so she did something that may seem illogical – she added a whole other project to her workload.
In conversation with her friends Dr. Jenn Vriend and Dr. Mary Simmering McDonald, Dr. Din Osmun found that they were experiencing the same thing. The three had become friends during an internship at the Children’s Hospital of Eastern Ontario (CHEO), and now all three were child psychologists in private practice in Ottawa. None of them could keep up with the demand.

How do you get essential information to as many people as possible as quickly as possible? Nothing can replace one-on-one therapy, but there was clearly a void as the supply was not coming close to matching the demand. Dr. Din Osmun proposed a podcast. Coping techniques for kids, delivered one episode at a time, coupled with discussions of the issues facing families during the pandemic and some personal stories about spending time at home with their own children.
The CopingToolbox: A Child Psych Podcast was born. The first episode was published February 17th, discussing specific coping strategies (setting boundaries, practicing gratitude) for children and parents during COVID.

“Everybody’s feeling overwhelmed right now, myself included. My friends, my clients – it’s a really difficult time. One of the things I’ve been practicing is just allowing myself to feel some of those feelings. Sometimes we feel sad and we don’t want to, or we feel anxiety and we don’t want to. But it’s a really difficult time and we’re going through a lot, and I think it’s really important that we allow ourselves to feel that feeling for a little while.”
Jenn Vriend, The Coping Toolbox Episode One
Future episodes will deal with subjects like depression, as the three friends try to bring more services to more people through a new and interesting platform. On the podcast, they refer to themselves as ‘Dr. Laila’, and ‘Dr. Jenn’, and ‘Dr. Mary’. To an outsider, this might remind people of the ‘Dr. Bobby’ episode of Friends (okay it’s me – I’m the outsider who was reminded of that episode) but it also creates a friendly and welcoming atmosphere should kids be listening with their parents. This was clearly an intentional choice, as was the use of the word ‘toolbox’. Says Dr. Laila,
“We called it The Coping Toolbox because we wanted to provide tools for coping. Not getting into too much detail, and we wanted it to be useful. At the end of every podcast we give three coping skills that we review for the people listening.”
In episode one, those skills are; take a few minutes and breathe, modeling positive behaviours for your kids, and being kind to ourselves. On the podcast, Dr. Jenn says;
“We’re modeling positive behaviours, but we’re not doing it perfectly. So we can take a deep breath, do our best to model those positive behaviours, for ourselves as well as our kids, and then just be gentle and kind to ourselves knowing that we’re doing the best we can given the situation.”
All three Coping Toolbox podcast co-hosts know about doing their best given the situation. They all have young children at home, and each of them brings a different perspective. While Dr. Din Osmun has set aside a large portion of her work to take care of the kids while her husband works a demanding job, Dr. Simmering McDonald, a mom of 3- and 5-year-old boys, is balancing her clinical practice with her husband’s long work days, limited childcare, and weekly appointments regarding the health needs of family members.
In The Coping Toolbox Episode One, Dr. Simmering McDonald notes, “it’s important to consider our own well-being and our own mental health. This is necessary for our own functioning but also for the functioning of our kids and our families.” Dr. Vriend speaks about grief, something many people are experiencing with COVID-19. She separated from her son’s father a few years ago, then sadly he passed away in the summer of 2020. “I’ve had to learn not just single parenting but lone parenting, where you’re it – you’re kind of the everything. I think that perspective, during the pandemic, is going to be interesting to discuss. I remember at one point feeling like ‘I’m my son’s entire world’. I’m his teacher, and I’m his coach, and I’m his mom, and I’m his dad, and it felt very overwhelming. It can add a different perspective because there are a lot of people who discuss both parents, and when you’re a single parent it can hurt a little bit and I think the pandemic has created a whole other layer for single parents and for lone parents.”
In professional practice, divulging personal details is not something psychologists do. But in the context of a podcast, doing so can help the narrative hit home – a narrative that, in the case of The Coping Toolbox, is warm, friendly, expert-driven and truly helpful for many who can’t access that help in other ways at the moment. Dr. Din Osmun says,
“It’s been a crazy time, and we just can’t meet the demands right now. It was getting really frustrating, and the three of us kept talking in group conversations – how can we help? We’re so limited in what we can do. We had the idea of creating a podcast, but we knew nothing about podcasting. The three of us are clinicians in private practice, we have no expertise in podcasting whatsoever. It was a huge learning curve, but we figured this IS something we can do to help people because it’s something the three of us can do from home. We felt like this was a way to help more people in a shorter period of time.”
Laila has taken the lead on the podcast, including taking on hosting duties and – the most painstaking and time-consuming job of all – the editing after the fact. It will all be worthwhile if enough people listen and take away something helpful they did not already know.
You can find The Coping Toolbox: A Child Psych Podcast on Apple Podcasts. https://podcasts.apple.com/ca/podcast/the-coping-toolbox-a-child-psych-podcast/id1553993639

Introducing The Coping Toolbox: A Child Psych Podcast. Dr. Jenn Vriend, Dr. Laila Din Osmun, and Dr. Mary Simmering McDonald are three child psychologists from Ottawa.
https://podcasts.apple.com/ca/podcast/the-coping-toolbox-a-child-psych-podcast/id1553993639
 Charles Henry Turner
Charles Henry TurnerCharles Henry Turner was a zoologist, one of the first 3 Black men to earn a PhD from Chicago University. Despite being denied access to laboratories, research libraries, and more, his extensive research was part of a movement that became the field of comparative psychology.
Dr. Turner was a civil rights advocate in St. Louis, publishing papers on the subject beginning in 1897. He suggested education as the best means of combatting racism, and believed in what would now be called a ‘comparative psychology’ approach.
Charles Henry Turner was a zoologist, one of the first 3 Black men to earn a PhD from Chicago University. He became the first person to determine insects can distinguish pitch. He also determined that social insects, like cockroaches, can learn by trial and error.
Despite an impressive academic record, Dr. Turner was unable to find work at major American universities. He published dozens of papers, including three in the journal 'Science', while working as a high school science teacher in St. Louis.
Despite being denied access to laboratories, research libraries, and more, his extensive research was part of a movement that became the field of comparative psychology.
Dr. Turner was a civil rights advocate in St. Louis, publishing papers on the subject beginning in 1897. He suggested education as the best means of combatting racism, and believed in what would now be called a 'comparative psychology' approach. He retired from teaching in 1922, and died at the age of 56 on Valentine's Day in 1923.
Photo: biography.com
 Penny Corkum
Penny CorkumDr. Penny Corkum studies sleep and children, and created Better Nights Better Days, a cross-Canada trial that improved sleep for both kids and parents before the pandemic. In the last year, Dr. Corkum and her team went back to those families to see how they were doing during COVID. Their launch of a revamped Better Nights Better Days for the pandemic era is imminent.
“When we launched our survey study asking parents during the pandemic how their child’s sleep was impacting them, what really came up was that it’s the whole family and not just the child. So we not only had to help the child sleep better but also give strategies for the parent to sleep better. So we added that into the intervention as well.”
It probably goes without saying that sleep is incredibly important for children. Difficulty falling asleep and staying asleep can have a big impact on a child, in terms of daytime functioning. They’re not able to focus or learn as well, and it might result in behavioural problems. Dr. Penny Corkum has been studying sleep in children for a long time. In the last decade, her sleep studies have taken the form of connecting parents and families with the interventions they now know work for children and sleep. Part of this is an e-health program, online tools that parents can access when they need them.
Between 2016 and 2018 Dr. Corkum and her team ran a cross-Canada trial called Better Nights, Better Days, to see if this program was effective. It was, and the program resulted in improved sleep, improved daytime functioning, and even parents were less tired during the day as a result. Then the pandemic hit, and it became a constantly evolving crisis – lockdown for a while, then lockdown lifted. School online from home then back to in-person classroom learning. Right away, sleep patterns were disrupted for both children and adults around the world.
The team went back to the families who had participated in the original Better Nights, Better Days trial, to see how they were doing during the pandemic.
“It seemed like a good place to start because we already knew about their sleep, and we knew that they had learned a lot of strategies to help their child sleep. We were curious – were they still using these strategies? There was some research coming out at the time that suggested families were actually having better sleep, since they didn’t have to get up at a certain time. But that’s not what we found. A small portion of our families were doing better, but about 40% of the children and 60% of the parents were sleeping worse than they were before the pandemic.”
A lot of this was happening because of disruptions in routine and structure. We sleep best when we have consistency in our days – a regular bedtime, a regular time to wake up, a standard time for supper. All of this was being upended by a constantly evolving pandemic and the restrictions that went along with it. Two of the biggest factors were anxiety as a result of worry about the pandemic, and screen time. Kids were using screens a lot more while locked down at home which was disrupting their sleep in a big way.
With new data collected from the Better Nights, Better Days cohort, Dr. Corkum and her team could move forward. Almost all the parents said they were still using the interventions they had used for sleep pre-pandemic. 95% of them said that they thought other families should have access to these strategies during the pandemic. Based on this, the Better Nights, Better Days team was able to get some funding to launch an intervention for all families during the pandemic.
That new program launches Very soon – hopefully very early in March. It is free for families to use, intended for parents of children ages 1-10 who are struggling with falling asleep and staying asleep. There have been slight modifications, now that Dr. Corkum and her team have information about the pandemic and how it impacts sleep. They’ve also added to the intervention some information about parents’ sleep, and how to help parents sleep better. Sleep is essential for the whole family!
Dr. Corkum also runs a diagnostic clinic in Truro, Nova Scotia that brings together pediatricians, school psychologists, health psychologists and others to do differential diagnostics for kids who have fairly complex presentations and need a comprehensive assessment. Well, she normally does. But in the past year the doors have remained closed because they just can’t have all those people together in one room. It’s disappointing for Dr. Corkum and her team, who likely won’t be able to re-open until next year. Therapy can be done virtually, diagnostic assessments not so much.
Dr. Corkum says she misses working at Dalhousie and seeing her students, staff and colleagues but doesn’t miss the walk! Her parking spot is far from the office that carrying a bag, and papers, and a laptop through deep snow or a blizzard makes the walk to work something of a nightmare and a serious workout, every winter. She’s still getting the walk and the workout in – but walking a big dog three times a day is a much more pleasant experience.
Fresh air, exercise, and sleep are three of the things that can make life during the pandemic a more pleasant experience. And with the launch of Better Nights, Better Days which has been modified for the COVID-19 context, Dr. Corkum is making at least one of those things easier and more accessible as of today.
Some of Dr. Corkum’s current studies:
Pediatric Sleep Knowledge, Attitudes, and Beliefs
Did you know that there are no well-developed, validated measures to assess healthcare providers’ pediatric sleep knowledge, attitudes, and beliefs? Help us develop one by testing your pediatric sleep knowledge today!
This study will involve completing a survey about your pediatric sleep knowledge, attitudes, and beliefs at two time points. It should take about 15 minutes to participate at each timepoint. Once you finish the survey, you will be contacted again in one month to complete the survey again. After completing the survey for a second time, you will receive the correct answers, as well as access to the first version of the Promoting Healthy Sleep for Early Childhood online training program for healthcare providers, once it has been developed.
To be eligible for this study, individuals must:
- Be a licensed healthcare provider practicing in Canada (e.g., physician, psychologist, nurse, or other allied health professional)
- Have current clinical experience working with young children (under the age of 5 years) at least some of the time
If you are interested in participating, please follow the link below to review and complete a Screening Questionnaire to determine your eligibility: https://redcap.its.dal.ca/surveys/?s=AXENE3YXNA9DCM4L
Develop and Validate the Insomnia Knowledge, Attitudes, Beliefs, and Practices (iKAB-P) Questionnaire
You are invited to participate in a sleep expert panel to assess the content validity of the initial draft of the iKAB-P questionnaire for adults aged 18-64 years old. Please also share this invitation to anyone who you think may be interested in participating!
As a part of the development and validation of the questionnaire, we are requesting your expertise to estimate the content validity of the draft. This is an exciting study as there are currently no validated KAB-P tools for insomnia for Canadian adults!
The inclusion criteria to be eligible to be apart of the sleep expert panel includes:
- Currently live and work in Canada
- Experts who have 3+ years' experience in working with adults with insomnia/insomnia symptoms. Experts include academics (i.e., clinical or research appointment at a university) and healthcare providers who assess and/or treat patients with insomnia
- Those who have expertise in the development and validation of any aspect of sleep measures (i.e., published peer-reviewed development and validation studies)
- Experts who have at least five years’ experience in working with adults with insomnia/insomnia symptoms
If you are interested in learning more, please go to https://redcap.its.dal.ca/surveys/?s=FXT3W8WPYAYCLM44
“Najimpay”: Gathering Indigenous Adult Perspectives on Sleep through Interviews in Nova Scotia
Join us for an interview about sleep in Indigenous adults! We are conducting individual interviews, and we will as you questions about sleep, sleep habits, sleep challenges, and sleep education/intervention.
To be eligible for this study, individuals must:
- Live in Nova Scotia
- Be aged 20 years or older
- Identify as Indigenous
- Be able to communicate in English or Mi’kmaw
- Be associated with Membertou First Nation or the Mi’kmaw Native Friendship Centre (e.g., be a community member, user of services)
If you are interested in learning more, click the following link: https://redcap.its.dal.ca/surveys/?s=FFJXKK74WXJML3H7
